2019.04.03.13
Files > Volume 4 > Vol 4 No 3 2019
NEWS AND VIEWS /NOTICIAS Y OPINIONES
Stem cell activity in the repair of cardiovascular tissues

Alejandra Cevallos and Abigail Solórzano
Available from: http://dx.doi.org/10.21931/RB/2019.04.03.13
ABSTRACT
Stem cells can become different types of cells and have the potential to divide and self-renew. There are two types of stem cells, first the embryonic stem cells and second the adult stem cells, both help in regeneration or repair tissues of an organism, for this reason, the stem cells are being used to renew the world of medicine. Stem cells are obtained from three sources: the first can be our own body that where certain organs still have some cells still not completely differentiated. The second source is the embryos when they are in the blastocyst phase (between five to fourteen days from conception), and the third source can be in the cells of the skin, liver or another cell type that have been modified to behave like embryonic stem cells. With this therapy, we would find ourselves before an inexhaustible source to repair the tissues and organs that were damaged in our bodies. One of the main causes of mortality in heart failure, but with the help of cell therapy has been studied the repair of cardiac tissue with the stem cell transplant. The objective of the cellular transplantation is that the transplanted cells in the heart tissue manage to regenerate, renewed, and repair any part of the heart tissue damaged.
keywords: Stem cell, cardiomyocytes, hematopoietic cells, autologous, bone marrow
INTRODUCTION
One of the fields of medicine that has caused more expectation in recent years has been cell therapy with stem cells. Stem cells in our body have the ability to self-renew, allowing our organs to repair the damaged tissue. These cells can be classified into embryonic stem cells, obtained from the embryo, adult stem cells found in the tissues of the adult organism, and induced pluripotent stem cells (iPSC) are adult cells that have been rescheduled genetically, the three types of cells have the ability for self-renewal and differentiation themselves in any of the types of specialized cell. Stem cells can be obtained in the human body in certain organs, in embryos or in the cells of the skin, liver or another cell type that have been modified to behave like embryonic stem cells.
Heart failure has been one of the diseases with the highest mortality rate,1 it is for this reason that it has sought to thousands of treatments that help to avoid or reduce deaths from heart failure. Among the most effective treatments is the heart transplant, however, is one of the treatments that carry more risk for the patient because many times they have to wait for a heart for years and with a fairly restricted lifestyle. Besides, when it is going to perform the transplant , there is a risk of death during the surgery and after it because of the rejection that the body can suffer when receiving a foreign organ. In recent years it has been shown that the heart has cells with the ability to renew, therefore it has been proposed as a type of treatment cell therapy with cells from the same organism to decrease the range of rejection of the body.
Stem cells may be donated from the same patient (autologous transplants) or may be donated by another individual that is compatible with the human leukocyte antigen (allogeneic transplants). There are several ways to transplant stem cells, and they can be: 1. intravascular: by intravenous route or 2. It is injected directly into the cardiac muscle: by trans-epicardial route or by infusion intracoronary or by injection through the coronary veins. The field of regenerative medicine is very extensive and is still in the process to be a completely feasible method, and that can save lives not only from people with heart tissue damage but to any other area such as neurological diseases, pulmonary or hepatic.
STEM CELLS: Definition
Stem cells differ from other cells because they have two essential characteristics. First, these are cells with the capacity to auto-renew through cell division, but without being specialized. Second, to be cells not specialized can become any cell specifies of tissues or organs with special functions. They have the potential to divide, also in many tissues; they can regenerate to repair or replace other cells that have died while the person or animal is alive. There are two types of stem cells, "from their origin we divide the stem cells in embryonic (derived from the embryo either the blastocyst or the gonadal crest) and adults (derived from one of the tissues Adults) ".2
Embryonic stem cells
After 4 or 5 days of fertilization, the cells of the embryo have been divided, forming a new structure called blastocyst constituted with around 500 cells. Cells that form the blastocyst are responsible for giving rise to all cell types, systems, tissues, and organs of the individual that is beginning to form. Embryonic stem cells are found in the internal cell mass of the blastocyst, can divide continuously and then have the ability to differentiate to form any tissue of the organism. The characteristics of embryonic stem cells are the same as cancer cells, according to Aj & Science.3 Human embryonic stem cells (hESCs) share several characteristics with cancer cells, including upregulation of oncogene expression, increased proliferation, genomic instability, and elevated telomerase activity. For this reason, embryonic stem cells are used for the field of regenerative medicine, challenging researchers because they try to control cell differentiation to obtain any tissue or regenerate any organ.4
Adult stem cells
Adult stem cells are cells found in different tissues, but these cells are not differentiated. Adult stem cells in the body are used to repair the tissue in which they reside, fulfilling the two main functions of the embryonic stem cells can self-renew and can differentiate to produce the cell types of the tissue or organ. The functions are significantly lower than the embryonic cells; however, several studies have been achieved with adult stem cells because they also have a function of trans differentiation, "every time it seems more evident than adult stem cells are capable of generating mature cells from tissues derived from different embryonic layers. "2
In each tissue or organ of our body there is a small number of stem cells that allow the tissue to regenerate, but in a limited way, therefore, when these cells are lost the tissue loses the ability to repair. The investigation of adult stem cells has achieved to find this type of cells in the brain and heart and with this finding has been able to apply cell transplantation as a therapy to regenerate damaged tissue healing many diseases that are caused by tissue damage.
OBTAINING THE STEM CELLS
There are different types of stem cells, the same ones that can be obtained in different ways: Adult Stem Cells or specific can be found in our own body in certain organs although they are in small numbers. Embryonic stem cells as its name say it is found in embryos. These embryos can be donated voluntarily by different patients in fertility clinics. And induced pluripotent stem that is in the cells of the skin, liver, or another cell type that have been modified to behave like embryonic stem cells.
Embryonic stem cells are those that can be extracted from the embryos; these cells are pluripotent which means that they are not yet cells of a specific tissue or organ and it can be converted into any tissue or organ of the human body. These embryonic cells are often obtained from different fertility clinics where fertilized ovules are found from some in vitro fertilization technique from different donors. Embryonic cells should be extracted when the embryo has few days of its creation, i.e. it is in a state of the blastocyst. This blastocyst has two parts an outer layer of cells that formed the placenta and the internal cell mass (inner layer of cells) these are the non-specialized cells, and it is not differentiated yet. In this way, the internal cell mass must be extracted in a culture plate containing a nutrient-rich broth (culture medium).5
Adult stem cells are those undifferentiated cells that are among cells that if they are differentiated tissue or organ. The function of these cells is to maintain and repair the tissue they are in. The amount of these cells in the different organs is not very high, but through years of research has been finding more in different tissues and organs. As well as hematopoietic stem cells, these cells can be obtained from the bone marrow, blood or umbilical cord. In the case of bone marrow cells, they are obtained through punctures in both iliac crests (located in the hip bone); this procedure will be carried out under general anesthesia and lasts 2 to 3 hours.6 In the case of the extraction of stem cells in the peripheral blood should be initiated with the administration of a growth factor (approximately four days before extraction). This medicine helps stem cells leave the bone marrow to the blood, once the cells are in the blood is necessary to perform the apheresis (the process by which extract blood from the donor of a vein of the elbow). This blood is processed on a machine that separates the stem cells of the others and proceeds to return the remainder through another vein in the other arm. 7
Induced pluripotent stem cells (IPSC) are the adult cell that has been genetically reprogrammed, possessing pluripotent characteristics. These are derived from cells that initially were not pluripotent. Therefore, these cells can be obtained as adult stem cells.7
TISSUE DAMAGE IN THE CARDIOVASCULAR SYSTEM.
The heart is one of the first organs that are formed in the fetus, cells called cardiomyocytes to form the cardiac muscle and according to Nadal-Ginard,8 the cardiomyocytes are generated from a cell precursor that divides and gives rise to groups of cells of the same type. Cardiomyocytes are cells responsible for generating contraction and relaxation in the heart; in other words, they are responsible for the heartbeat.9 The cells of the muscle heart (cardiomyocytes) are cells with the potential to multiply during the development of the fetus until the human being comes to the 3 or 4 months of postnatal life, then it is assumed that the human being already has the maximum number of cardiomyocytes and from there lost cells will not recover or regenerate.8,10
Cardiovascular diseases are the diseases that cause most deaths in the world, "accounting for more than 17 million deaths every year and accounting for 31% of all global deaths".11 The World Health Organization claims that cardiovascular disease is due to heart and blood vessel disorders; one of the most important and most dangerous diseases is heart failure. Every year more people die because of this disease than any other, for this reason, thousands of treatments have been sought to reduce deaths, however, when treatments such as drugs or therapies do not work, the heart transplant is used.
Although the heart transplant seems to be the best treatment, it is also the riskiest during and after surgery. Also, Park and Yoon11 say “heart transplantation is currently the only definitive treatment; however, it is limited by lack of donors, potential graft rejections, and various side effects resulting from immunosuppression.” For this reason, other ways of repairing the patient's heart have been investigated without the need for a complete replacement, and a form has been therapy or cell transplantation.
The heart has the potential to regenerate their tissues, but in a limited way and depending on the speed of its degeneration, therefore, one of the best ways to help with the regeneration of muscle cardiac is transplanting stem cells from the same heart as cardiomyocytes or myoblasts (cells from the muscle-skeletal).
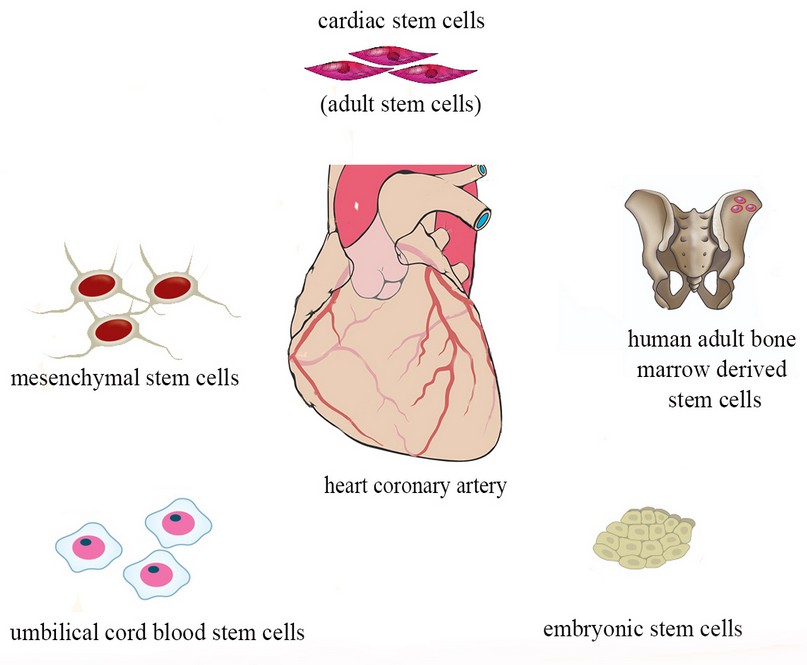
Figure 1. Types of stem cells used to repair cardiac tissue
HOW TRANSPLANTING THE STEM CELLS
Before talking about the ways to perform stem cell transplantation, it is necessary to mention the two types of bone marrow transplantation that can be found:
Autologous transplants: In these transplants, an individual donates his or her stem cells from his or her bone marrow to the treatment.12
Allogeneic transplants: Instead, in this transplant, the patient receives the stem cells from another person's bone marrow for treatment.12 Of course, this type of transplant has certain complications as the patient must find a donor with the compatible bone marrow. The patient should be compatible with the Human Leukocyte Antigen (HLA) because they are some specific proteins in white blood cells and other cells that make the type of tissues different in each. For this reason, a patient with a higher percentage about HLA will have a lower probability of the occurrence of side effects.13
There are several pathways for stem cell transplantation but first must select what type of stem cells are to be used in transplantation, can be embryonic, adult or pluripotent-induced stem cells. In this case, will explain the transplantation of hematopoietic stem cells obtained from the bone marrow. The pathways for this transplantation may be: intravascular or injected directly into the heart muscle.
1. Intravascular this can be performed by intravenous route.
The intravenous route:
This procedure is simple and consists of entering stem cells by an injection into the blood using a central venous catheter. The problem in this pathway lies in the fact that the stem cells entered can be directed toward other organs which reduce greatly the number of stem cells that should reach the myocardium and them join together to generate the regeneration. 6
2. Injected directly into the heart muscle.
This process is usually used in diseases such as cardiomyopathy, or coronary heart disease. This process can be done a trans-epicardial route or by infusion intracoronary or by injection through the coronary veins.
Trans-epicardial route:
In this process, stem cells are inserted directly in the myocardium (affected area and its edges). According Siminiak T, Fiszer D, Jerzykowska O: "In humans, this pathway has been used so far in conjunction with Revascularization surgery or bypass, or during the placement of a mechanical ventricular device."14 By this means the cells to enter directly to the affected area and will have more precision to make the process successful. However, this process has a small limitation because it can have risks in surgery and by the use of anesthesia. As a result, it is usually only performed to individuals who are going to have a revascularization surgery. 6
Intracoronary Infusion:
In this process the cells are inserted by an intracoronary catheter and depending on the exact area in which it was inserted, the cells will be distributed by the coronary vascular bed or placed in a specific area of the myocardium.6
Injection through coronary veins:
This method uses a catheter that has an ultrasound system placed at the tip of the catheter (this is used to guide the catheter) and an expandable needle through which the cells are inserted into the myocardium. The cells are injected more deeply in parallel to the ventricle wall. This process is still risky and complicated.6
CLINICAL TRIALS
In several experimental studies have been using different types of stem cells, in this clinical study was sought to identify what type of stem cell is most suitable for transplantation in cardiac diseases (Table 1).
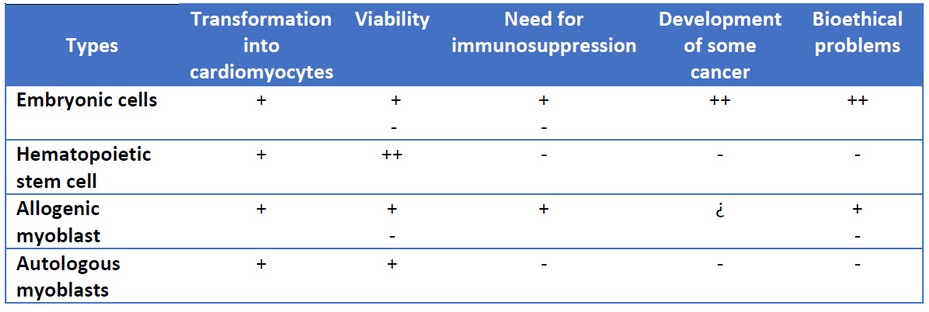
Table 1. Stem cells used in cardiac regeneration
Embryonic cells seem to be the most suitable because of their ability to differentiate. However, they face many ethical problems and in different studies are prone to be carcinogenic. According to Dorticós E and Hernández P: "It is known that in the bone marrow there is a very heterogeneous cellular population, although the various types of progenitor cells, as well as the mechanisms of control of their function and differentiation, are not yet well understood. Hematopoietic progenitors (CD34), endothelial precursors (CD 133), mesenchymal cells (stromal) (CD34-), others called a lateral population, and the multipotent adult progenitor cells (MAPC) are found. Therefore, of the different types of stem cells, those coming from the bone marrow seem to be, so far, those that have shown greater ability to differentiate towards cardiac muscle fibers or endothelial cells "6. For this reason, we have observed that stem cells obtained from bone marrow have been taken into account in several clinical trials in recent years.
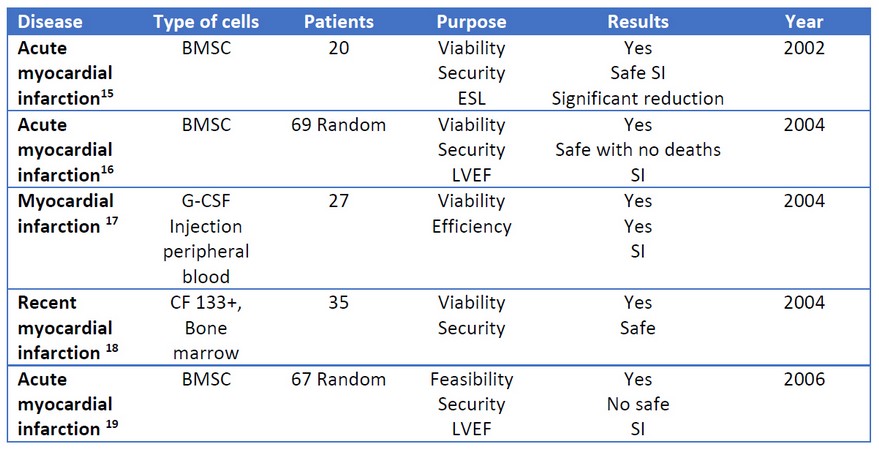
Table 2. Clinical studies with hematopoietic stem cells injected by infusion intracoronary. BMSC: bone marrow-derived stem cell; G-CSF: granulocyte-colony stimulating factor; ESL: end-systolic left; LVEF: Left ventricle ejection fraction; SI: Significant improvement.
In a clinical study performed on 55 patients with dilated cardiomyopathy, it was divided into two groups, 28 patients would have CD34+ transplantation, while 27 patients would not have transplantation with stem cells and would only serve as a control group. The two groups received granulocyte-colony stimulating factor (G-CSF) therapy, but only in the first group were collect cells CD34+ by a technique called apheresis, then patients in this group received intracoronary transplantation of autologous CD34+ cells. In both groups, the same evaluation parameters were taken like an increase in the left ventricular ejection fraction (LVEF), an increase in 6-minute walk distance and measured plasma levels of NT-proBNP. At the beginning of the clinical trial, all 55 patients had the same age, gender, left ventricular ejection fraction (LVEF), and NT-proBNP levels were the same. However, after one year of the study, the parameters of each group were evaluated and according to Vrtovec20 the following results were obtained: An increase in LVEF (from 25.5± 7.5% to 30.1± 6.7%), an increase in 6-minute walk distance (from 359± 104 m to 485± 127 m), and a decrease in NT-proBNP (from 2069± 1996 pg/mL to 1037± 950 pg/mL). Also during the clinical trial, it was possible to demonstrate the decrease in mortality in patients with stem cell transplantation, two patients died by cardiac failure which represents a percentage of 7%, in contrast in the control group died 8 patients; it means 30 % of 27 patients died. The clinical trial showed the autologous hematopoietic stem cell transplantation as a technique to improve the function of the left ventricle, thus improving the lifestyle of patients suffering from dilated cardiomyopathy.
CONCLUSION
The cellular self-renewal not only of the heart but of any organ will allow giving a turn to the medicine allowing advancement in the disciplines like the genetics and cellular biology. In advances in regenerative medicine, clinical trials have been conducted practically for all types of tissues and organs, but some of them without results. In cell therapy, stem cells are ones indicated to be transplanted by their ability to self-renew and differentiation, helping to generate new healthy cells and in this way to replace the damaged or dead tissue cells. There are three types of stem cells, embryonic stem cells, adult and pluripotent; however, transplantation of these cells entails ethical problems. Embryonic stem cells by obtaining them from the embryo cause more conflict with society.
On the other hand, with the adult stem cells and pluripotent does not pose any more problem than the informed consent of the person from which the cells are extracted. Of the different types of stem cells that we can obtain, the best is the adult stem cells specifically the hematopoietic stem cells obtained from the bone marrow since in several trials it has been seen that these cells differentiate into cells of the tissue damaged. One of the organs most studied for cell transplantation is the heart. The heart is an organ in a continuous process of death and renewal. Therefore the cultivation of stem cells of the own cardiac tissue as the cardiomyocytes represents an innovative form of treatment for heart failure. However, current studies on cell therapy applied to cardiac tissue, show a favorable differentiation towards cardiomyocytes when hematopoietic stem cells are obtained from the bone marrow.
REFERENCES
1. Trainini J, Cichero D, Cardiol NB-RA, 2002 undefined. Cardioimplante celular autólogo. SacOrgAr.
2. Prósper F, Gavira JJ, Herreros J, Rábago G, Luquin R, Moreno J, et al. Trasplante celular y terapia regenerativa con células madre Cell transplant and regenerative therapy with stem cells. An Sist Sanit Navar. 2006;29(2):219–34.
3. Aj B, Science B. Chapter 12: 2000;1869:127–42.
4. Castagnino JM. Células madre embrionarias. Acta bioquímica clínica Latinoam. 2005;39(3):277–8.
5. Rippon HJ, Bishop AE. Embryonic stem cells. Cell Prolif [Internet]. 2004 Feb [cited 2018 Nov 27];37(1):23–34. Available from: http://doi.wiley.com/10.1111/j.1365-2184.2004.00298.x
6. Centro Nacional de Información de Ciencias Médicas. E, Hernández Ramírez P. Revista cubana de hematología inmunología y hemoterapia. [Internet]. Vol. 22, Revista Cubana de Hematología, Inmunología y Hemoterapia. Centro Nacional de Información de Ciencias Medicas, Ministerio de Salud Publica; 2006 [cited 2018 Nov 27]. 0-0 p. Available from: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0864-02892006000100003
7. Herreros González J, Prósper Cardoso F, Alegría Ezquerra E. Utilización de células madre para la regeneración miocárdica en la insuficiencia cardíaca. Rev Española Cardiol [Internet]. 2003 Oct 1 [cited 2018 Nov 27];56(10):935–9. Available from: http://www.revespcardiol.org/cgi-bin/wdbcgi.exe/cardio/mrevista_cardio.fulltext?pident=13052378
8. Nadal-Ginard B. Inducción de nuevos cardiomiocitos en el corazón adulto : futuro de la regeneración miocárdica como alternativa al trasplante. Rev Española Cardiol. 2001;54(5):543–50.
9. Woodcock EA, Matkovich SJ. Cardiomyocytes structure, function and associated pathologies. Int J Biochem Cell Biol. 2005;37(9):1746–51.
10. Bigalli D, Bico Uribe JA, Gossio Landoni EE. Cardioimplante celular para reparar tejido cardiaco: un nuevo concepto terapeutico?^ies. Rev urug cardiol. 2005;20(3):158–70.
11. Park M, Yoon Y. Cardiac Regeneration with Human Pluripotent Stem Cell-Derived Cardiomyocytes. Korean Circ J. 2018;48(11):974.
12. Cuadros Celorrio M, Sarmiento González-Nieto V, Villegas Portero R. Células madre en pacientes cardíacos [Internet]. [cited 2018 Nov 27]. Available from: http://www.aetsa.org/download/publicaciones/antiguas/AETSA_2007-02-08_Celulas_Madre.pdf
13. Valdés Chavarri M, Pascual Figal D, Prósper Cardoso F, Moreno Montañés J, García Olmos D, Barcia Albacar JA. Medicina regenerativa con células madre adultas. Rev Clin Esp [Internet]. 2005;205(11):556–64. Available from: http://dx.doi.org/10.1016/S0014-2565(05)72638-2
14. Siminiak T, Fiszer D, Jerzykowska O. Percutánea trans-coronaria-venosa trasplante de autólogas esqueléticos mioblastos en el tratamiento de poste - infarto deterioro de la contractilidad miocárdica: la ... Eur Hear [Internet]. 2005 [cited 2018 Nov 27]; Available from: https://academic.oup.com/eurheartj/article-abstract/26/12/1188/524870
15. Assmus B, Schächinger V, Teupe C, Britten M, Lehmann R, Döbert N, et al. Transplantation of Progenitor Cells and Regeneration Enhancement in Acute Myocardial Infarction (TOPCARE-AMI). Circulation [Internet]. 2002 Dec 10 [cited 2018 Nov 27];106(24):3009–17. Available from: https://www.ahajournals.org/doi/10.1161/01.CIR.0000043246.74879.CD
16. Chen S, Fang W, Ye F, Liu Y, Qian J, … SS-TA journal of, et al. Effect on left ventricular function of intracoronary transplantation of autologous bone marrow mesenchymal stem cell in patients with acute myocardial infarction. Elsevier [Internet]. [cited 2018 Nov 27]; Available from: https://www.sciencedirect.com/science/article/pii/S0002914904004485
17. Kang H, Kim H, Zhang S, Park K, Lancet HC-T, 2004 U. Effects of intracoronary infusion of peripheral blood stem-cells mobilised with granulocyte-colony stimulating factor on left ventricular systolic function and restenosis. Elsevier [Internet]. [cited 2018 Nov 27]; Available from: https://www.sciencedirect.com/science/article/pii/S0140673604156894
18. De Bondt P, Van Haute I, Lootens N, Heyndrickx G, Wijns Jozef Bartunek W, Vanderheyden M, et al. Promotes Cardiac Recovery After Recent Myocardial Infarction: Feasibility and Safety Intracoronary Injection of CD133-Positive Enriched Bone Marrow Progenitor Cells. 2005 [cited 2018 Nov 27]; Available from: http://circ.ahajournals.org/content/112/9_suppl/I-178
19. Janssens S, Dubois C, Bogaert J, Lancet KT-T, 2006 U. Autologous bone marrow-derived stem-cell transfer in patients with ST-segment elevation myocardial infarction: double-blind, randomised controlled trial. Elsevier [Internet]. [cited 2018 Nov 27]; Available from: https://www.sciencedirect.com/science/article/pii/S0140673605678610
20. Vrtovec B, Poglajen G, Sever M, Lezaic L, Domanovic D, Cernelc P, et al. Effects of Intracoronary Stem Cell Transplantation in Patients With Dilated Cardiomyopathy. J Card Fail. 2011;17(4):272–81.
Received: 12 May 2019
Accepted: 16 July 2019
Alejandra Cevallos and Abigail Solórzano
Yachay University of Experimental Technological Research. Ecuador