2022.07.01.6
Files > Volume 7 > Vol 7 No 1 2022
Evaluation of secondary cancers, synchronous and metachronous with bladder cancer

1 Department of Surgery, Qom University of Medical Sciences, Qom, Iran.
2 Department of Pediatric Nephrology, School of Medicine, Qom University of Medical Sciences, Qom, Iran
3 Student Research Committee, Qom University of Medical Sciences, Qom, Iran
* Corresponding author: [email protected].
Available from: http://dx.doi.org/10.21931/RB/2022.07.01.6
ABSTRACT
The number of bladder cancer survivors worldwide is increasing due to the advancement of diagnostic methods and bladder cancer treatment. Besides, bladder cancer is the sixth most common cancer in Iran. Nowadays, many secondary cancers have been proven with bladder cancer. This study focused on synchronous and metachronous cancers with bladder cancer. This study was performed retrospectively. A total of 276 patients with a definitive diagnosis of bladder cancer were included in the study. Tumors were diagnosed using ultrasound and cystoscopy. Out of 276 patients with bladder tumor, 240 underwent resection, 25 underwent radical cystectomy, and 31 underwent chemotherapy in addition to resection.
The mean age of patients was 65±3.9 years. Among the patients, 184 were male (67%), and 92 were female (33%). Smoking was the most common known risk factor. There were 165 smokers, 135 of whom were male and 30 female. Sixty-nine patients had no known risk factor (P <0.05). Gastric cancer was the most common secondary cancer with bladder cancer in all individuals (5.7%). Prostate cancer (20%) in men and cervical cancer (11.9%) in women was the most common secondary cancer simultaneous with bladder cancer. Given the importance of SPC as a cause of cancer death, early detection and screening of primary cancer survivors will increase patients' life expectancy and quality of life.
Keywords. Secondary cancers, Synchronous, Metachronous, Bladder cancer.
INTRODUCTION
Bladder cancer is the most common malignancy of the urinary system and the 11th most common cancer in people. The prevalence of this cancer is increasing in different countries of the world. This cancer's mortality rate and incidence vary in different countries and regions. This difference depends on epidemiological data, social, cultural, and economic characteristics 1-2. Bladder cancer is the sixth most common cancer in Iran. The prevalence of this cancer in Iran's population is 33.2 patients per 100,000 people 3. Statistics indicate that this cancer has an increasing prevalence in Iran 4 and registers more than 70,000 new cases and 30,000 deaths annually 5. In general, 7.04% of cancers in Iran are associated with bladder cancer 6. Bladder cancer's leading risk factor is smoking, accounting for 50-65% of all cases. Occupational or environmental toxins also play a significant role in causing this disease. In general, the risk factors for bladder cancer can be classified into three subtypes: genetic and molecular abnormalities, chemical or environmental exposure, and chronic irritation.
The bladder is an empty organ that stores urine in the lower abdomen. The urothelial cells of the bladder's lining are exposed to mutagenic substances secreted by the kidneys. These substances cause metaplasia and dysplasia changes and eventually bladder cancer. Most bladder tumors are transitional. In studies, bladder tumors have been synchronous and metachronous with other tumors. 90% of bladder cancers are diagnosed at 55 and above, and the disease is four times more common in men than women 7-10. In general, the treatment approach in bladder cancer is determined after determining the type of cancerous tissue. Treatments include bladder tumor resection, radical cystectomy, and complementary therapies such as single-dose intravesical immunotherapy with bacillus Calmette-Guérin (BCG) or intravesical chemotherapy 11. This study aimed to evaluate secondary tumors synchronous and metachronous with bladder tumors that, if diagnosed and treated in time, the disease will have a better prognosis, and the person will achieve better recovery.
MATERIALS AND METHODS
Ethics
This study was performed in the Center of Shohada Ashayer Khorramabad and Kamkar-Arabnia Hospital in Qom from 2006 to 2019. Written consent was obtained from all participants in the study. The personal information of patients included in the study was kept secret.
Study population and inclusion and exclusion criteria
In this study, 276 patients were included in the study. The inclusion criteria were those patients with significant bladder tumors. All types of bladder tumors were considered. These patients then underwent bladder tumor resection surgery based on a specialist diagnosis or, if necessary, radical cystectomy or additional treatments were considered for them 13. Suspected patients to bladder cancer, which were referred to the hospital for cystoscopy and had consented to participate in the study were included in this survey. Patients without bladder tumors and those who don't have access to a definitive diagnosis were excluded from the survey.
Tumors diagnosis
Tumors were diagnosed using ultrasound and cystoscopy12. Ultrasound was carried out with GE Voluson 730 using a convex probe with 5.3 Hz for all patients. A single individual carried out all ultrasounds. Afterward, the patients underwent cystoscopy conducted by a urologist who was not aware of the patients' ultrasound results. Afterward, tissue samples were prepared and sent to a pathology laboratory for pathological examinations. Olympus flexible fiberoptic cystourethroscopy was used for cystoscopy diagnosis of bladder tumors12.
Study procedure
This study was performed retrospectively. The patients' information in the study was evaluated at intervals of about one year and five years after the diagnosis of bladder tumor in reading files, telephone calls, self-reports, and door-to-door visits for underlying diseases and secondary cancers. In case of the patient's presence and declaration of secondary cancer, the inclusion criteria were pathology reports, biopsy, endoscopy, and cancer-appropriate imaging in their medical records in the hospital. The subjects' underlying disease information in the study was recorded as a reading of hospital information.
Statistical analysis
According to the chi-square test, all data were then analyzed using SPSS software (version 22). P-value <0.05 was considered a significant level 14-18.
RESULTS
Demographic characters
Out of 276 patients with bladder tumor, 240 underwent resection, 25 underwent radical cystectomy, and 31 underwent chemotherapy in addition to resection. The mean age of patients was 65±3.9 (69 years). The youngest was 24 years old, and the oldest was 105 years old. Among the patients, 184 were male (67%), and 92 were female (33%). Men's ratio to women was 2, and men 61-80 years old had the highest prevalence (P <0.05). Smoking was the most common known risk factor. There were 165 smokers, 135 of whom were male and 30 female. Sixty-nine patients had no known risk factor (P <0.05).
Bladder tumors frequency
Table 1 shows the frequency of bladder tumors amongst included patients. Findings showed that Transitional cell cancer (TCC) was the most frequently detected tumor amongst studied samples (88.60%) (P <0.05). However, adenocarcinoma was the less frequently detected tumor.
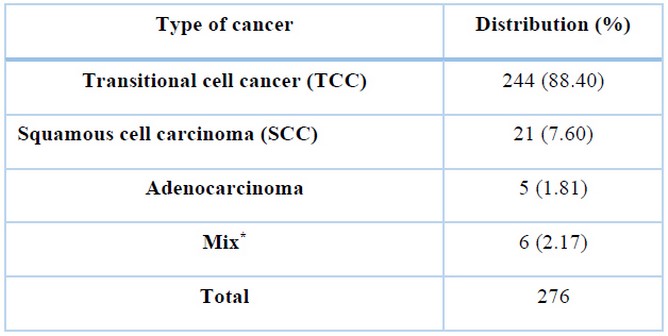
* Several types of cancers
Table 1. Frequency of bladder tumors amongst included patients.
Job frequency
Table 2 shows the job frequency of included patients. Teachers (26.44%), farmers (23.18%), and workers (17.75%) were the most frequently determined jobs amongst the study population.
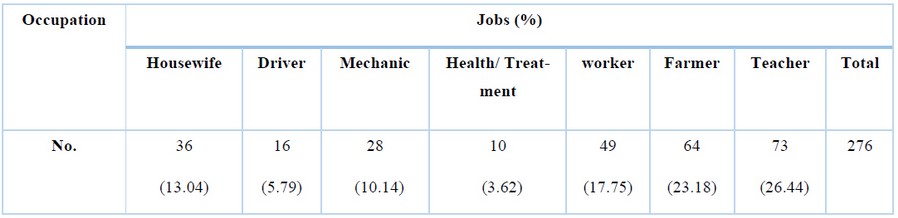
Table 2. Job frequency of included patients.
Age distribution
Table 3 shows the age distribution of examined patients. The majority of patients (30.79%) had 61-80 years old. Frequency of 0-30 and 101< years old patients were 3.26% and 8.33%, respectively.
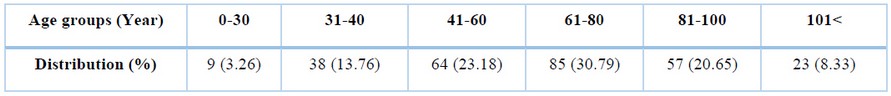
Table 3. Age distribution of studied patients.
Frequency of underlying diseases
Table 4 shows the frequency of underlying diseases amongst the studied patients. The most commonly identified underlying diseases amongst the studied patients were skeletal (35.14%), diabetes (18.47%), blood pressure (14.85%), and digestive (14.49%). Only 1.81% of examined patients had thyroid disorders. Additionally, only2.53% of patients had pulmonary disease.
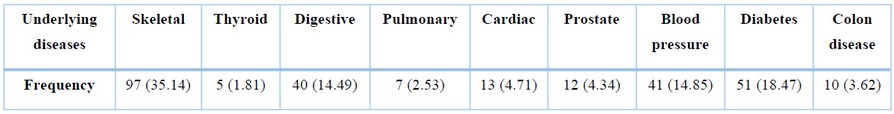
Table 4. Frequency of underlying diseases amongst the studied patients.
Other cancer distribution
Table 5 shows the frequency of other cancer types amongst the studied patients. In clinical, self-report and confirmed pathology examination, synchronous tumors, five years and if alive ten years after bladder tumor, diverse cancers were obtained. The most frequently detected cancer types were prostate (13.40%), stomach (5.79%), colon (4.34%), and cervix (3.98%). 63.40% of patients had no other cancers 5 years after the bladder tumor. No testicular tumor was clinically observed in the urogenital tract. Laryngeal and pancreatic tumors were also not observed in this study.
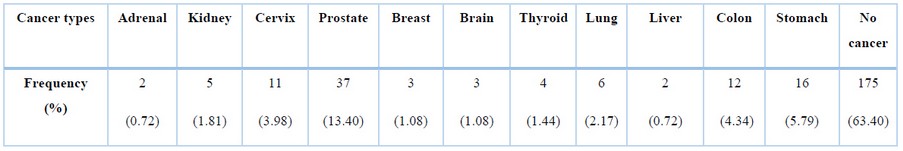
Table 5. Distribution of other cancer types among studied patients five years after bladder tumor.
DISCUSSION
Despite high advances in the medical sciences 19-24, some diseases remain health-threatening 25-30. The bladder is a hollow organ lined with mucous epithelial cells that stores urine for several hours. Mutagenic substances such as phenethylamines and benzene compounds and synthetic substances, chronic infection and inflammation cause metaplasia, dysplasia and eventually cancer and invasion to the underlying muscle tissue. According to the latest GLOBOCAN data, bladder tumors have 3% prevalence among tumors and increase in developed and developing countries. In the United States, bladder tumors are the sixth most common, mostly 55 years old, and are 2 to 4 times more common in men than women. In tumors with lower stage, the 5-year lifespan is 77%, and in metastatic cases, it is 5%. Cigarette tobacco is the most potent risk factor. Occupational and environmental factors contribute to about 20% of cases. Only about 7% of bladder tumors are inherited. In many cases, no specific exposure is found 7.
Kotake et al. 31 found that 376 patients with bladder tumors were analyzed for clinical cases. In their study, 299 patients were male, and 77 were female. The mean age of the subjects was 65.7 years. The most common synchronous tumors with bladder cancer in men were first gastric cancer (27.4%) and then prostate (15.3%), and in women, first cervical cancer (27.9%) and then gastric cancer (16.2%). Of the 119 cases, 58 were synchronous tumors, and 61 were metachronous tumors. Bladder tumors in 85% of cases coincided with other urological tumors. Also, the ratio of secondary cancers to total cancers was 5.2%, and the ratio of secondary cancers with bladder cancer to total cancers was 15.9% 31. In another study, multiple tumors were associated with prostate cancer in 93 patients (15.2%), and the organ most associated with prostate cancer was gastric cancer, followed by bladder, clone, and lung cancer. The mean age of the first, second, and third cancers was 72, 74 and 75 years. In 37 cases of death (71.4%) due to prostate cancer, the first and second cancers were about 20 months and about 8 months for third cancer. The primary stage in primary prostate tumors was lower than in secondary tumors. Survival rates were also reported to be better in this group. For this reason, it is recommended to consider the possibility of secondary cancers in primary ones 32.
In a study in Taiwan conducted by Wu et al. 33 from 1987 to 2002 on 2109 patients, 99 patients were diagnosed with multiple secondary cancers with gastric tumors (4.7%). Secondary cancer (77.8%) was diagnosed 5 years before and after gastric cancer. 34.3% of patients were diagnosed with the synchronous tumor within one year. 77 male patients, prostate cancer, was the most common (19.5%), followed by colon cancers (18.2%) and liver (14.3%). In 22 female patients, colon cancer (31.9%) first followed by breast and cervical cancers (22.7%) had the highest prevalence rate, 33. In another study in Hungary, 77,504 autopsy cases were examined, of which 385 (4.2%) had double multiple primary malignant tumors. There was no significant difference in gender. Thyroid tumors were more commonly associated with lung, breast, and gastrointestinal tumors 34. In another study, secondary cancer was seen in 16.8% of kidney cancers, 12.5% of bladder cancers, and 21.8% of prostate cancers. The cause of recurrent tumor connections can be explained somewhat by the high average age (72 years). Uropoetic cancer was associated with lung cancer (the role of tobacco), gastrointestinal tumors (genetic or dietary factors), prostate cancer, bladder cancer, and hematologic malignancies. In this study, no association was found between testicular cancer and other malignancies 35.
In the study of Özdamar et al. 36 on 147 patients with genitourinary tumors, 6 patients had another tumor, 2 of which were concomitant and 4 of which were asynchronous. Cancer patients are at higher risk of secondary cancer than the general population. Secondary cancer may be diagnosed in long-term follow-up of cancer patients, or etiological factors may cause pleiotropic effects, or it may be due to treatments for first cancer. In a study in France, from 1989 to 2004, 10047 patients with bladder cancer were evaluated for secondary cancer. This study showed that the risk of new cancer among cancer survivors is 60% higher than the general population. Male patients also had a higher risk of prostate, head, neck, and lung cancers 37. In another study by T Fukagai et al. 38 in Japan from October 1980 to December 1994, 392 patients were treated for malignant neoplasms. 42 patients (10.6%) had multiple neoplasms, their mean age was 72.2 years, and 83% were male. Malignant neoplasms of the bladder, prostate, and kidney were observed in 19 (35%), 19 (35%), and 10 cases (11%), respectively. The incidence of prostate cancer was more associated with genitourinary organs than other primary malignant neoplasms. Other organs which had malignant neoplasms along with the genitourinary tract organs were the stomach (39%), lungs (12%), esophagus (9%), and pancreas (9%). Only 16 patients (35%) simultaneously had multiple malignancies neoplasms.
In a study by Whi-An Kwon et al. 39 in South Korea from 1993 to 2013, 48,875 people were investigated with an early diagnosis of bladder cancer. Bladder cancer survivors were at increased risk for some secondary cancers, particularly prostate and kidney, squamous cell carcinoma of the lung, and the lung's adenocarcinoma. In the cohort study by Eric Adjei Boakye et al., 40 2903241 cancer patients were identified, of which 259685 (8.9%) developed secondary cancer (7.6% female and 10.3% male). Patients with smoking-related cancers had a higher risk of developing SPC than patients with non-smoking-related cancers. Besides, considering the infection of 30-80% of different communities with H. pylori and proving its role in the development of various cancers, including gastric cancer and its concurrence with bladder cancer in most studies 41, 42, it seems that the prevalence of this infection also plays a role in the development of multiple secondary cancers.
However, specific research should assess other aspects and epidemiological properties of bladder cancer among the population. The study was limited to the low number of samples and low frequencies of studied groups.
CONCLUSION
Due to the increasing trend of bladder cancer worldwide and the evidence of concurrence or subsequent secondary cancers, identifying the causative agents and related risk factors can improve the prognosis of the disease and increase the life expectancy and quality of life of patients with this cancer. Therefore, it is essential to continuously monitor the risk of secondary cancer among bladder cancer survivors. On the other hand, owing to the growing number of cancer survivors cases and the SPC importance as a cancer death reason, there is a need to upsurge SPC screening and prevention.
REFERENCES
1. Rozanec, José J., Fernando P. Secin. Epidemiología, etiología, prevención del cáncer vesical. Arch Esp Urol.2020: 73(10), 872–878.
2. Mathur, P., Sathishkumar, K., Chaturvedi, M., Das, P., Sudarshan, K.L., Santhappan, S., Nallasamy, V., John, A., Narasimhan, S., Roselind, F.S. Icmr-Ncdir-Ncrp Investigator Group. 2020. Cancer statistics, report from national cancer registry programme, India. JCO Global Oncol. 2020;6:1063-1075.
3. Farmanfarma, K.K., Mahdavifar, N., Salehiniya, H. Bladder Cancer in Iran: An Epidemiological Review. Res Report Urol. 2020;12:91-103.
4. Hassanipour, S., Fathalipour, M. Salehiniya, H. The incidence of prostate cancer in Iran: a systematic review and meta-analysis. Prostate Int. 2018;6(2):41-45.
5. Ahmadi, M., Ranjbaran, H., Amiri, M..M, Nozari, J., Mirzajani, M.R., Azadbakht, M., Hosseinimehr, S.J. Epidemiologic and socioeconomic status of bladder cancer in Mazandaran Province, northern Iran. Asian Pac J Cancer Prev. 2012;13(10):5053-6.
6. Shakhssalim, N., Hosseini, S.Y., Basiri, A., Eshrati, B., Mazaheri, M. Soleimanirahbar, A. Prominent bladder cancer risk factors in Iran. Asian Pacific J Cancer Prev. 2010;11(3): 601-6.
7. Silverman, D.T., Hartge, P., Morrison, A.S. Devesa, S.S. Epidemiology of bladder cancer. Hematol/Oncol Clin North Am. 1992;6(1):1-30.
8. Kaufman, D.S., Shipley, W.U. Feldman, A.S. Bladder cancer. The Lancet. 2009;374(9685):239-249.
9. Sanli, O., Dobruch, J., Knowles, M.A., Burger, M., Alemozaffar, M., Nielsen, M.E. Lotan, Y. Bladder cancer. Nature Rev Dis Primer. 2017;3(1):1-19.
10. Jégu, J., Colonna, M., Daubisse-Marliac, L., Trétarre, B., Ganry, O., Guizard, A.V., Bara, S., Troussard, X., Bouvier, V., Woronoff, A.S. Velten, M. The effect of patient characteristics on second primary cancer risk in France. BMC Cancer. 2014;14(1):1-14.
11. DeGeorge, K.C., Holt, H.R. Hodges, S.C. Bladder cancer: diagnosis and treatment. Am Family Physic. 2017;96(8):507-514.
12. Herr, H.W. Outpatient flexible cystoscopy and fulguration of recurrent superficial bladder tumors. J Urol. 1990;144(6):1365-1366.
13. DeGeorge, K.C., Holt, H.R. Hodges, S.C. Bladder cancer: diagnosis and treatment. Am Family Physician. 2017;96(8):507-514.
14. Dehkordi FS, Momtaz H, Doosti A. Application of Real-Time PCR for detection of Aspergillus species in aborted ruminant foetuses. BulgaJ Vet Med. 2012;15(1):30-6.
15. Dehkordi, F.S., Saberian, S., Momtaz, H. Detection and segregation of Brucella abortus and Brucella melitensis in Aborted Bovine, Ovine, Caprine, Buffaloes and Camelid Fetuses by application of conventional and real-time polymerase chain reaction. The Thai J Vet Med. 2012;42(1):13.
16. Dehkordi FS. Prevalence study of Coxiella burnetii in aborted ovine and caprine fetuses by evaluation of nested and real-time PCR assays. American J Anim Vet Sci. 2011;6(4):180-6.
17. Dehkordi FS, Tirgir F, Valizadeh Y. Effects of Guajol® ointment synthesized from medicinal smoke condensate of jennet feces on burn wound healing on Wistar rat. Vet Res Forum. 2017; 8(3):215.
18. Dehkordi FS, Tavakoli-Far B, Jafariaskari S, Momtaz H, Esmaeilzadeh S, Ranjbar R, Rabiei M. Uropathogenic Escherichia coli in the high vaginal swab samples of fertile and infertile women: virulence factors, O-serogroups, and phenotyping and genotyping characterization of antibiotic resistance. New Microb New Infect. 2020;38:100824.
19. Dehkordi FS, Haghighi N, Momtaz H, Rafsanjani MS, Momeni M. Conventional vs real-time PCR for detection of bovine herpes virus type 1 in aborted bovine, buffalo and camel foetuses. Bulgar J Vet Med. 2013;16(2):102-12.
20. Dehkordi FS, Yazdani F, Mozafari J, Valizadeh Y. Virulence factors, serogroups and antimicrobial resistance properties of Escherichia coli strains in fermented dairy products. BMC Res Notes. 2014;7(1):1-8.
21. Dehkordi FS, Barati S, Momtaz H, Ahari SN, Dehkordi SN. Comparison of shedding, and antibiotic resistance properties of Listeria monocytogenes isolated from milk, feces, urine, and vaginal secretion of bovine, ovine, caprine, buffalo, and camel species in Iran. Jundishapur J Microbiol. 2013;6(3):284.
22. Ghorbani F, Gheisari E, Dehkordi FS. Genotyping of vacA alleles of Helicobacter pylori strains recovered from some Iranian food items. Trop J Pharm Res. 2016;15(8):1631-6.
23. Dehkordi FS, Gandomi H, Basti AA, Misaghi A, Rahimi E. Phenotypic and genotypic characterization of antibiotic resistance of methicillin-resistant Staphylococcus aureus isolated from hospital food. Antimicrob Res Infect Control. 2017;6(1):1-1.
24. Dehkordi FS. Prevalence study of Bovine viral diarrhea virus by evaluation of antigen capture ELISA and RT-PCR assay in Bovine, Ovine, Caprine, Buffalo and Camel aborted fetuses in Iran. AMB Express. 2011;1(1):1-6.
25. Dehkordi FS, Parsaei P, Saberian S, Moshkelani S, Hajshafiei P, Hoseini SR, Babaei M, Ghorbani MN. Prevalence study of Theileria annulata by comparison of four diagnostic Techniques in shouthwest Iran. Bulgar J Vet Med. 2012;15(2): 123-130.
26. Dehkordi FS, Haghighi Borujeni MR, Rahimi E, Abdizadeh R. Detection of Toxoplasma gondii in raw caprine, ovine, buffalo, bovine, and camel milk using cell cultivation, cat bioassay, capture ELISA, and PCR methods in Iran. Foodborne Pathog Dis. 2013;10(2):120-5.
27. Dehkordi FS, Khamesipour F, Momeni M. Brucella abortus and Brucella melitensis in Iranian bovine and buffalo semen samples: The first clinical trial on seasonal, Senile and geographical distribution using culture, conventional and real-time polymerase chain reaction assays. Kafkas Univ Vet Fak Derg. 2014;20(6):821-8.
28. Dehkordi FS, Valizadeh Y, Birgani TA, Dehkordi KG. Prevalence study of Brucella melitensis and Brucella abortus in cow's milk using dot enzyme linked immuno sorbent assay and duplex polymerase chain reaction. J Pure Appl Microbiol. 2014;8(2):1065-9.
29. Safarpordehkordi F, Yahaghi E, Khodaverdi Darian E. Prevalence of antibiotic resistance in Escherichia coli isolated from poultry meat supply in Isfahan. Iran J Med Microbiol. 2014;8(2):41-7.
30. Safarpour Dehkordi F, Hosseini S, Rahimi E, Momeni M, Yahaghi E, Khodaverdi Darian E. Investigate the frequency of virulence genes Vibrio parahaemolyticus isolated from fish, lobsters and crabs caught from Persian Gulf. Iran J Med Microbiol. 2014;8(2):1-7.
31. Kotake, T. Kiyohara, H. Multiple primary cancers (MPC) associated with bladder cancer: an analysis of the clinical and autopsy cases in Japan. JPN J Clin Oncol. 1985;15:201-210.
32. Nakata, S., Takahashi, H., Takezawa, Y., Kobayashi, M., Suzuki, T., Kawashima, K. Hinyokika kiyo. Acta Yrol JPN. 200;46(6):385–391.
33. Wu, C.W., Lo, S.S., Chen, J.H., Hsieh, M.C., Li, A.F. Lui, W.Y. Multiple primary cancers in patients with gastric cancer. Hepato-Gastroenterol. 2006;53(69):463-467.
34. Tiszlavicz, L., Varga, Z. Pajzsmirigyrákhoz társuló malignus tumorok autopsziás anyagban [Malignant tumors associated with thyroid cancer in an autopsy material]. Orvosi Hetilap. 1991;132(11):575–578.
35. Laszlo, T. Istvan, S. Urologiai multiplex tumorok autopsias anyagban. Orvosi Hetilap. 1993;134(11):577-577.
36. Özdamar, A.S., Gültekin, E.Y. Gökalp, A. Multiple primary tumours of the urogenital system: our cases and a review of the literature. Int Urol Nephrol. 1997;29(5):511-515.
37. Muller, J., Grosclaude, P., Lapôtre‐Ledoux, B., Woronoff, A.S., Guizard, A.V., Bara, S., Colonna, M., Troussard, X., Bouvier, V., Trétarre, B. Velten, M. Trends in the risk of second primary cancer among bladder cancer survivors: a population‐based cohort of 10 047 patients. BJU Int. 2016;118(1):53-59.
38. Fukagai, T., Ishihara, M., Funabashi, K., Naitoh, Y., Maruyama, K. Hinyokika kiyo. Acta Urol Japonica. 1996;42(3), 181–185.
39. Kwon, W.A., Joung, J.Y., Lim, J., Oh, C.M., Jung, K.W., Kim, S.H., Seo, H.K., Park, W.S., Chung, J., Lee, K.H. Won, Y.J. of second primary Cancer among bladder Cancer patients: a population-based cohort study in Korea. BMC Cancer. 2018;18(1):1-9.
40. Boakye, E.A., Wang, M., Sharma, A., Jenkins, W.D., Osazuwa-Peters, N., Chen, B., Lee, M. Schootman, M. Risk of second primary cancers in individuals diagnosed with index smoking-and non-smoking-related cancers. J Cancer Res Clin Oncol. 2020;146(7):1765-1779.
41. Al-Marhoon, M.S., Ouhtit, A., Al-Abri, A.O., Venkiteswaran, K.P., Al-Busaidi, Q., Mathew, J., Al-Haddabi, I., Shareef, O., Aquil, S., Rahman, K. Al-Hashmi, I. Molecular evidence of Helicobacter pylori infection in prostate tumors. Current Urol. 2014;8(3): 138-143.
42. Park, J.Y., Forman, D., Waskito, L.A., Yamaoka, Y., Crabtree, J.E. Epidemiology of Helicobacter pylori and CagA-positive infections and global variations in gastric cancer. Toxins. 2018;10(4):163.
Received: 10 June 2021 / Accepted: 26 August 2021 / Published: date. 15 February 2022
Citation: Eshagh Hosaini S K, Heidari M, Fatemi Manesh H. Evaluation of secondary cancers, synchronous and metachronous with bladder cancer. Revis Bionatura 2022;7(1). 6. http://dx.doi.org/10.21931/RB/2022.07.01.6