2022.07.02.42
Files > Volume 7 > Vol 7 No 2 2022
Hamdi Al Mutori 1* , Mazin Al Rudaini 2
, Mazin Al Rudaini 2 , Ahmed F. Omar 3
, Ahmed F. Omar 3 , Sanam Anwar 4
, Sanam Anwar 4 , Yasser Selim 5
, Yasser Selim 5 , Bahaa Yaseen 6
, Bahaa Yaseen 6
1. Department of Medicine, National University of Science and Technology, College of Medicine, Oman; [email protected].
2. Department of Medicine, National University of Science and Technology, College of Medicine, Oman; [email protected].
3. Department of Medicine, Suhar Hospital, Oman, [email protected].
4. Department of Public Health, National University of Science and Technology, College of Medicine, Oman; [email protected].
5. Department of Radiology, Suhar Hospital, Oman; [email protected].
6. Department of Gastroenterology, Aster Hospital, Oman; [email protected]
* Corresponding Author: [email protected].
Available from: http://dx.doi.org/10.21931/RB/2022.07.02.42
ABSTRACT
Keywords. NAFLD, Obesity, Oman
INTRODUCTION
Obesity has become an increasing medical concern worldwide since its rate is steadily rising. The WHO reported that the obese population (defined as body mass index BMI equal to or more than 30 kg/m2) exceeds 500 million globally.1 Among all Arab Gulf countries, the prevalence of obesity and overweight is increasing, where more than 30% of the population is obese.2 Such higher percentages of obesity and overweight are also seen in Middle Eastern, United States, New Zealand, Canada, Australia.3
Obesity is a well-known risk factor for many medical conditions like type 2 diabetes, hypertension, dyslipidemia, and Nonalcoholic Fatty Liver Disease (NAFLD) among adults.4
It has been reported that all ranges of obesity, from overweight to obese and severely obese, are associated with NAFLD.5
The definition and diagnostic modalities for NAFLD depend on imaging or histopathological evidence of hepatic steatosis after excluding all possible secondary causes like alcohol consumption, steatogenic drugs, or genetic disorders.6
The overall prevalence of NAFLD diagnosed by imaging is between 14-31%.7 The highest prevalence is reported in the Middle East and the United States, whereas the lowest prevalence is reported in Africa.8 Increasing incidence of obesity, insulin resistance and Type 2 diabetes in Oman sensibly predict an associated increase in NAFLD incidence. Despite this, the exact figure of NAFLD prevalence is still obscured due to a lack of data.
NAFLD can be classified histologically into the nonalcoholic fatty liver (NAFL) and nonalcoholic steatohepatitis (NASH); such classification depends on the percentage of hepatic steatosis and the presence or absence of hepatic injuries with or without the element of fibrosis.6
Clinically, NAFLD presentation varies according to its histological changes. Patients with only hepatic steatosis are commonly asymptomatic; however, others might present with features related to advanced cirrhosis or hepatocellular carcinoma in its most severe form. After a speedily growing number of obese individuals in society, NAFLD has become one of the most common causes of chronic liver disease.9 NAFLD with associated cirrhosis of the liver curries considerable patient morbidity and mortality, representing a real encumbrance on health care providers.10,11 It has been found that hepatic mortality encounters the second or third cause of death among NAFLD.12
This study aims to find the prevalence of NAFLD amongst obese Omani patients and show its relationship with other components of metabolic syndrome. This will help increase healthcare providers’ orientation toward NAFLD with possible early intervention and prevention of subsequent serious complications.
METHODS
Obese patients who attended Sohar polyclinic for regular check-ups or mild acute illness were offered to be enrolled in this study between August 2018 and December 2019. All participants have explained the nature and the objectives of the study comprehensively and have given their consent to be part of it. Individuals who initially indicated known liver disease, alcohol consumption, usage of medications with possible liver damage as a side effect (Chronic use of NSAID/Acetaminophen, Methotrexate, Corticosteroid, Amiodarone, Antidepressant, Antipsychotic and Tamoxifen), those with known history of diabetes, hypertension or dyslipidemia, and those who later showed positive markers for hepatitis B or C were excluded from the study.
Obesity was diagnosed according to the WHO definition. BMI ranging between 30 and 39.9 kg/m2 was defined as Grade 2 obesity, whereas patients with a BMI of 40 kg/m2 or more were defined as having Grade 3 obesity. To obtain BMI, height and weight were measured in the OPD using the same scaling device. We followed The Eighth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VIII) recommendations in assessing blood pressure and diagnosing hypertension. Hypertension is diagnosed if the systolic blood pressure is more than 140 mmHg and the diastolic one of more than 90 mmHg.
While fasting for 12 hours, a blood sample was collected from each participant and sent for the following tests: lipid profile (total cholesterol, HDL, LDL, TG and VLDL), liver function (total bilirubin, AST, ALT, alkaline phosphatase and albumin), fasting glucose, glycosylated Hb, uric acid and hepatitis B and C markers.
To diagnose fatty liver changes, candidates who achieved inclusion criteria were examined ultrasonographically by a single qualified radiologist using the same device (multifrequency 2-5 MHz convex transducer of Toshiba Aplio 500 ultrasound machine) each time. Normal liver parenchyma displays homogeneous echogenicity equal to that of the renal cortex and spleen. In patients with fatty infiltration, the liver appears hyperechoic as the echogenicity is higher than the renal cortex and spleen with increased brightness.
Data was entered and analyzed in SPSS (version 22). The prevalence of NAFLD was calculated using frequency and percentages. Two-by-two table comparisons were made to study the covariates of NAFLD, and results were presented using descriptive statistics. Mean and standard deviations were calculated to compare continuous variables. A test of significance in a t-test was used to compare the means. A p-value of less than 0.05 was considered for statistical significance.
RESULTS
There were 55 study participants, out of which there were 28 (50.9%) males and 27 (49.1%) females. The mean age of the participants was 38.22 ± 12.62years. Out of the total study population of 55 patients, Nonalcoholic Fatty Liver Disease (NAFLD) was found in 37 patients, thus making the prevalence of NAFLD in this study 67.3%. [Table 1].
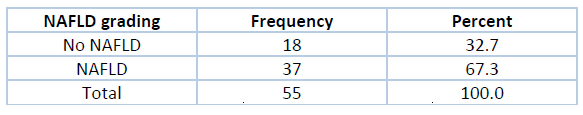
Table 1. Prevalence of NAFLD
The mean age of the NAFLD patients was 39.43 ± 2.01 years. The age distribution showed that most of them were less than 50 years of age (81.1%), and only 18.9% were more than 50 years of age. Most of the NAFLD patients were females. However, age and gender differences were not found to be statistically significant (p>0.05). Grade 2 obesity with BMI classification was found in most patients (78.3%). Mean BMI was higher in NAFLD patients (37 ± 0.34) compared to the control group, and this difference was statistically significant with a p-value <0.01.
Systolic hypertension was present only in 17 patients (45.9%), while diastolic hypertension was present in 16 patients (43.2%). Total serum bilirubin, alkaline phosphatase and albumin levels were normal in all the patients. However, AST and ALT levels were increased in most patients; 81.1% and 73%, respectively. [Table 2]
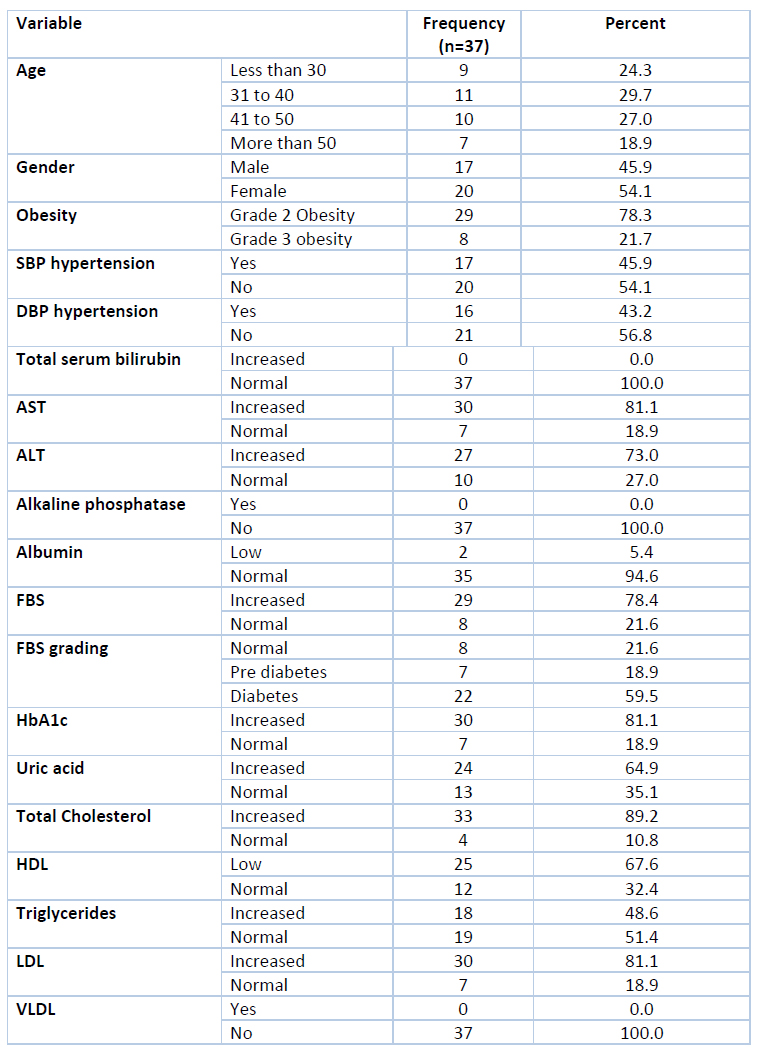
Table 2. Covariates of NAFLD in the study population
The mean values of AST and ALT levels differed significantly from the patients without NAFLD (p<0.001). According to fasting blood sugar (FBS) levels, most of the patients had diabetes (59.5%), and a few (18.9%) had prediabetes. The HbA1c levels correlated with the FBS levels, and thus in 81.1% of patients; it was higher than the normal range. Both FBS and HbA1c mean levels were higher in the NAFLD group compared to a non-NAFLD group of patients, and this difference was statistically significant (p<0.01) [Table 3]. Serum uric acid levels were high in 64.9% of patients, while total cholesterol was high in most patients (89.2%). Similarly, LDL was increased in 81.1% of patients while VLDL levels were normal. Significantly low HDL levels were found in 67.6% of patients compared to the non-NAFLD group. Mean levels of LDL, uric acid, and total cholesterol were significantly higher in the NAFLD patients (p<0.01).
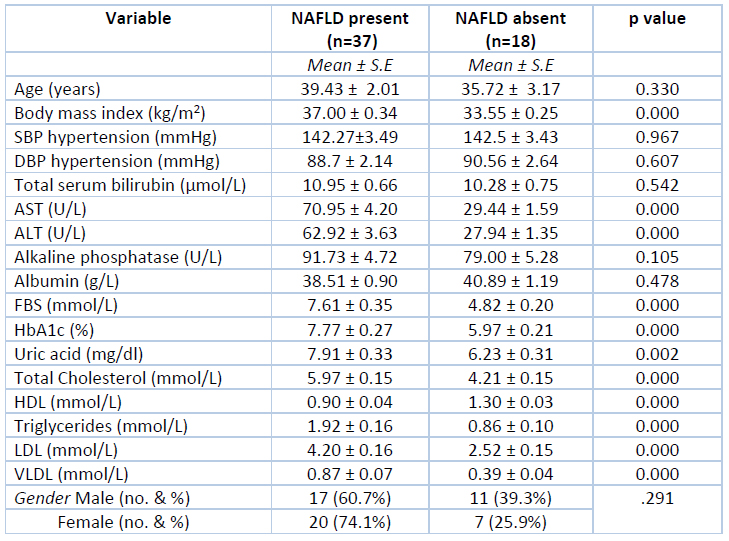
Table 3. Comparison of covariates of NAFLD in the study population
DISCUSSION
Among the six Arab Gulf countries, obesity and overweight are very high. Assessing obesity by measuring the BMI, which is linked to increased fat in the body and subsequently insulin resistance, is considered a good tool to predict possible complications. Thirty percent or more of the individuals in these countries are obese (BMI equal to or more than 30 kg/m2), and more than 60% have a weight range higher than usual (BMI equal to or more than 25 kg/m2). Similar percentages of obesity and overweight are found in other Middle Eastern countries, Maghreb countries, the United States, New Zealand, Canada, Australia, and some European countries.3 In Oman, the prevalence of obesity and overweight for males and females is 61% and 66%, respectively.3 Liver diseases in obese individuals have become a recognized medical problem worldwide. Among them, NAFLD represents the primary etiology.
In this study, we found that the overall prevalence of NAFLD is 67.3% (37 patients). The global prevalence of NAFLD diagnosed by imaging is around 25%, where the highest majority is found in the Middle East (31%), and South America (30%) and the lowest is found in Africa (13%).8 The increased prevalence of NAFLD among diabetes mellitus is well documented in many studies.13,14 Given that the prevalence of diabetes mellitus in Oman is on the rise (15.7%),15 is anticipated to find a high rate of NAFLD in Omanis, as shown in this study. Despite this, we could not find adequate data on the prevalence of NAFLD in the general population (obese or non-obese) in this country.
This study shows that NAFLD patients are slightly younger than similar studies, with a mean age of 39.43 ± 2.01 years and the majority of the patients’ age was less than 50 years. Most western studies have reported the mean age of NAFLD to be between 41-45 years. In Indian studies, the mean age was said to be (49.14±9.65) years by Mahaling et al.,16 and (42.90±10.54) years by Agarwal et al.17 This earlier development of NAFLD in the examined sample may be attributed to the early onset of obesity among young adults in the Gulf countries.18
We found that most NAFLD patients were female (81.1%). Most studies in a meta-analysis also showed a female predominance, with the mean proportion of females at 73%.19 Such females’ predominance may be due to the high prevalence of obesity. Additionally, men were less included in the study due to a history of significant alcohol intake among them compared to women in this part of the world. In controversy to other studies, male sex has been considered a risk factor for NAFLD with two times higher than females.20-22 Exploring the possible etiology behind this gender-wise discrepancy in the prevalence of NAFLD necessitates further dedicated studies.
The prevalence of hypertension, diabetes mellitus, hyperuricemia and dyslipidemia was significantly higher among obese patients (P<0.000). This obviously, could be attributed to the associated metabolic syndrome. This finding is consistent with the majority of comparable studies.16,17,23-27
NAFLD is usually symptomless in most patients due to its slowly progressing course despite possible alterations of liver functions. All patients included in our study were asymptomatic concerning the liver disease. However, deranged liver function was seen as significantly raised AST and ALT among the majority of NAFLD patients, and such finding is consistent with Marchesini et al.,28 Angulo et al.,29 Rushad Patell et al.,9 were ALT and or AST often the only laboratory abnormality found in NAFLD patients.
CONCLUSION
The increasing number of obese individuals in developing countries, including Oman, heralds the rising associated metabolic problems, including NAFLD. Our study documented this, along with the increasing prevalence of other related medical complications like hypertension, diabetes, and dyslipidemia.
Limitations
Although it reflects a significant prevalence, the number of patients included in the study is relatively small, and further, more exhaustive studies are recommended in the future.
Acknowledgments: The authors acknowledge the technical support from Sohar polyclinic, which contributed a lot to achieve this research.
Funding Sources: The authors received no financial support for this article’s research, authorship, and publication.
Conflict of Interest: The author(s) declares no conflict of interest.
REFERENCES
1. World Health Organisation. Overweight and Obesity. Factsheet no. 311. 2012. http://www.who.int/mediacentre/
2. Anastasia S, Pernille T. A, and Arja R. Aro. Health Promotion and Obesity in the Arab Gulf States: Challenges and Good Practices. J Obes. 2019; Article ID 4756260, 6 pages. Doi: 10.1155/2019/4756260.
3. World Health Organization (WHO), “Global health observatory data: Overweight &Obesity”,2016,http://www.who.int/gho/ncd/risk_factors/overweight_obesity/obesity_adults/en/.
4. Marchesini G, Bugianesi E, Forlani G, Cerrelli F, Lenzi M, Manini R, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology. 2003;37(4):917-923. Doi:10.1053/jhep.2003.50161.
5. Subichin M, Clanton J, Makuszewski M, Bohon A, Zografakis JG, Dan A. Liver disease in the morbidly obese: a review of 1000 consecutive patients undergoing weight loss surgery. Surg Obes Relat Dis 2015;11:137-141. Doi:10.1016/j.soard.2014.06.015.
6. Naga Chalasani, Zobair Younossi , Joel E. Lavine, Michael Charlton, Kenneth Cusi, Mary Rinella, et. al. The Diagnosis and Management of Nonalcoholic Fatty Liver Disease: Practice Guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328-357. Doi:10.1002/hep.29367.
7. Stefano B, Gioconda S, Flora M, Lory S. Crocè, Giovanni B, Franco S, et al. Prevalence of and risk factors for hepatic steatosis in northern Italy. Ann Intern Med. 2000; 132: 112-7. Doi: 10.7326/0003-4819-132-2-200001180-00004.
8. Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73-84. Doi: 10.1002/hep.28431.
9. Rushad P, Rupal D, Harshal J, Smit S, Purav S, Sarfaraz J. Non-Alcoholic Fatty Liver Disease (NAFLD) in Obesity. J Clin Diagn Res. 2014 Jan;8(1):62-66. Doi: 10.7860/JCDR/2014/6691.3953.
10. Sayiner M, Otgonsuren M, Cable R, Younossi I, Afendy M, Golabi P, et al. Variables associated with inpatient and outpatient resource utilization among Medicare beneficiaries with nonalcoholic fatty liver disease with or without cirrhosis. J Clin Gastroenterol. 2017;51:254-260. Doi: 10.1097/MCG.0000000000000567.
11. Adams LA, Lymp JF, St Sauver J, Sanderson SO, Lindor KD, Feldstein A, et al. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129:113-121. Doi: 10.1053/j.gastro.2005.04.014.
12. Younossi Z, Henry L. Contribution of alcoholic and nonalcoholic fatty liver disease to the burden of liver-related morbidity and mortality. Gastroenterology. 2016;150:1778-1785. Doi:10.1053/j.gastro.2016.03.005.
13. Tilg, H., Moschen, A., Roden, M. NAFLD and diabetes mellitus. Nat Rev Gastroenterol Hepatol 14, 32–42 (2017). Doi:10.1038/nrgastro.2016.147.
14. Xia MF, Bian H, Gao X. NAFLD and Diabetes: Two Sides of the Same Coin? Rationale for Gene-Based Personalized NAFLD Treatment. Front Pharmacol. 2019 Aug 6;10:877. Doi: 10.3389/fphar.2019.00877.
15. Al-Mawali A, Al-Harrasi A, Jayapal SK, Morsi M, Pinto AD, Al-Shekaili W, Al-Kharusi H, Al-Balushi Z, Idikula J. Prevalence and risk factors of diabetes in a large community-based study in the Sultanate of Oman: STEPS survey 2017. BMC Endocr Disord. 2021 Mar 5;21(1):42. Doi: 10.1186/s12902-020-00655-9.
16. Mahaling DU, Basavaraj MM, Bika AJ. Comparison of lipid profile in different grades of nonalcoholic fatty liver disease diagnosed on ultrasound. Asian Pacific journal of tropical biomedicine. 2013;3(11):907-12.
17. Agrawal R, Mishra S, Dixit VK, Rai S. Association of nonalcoholic fatty liver disorder with obesity. Indian J Prev Soc Med. 2009;40:126-9.
18. ALNohair S. Obesity in gulf countries. Int J Health Sci (Qassim). 2014 Jan;8(1):79-83. Doi: 10.12816/0006074.
19. James OFW, Day CP. Nonalcoholic steatohepatitis (NASH): a disease of emerging identity and importance. J Hepatol. 1998; 29: 495-501.
20. Fattahi MR, Niknam R, Safarpour A, Sepehrimanesh M, Lotfi M. The prevalence of metabolic syndrome in nonalcoholic fatty liver disease; a population-based study. Middle East J Dig Dis 2016;8:131-137.
21. Park KS, Lee YS, Park HW, Seo SH, Jang BG, Hwang JY, et al. Factors associated or related to with pathological severity of nonalcoholic fatty liver disease. Korean J Intern Med 2004;19:19-26.
22. Zelber-Sagi S, Nitzan-Kaluski D, Halpern Z, Oren R. Prevalence of primary nonalcoholic fatty liver disease in a population-based study and its association with biochemical and anthropometric measures. Liver Int 2006;26:856-863.
23. Khan SH, Khan FA, Ijaz A, Sattar A, Dilwar M, Hashim R. Hypertension and metabolic syndrome: impact of clustering of hypertension in subjects with metabolic syndrome. Pak Med Sci. 2007;23:903-908.
24. Leite NC, Salles GF, Araujo AL, Villela-Nogueira CA, Cardoso CR. Prevalence and associated factors of nonalcoholic fatty liver disease in patients with type-2 diabetes mellitus. Liver Int 2009;29:113-119.
25. Fan N, Zhang L, Xia Z, Peng L, Wang Y, Peng Y. Sex-specific association between serum uric acid and nonalcoholic fatty liver disease in type 2 diabetic patients. J Diabetes Res 2016;2016:3805372.
26. Wu KT, Kuo PL, Su SB, Chen YY, Yeh ML, Huang CI, et al. Nonalcoholic fatty liver disease severity is associated with the ratios of total cholesterol and triglycerides to high-density lipoprotein cholesterol. J Clin Lipidol 2016;10:420-425.e1.
27. Sudhir Navale, Dhruv Vala, Madhavi Gupta. Grading of Nonalcoholic fatty liver disease on ultrasound and its correlation with lipid profile. International Journal of Contemporary Medicine Surgery and Radiology. 2019;4(3):C187-C192.
28. Marchesini G, Brizi M,Bianchi G, et al. Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes. 2001;50:1844-50.
29. Angulo P, Keach JC, Batts KP, Lindor KD. Independent predictors of liver fibrosis in patients with nonalcoholic steatohepatitis. Hepatology. 1999;30:1356-62.
Received: 9 January 2022 / Accepted: 12 April 2022 / Published:15 May 2022
Citation: Al Mutori H , Al Rudaini M , Omar AF, Anwar S , Selim Y, Yaseen B. Nonalcoholic Fatty Liver Disease Among Obese Patients in Oman. Revis Bionatura 2022;7(2) 42. http://dx.doi.org/10.21931/RB/2022.07.02.42
