2021.06.03.22
Files > Volume 6 > Vol 6 No 3 2021
Risk factors in bacterial colonization of internal ureteral stent
Ekremah K. Shaker1, Fatima A. Chaloob*2
Available from http://dx.doi.org/10.21931/RB/2021.06.03.22
ABSTRACT
A ureteral stent is most broadly used to manage upper urinary tract disorders such as obstruction and prevent post-endoscopic complications. However, the stent may become a niche for bacterial colonization. This study aimed to determine the rate of bacterial colonization and type of bacteria in internal ureteral stents and the risk factors associated with bacterial colonization. This prospective cross-sectional study included 100 consecutive adult patients who had temporary ureteral stenting as preparation for a secondary ureterorenoscopy at Al-Yarmook Hospital/ Baghdad. All included patients were negative for bacterial culture before stenting.
Stent and urine culture were performed at the time of stent removal. The colonization rate and bacteriuria in patients with internal ureteral stent were 19% and 9%, respectively. The most common bacteria in-stent and urine were E. coli accounting for 31.58% and 33.33%. Pseudomonas aeruginosa was common in stent culture, representing 21.05%. Positive bacterial culture was confirmed in 19 stents and 9 urine samples. All cases with positive urine samples were also positive for culture. Thus, the sensitivity and specificity of urine culture for detection of stent colonization were 47.37% and 100%, respectively. Diabetes mellitus, chronic renal failure, and prolonged stenting were significantly associated with increased stent colonization. The ureteral stent could be a source of urinary tract infection. The most pathogenic bacteria associated with the ureter stent are E. coli and Pseudomonas aeruginosa. Risk factors associated with stent colonization are diabetes mellitus, chronic renal failure, and prolonged indwelling time.
Keywords: Ureteral stent colonization, urine culture, bacterial profile, urinary tract infection
INTRODUCTION
Ureteral Double-J (DJ) stents are broadly employed to treat obstruction in upper urinary tract and avoid post-endoscopic complications. Moreover, these stents are also used to decrease the possible risk of obstruction resulting in stone fragmentation after extracorporeal shock-wave lithotripsy (ESWL), especially in patients with relatively large stones1. On the other hand, a ureteral stent is generally associated with several complications, including dysuria, hematuria, lumbar or suprapubic pain2, stent migration, fragmentation, and encrustation. However, the most severe complication possibly involves the biofilm formation on the stent and infection, which may be associated with bacteremia, renal worsening, pyelonephritis, or even mortality because of the development of sepsis3.
The biofilms that form on the ureteral stent can originate from urinary tract microbiota or contamination of the stent during insertion of the device4. Moreover, the internal ureteral stents offer a perfect medium for bacterial adhesion, colonization, and biofilm formation5. Regardless of its origin, biofilm formation on the stent indicates that even very small numbers of bacteria can rapidly benefit from the niche-altering non-self material to grow and increase their population. Previous studies in stented patients have indicated that 70% to 90% of those patients developed bacterial colonization6.
The present study aimed to determine the rate of bacterial colonization and type of bacteria in an internal ureteral stent and determine the risk factors associated with bacterial colonization of these stents.
MATERIAL AND METHODS
Patients
This is a single prospective center observational study including all consecutive adult patients who had ureteral stenting as part of management for a secondary ureterorenoscopy (URS) due to urolithiasis during the period from April 2020 to May 2021 in the department of Urology/ Al-Yarmook Teaching Hospital, Baghdad, Iraq. Patients positive for urine bacterial culture, immune suppression, pregnant women, those with previous surgery for lower urinary tract, and those who refused to give consent were excluded from the study. Demographic data, including age, gender, body mass index (BMI), the presence of comorbidities, and stent dwelling time, were extracted through direct interviews or from patient records. The study was approved by the Institutional Review Board (IRB) of Al-Dewaniyah Technical Institute, Al-Furat Al-Awsat Technical University. Written consent from each participant was obtained at the time of sample collection after explaining the aim of the study. Each patient was given the complete unconditioned choice to withdraw anytime. The patients were assured that data will be used for research purposes only. Based on inclusion and exclusion criteria, the eligible patients who give the consent form were 100 patients.
Bacterial Isolation from Stents and Urine
At the time of stent removal, Midstream urine from all patients was collected. The stents were removed under antiseptic conditions with the aid of a cystoscope and foreign body forceps. All stent segments (inner and outer surface and the stent tip) were splashed with 1 mL sterile tryptic soy broth solution. The resultant liquid was vortexed for 1 minute, then diluted (1/100) with phosphate buffer saline. Both urine samples and diluted stent preparation were immediately transferred to a Brain heart infusion (BHI) medium. The medium was incubated at 37°C overnight. The samples were then subcultured aerobically on MacConkey agar, while chocolate agar media was used for incubation under CO2 conditions. The growth of microorganisms on the agar was evaluated quantitatively (growth of >1000 colony-forming units/mL was considered positive)7. Api20E system was used to identify Enterobacteriaceae, while Api Staph System was used to identify staphylococci (bio-Merieux, France). These systems can detect bacteria to species level. For other bacteria, routine biochemical tests were used for identification. These included the oxidase test, catalase test, CAMP test, motility agar, and urease test.
Statistical Analysis
All statistical analyses were performed using SPSS Statistics Windows, Version 25.0 (Armonk, NY: IBM Corp.). Data were expressed as mean and standard deviation (for quantitative variables) and frequency and percentage (for binomial variables). Student t-test or Chi-square as required was used to compare the association between different factors and the stent colonization. The level of significance was set at p < 0.05
Demographic and Clinical Characteristics of the Patients
The mean age of the patients was 53.01±9.67 years (range 26-82 years). About three-quarters of the patients were males. The mean BMI was 26.44±3.57 kg/m2. Most patients (60%) had no comorbidity, while 25% and 24% of them were suffering from DM or hypertension, respectively. The mean stent indwelling time was 42.32±9.9 days (range 24-66 days), as shown in table 1.
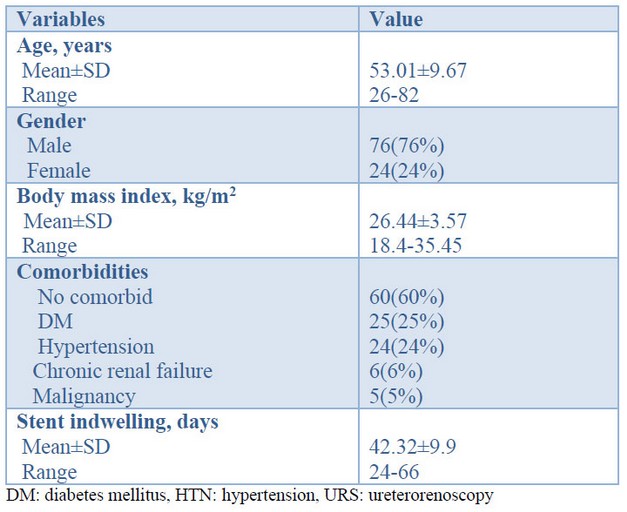
Table 1. Patients' characteristics and demographic data (n=100)
Microbiology
Out of 100 stents, positive culture was confirmed in 19 stents (19%). On the other hand, only 9 urine samples had a positive culture. Interestingly, all positive urine samples were positive for stent culture. On the other hand, 10 positive stent cultures had negative urine cultures. Thus, urine culture's sensitivity and specificity for stent colonization detection are 47.37% and 100%, respectively (Table 2).
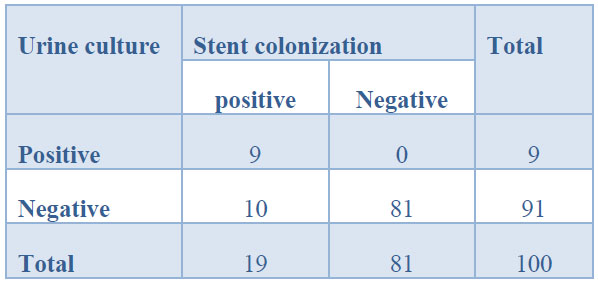
Table 2: Relationship of stent colonization with urine culture
The most common bacterium was E. coli encountered in 31.58% and 33.33% of stent and urine cultures. P. aeruginosa came next accounted for 21.05% of stent colonization but was not detected in urine samples. Staphylococcus epidermidis and Klebsiella pneumoniae were detected in 10.53% and 11.11% of stent and urine culture, respectively (Table 3). None of the stent or urine cultures had mixed infection.
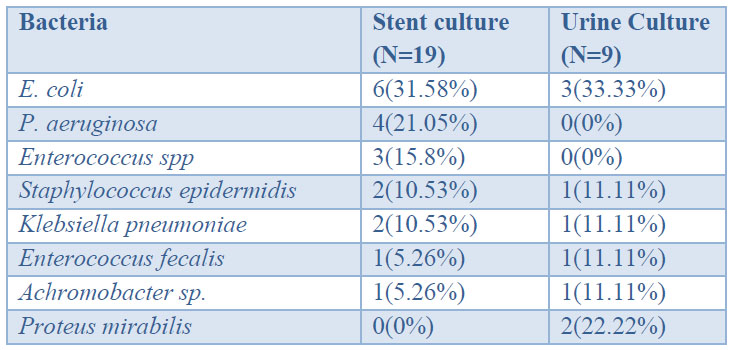
Table 3. Bacterial isolates from stent and urine samples
Association of Demographic and Clinical Characteristics with Stent Colonization
Two factors were significantly associated with stent colonization: comorbidities and stent indwelling. A 47.37% of patients in the bacterial colonization group had DM compared with 19.75% among patients without colonization with a significant difference. Similarly, chronic renal failure was more common among patients than without colonization (15.79% vs. 3.7%), with a significant difference. The mean time for indwelling stent patients with colonization was 47.68±9.63 days compared with 41.06±9.59 days in patients without colonization, with a highly significant difference (Table 4).
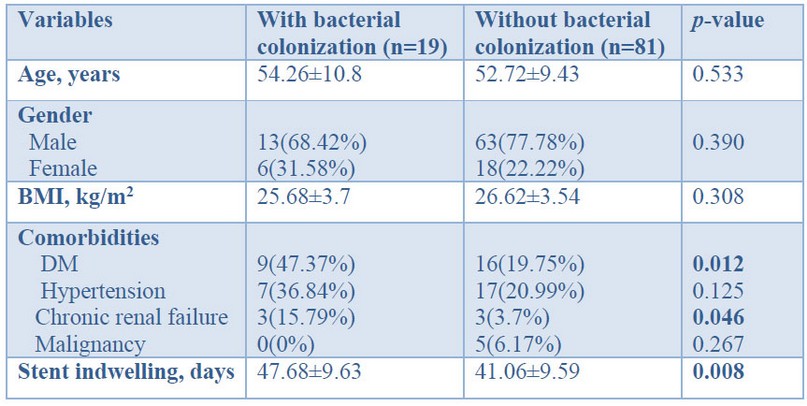
Table 4. Association of demographic and clinical characteristics with stent colonization
DISCUSSION
According to the result of the present study, 19% and 9% of internal ureteral stents and urine samples were positive for bacterial colonization. A speedy result was obtained by Ulkar et al.8, in which bacterial colonies were demonstrated in 20%. Also, Lojanapiwat9 reported that bacterial colonization and growth in-stent culture was detected in 7 of 35 patients (20%). A much higher rate was reported in other studies. Kehinde et al.10 reported that about 42 % of patients with indwelled stent had their stent colonized, while 17% developed bacteriuria. Lifschitz et al.11 reported that 45 of their patients had positive stent culture, and 15% suffered from bacteriuria. In Bangladesh, Rahman et al.6 investigated 100 adult patients who had ureteral stent placement for different urinary tract operations. Bacterial colonies were found in 45% of the stent, while bacteriuria was found only in 21% of patients. On the other extreme, as high as 90% of stent colonization was reported in an earlier series of 30 patients12.
These discrepancies in the colonization rate may be attributed to several factors, the most important of which are the polymer characteristic of the stent, indwelling times, different patient populations, and technical issues. The relatively low rate of colonization in the present study reflects the high standard of hygiene followed by the operative team, and maybe some prophylactic antibiotics were taken by the patients.
In the present study, the sensitivity and specificity of bacteriuria in the detection of stent colonization were 47.37% and 100%, respectively. In a similar study, Lifshitz et al.11 demonstrated that the sensitivity and specificity of urine culture were 31% and 97%, respectively. Thus, in most cases, urine culture had low sensitivity and very high specificity because mostly urine gives negative results when there is no stent colonization, but not all stent colonization results in bacteriuria.
According to the present study, E. coli and. P. aeruginosa was the most predominant pathogen in-stent and urine culture. In this regard, different studies disclosed different bacterial profiles of stent and urine colonization. In many previous studies, E. coli and Enterococci spp were found to be the most prevalent13-14. In a Turkish study, the most frequently isolated bacteria were Staphylococcus epidermidis, Escherichia coli, and Enterococcus faecalis8. In Rahman's et al.'s study, E. coli was the common organism isolated from both stent and urine6. Lojanapiwat et al.9 found that Staphylococcus epidermidis is the predominant bacteria responsible for stent colonization. Two other recent studies described gram-positive pathogens, particularly Staphylococcus, as predominant bacterium15-16. Farsi et al.13 reported that P. aeroginosa was most commonly isolated from both stents and urine. Paick et al.17 isolated Enterococcus species from 6 stents out of 25, followed by E. coli (5 of 25). They indicated that Gram-positive and gram-negative bacteria were similarly distributed in-stent cultures; nevertheless, only gram-negative bacteria were established in urine cultures. Another study demonstrated that Acinetobacter sp. and R. pickettii were the most common pathogens, followed by Staphylococci and Pseudomonas species in-stent culture7.
Therefore, it seems that each study has its peculiar conditions regarding antibiotic use, isolation, stent material, and study population that result in specific bacterial profiles.
There was almost complete agreement between stent and urine in the types of bacterial isolates. These data suggest that colonization in the stent is a crucial step of UTI and precedes colonization in the urine.
In the present study, DM and chronic renal failure, as comorbidities, were significantly associated with an increased stent colonization rate. Furthermore, the meantime for indwelling stent patients with colonization was significantly longer than in patients without colonization. Following these results is the outcome of many previous studies worldwide. Akay et al.14 investigated risk factors for UTI and stent colonization in 190 patients with ureteral stents. The independent risk factors for the development of UTI were DM, chronic renal failure, and pregnancy. Altuna et al.18 demonstrated that UTI was more common in patients with ureteral stents with DM and chronic renal failure.
Diabetes is known to hurt the immune system. Besides, the presence of sugar in the urinary tract enhances bacterial growth. On the other hand, chronic renal failure is associated with urinary stagnation, alkalization of urine, and absence of flushing action19. All these factors increase the likelihood of bacterial colonization.
The association of prolonged stent dwelling with stent colonization is beyond dispute. Most studies in this regard demonstrated that stent dwelling periods were significantly correlated with stent colonization rates 10. The longer the indwelling period, the higher rate of stents colonized. Rahman et al.6 disclosed that the colonization rate was 71.4% in stents that exist for 6 weeks compared to 33.3% in those that exist for 4-6 weeks and 23.5% for stents removed before 4 weeks. In a prospective study, Farsi et al.13 investigated stent colonization in 266 patients for 2 weeks to 27 months. A linear correlation was disclosed between the indwelling time and stent colonization rate. Coskun et al.20 emphasized that prompt removal of the stent can significantly decrease the rate of UTI. Shabenaa et al.21 did not find bacterial colonization in the first two weeks of stent employment.
As dwelling time increases, there will be more chance for different bacterial strains to adhere and colonize the stent regardless of the stent material. Eventually, a biofilm is formed, and most bacteria find their way to the urine.
The study has some limitations. Firstly, it was a single-center study with a limited number of patients, and the result cannot be generalized. Therefore, multicenter studies with a larger sample size are required for more solid conclusions. Secondly, the study did not link stent colonization with clinical symptoms and patients' quality of life. That is because the study was intended to be a microbiological rather than a clinical study. However, this study provides a clear insight into the risk of bacterial colonization of internal ureteral stent.
CONCLUSIONS
The study findings indicate the importance of internal ureteral stent as a source for UTI. The most pathogenic bacteria associated with the ureter stent are E. coli and Pseudomonas aeruginosa. Risk factors associated with stent colonization are DM, chronic renal failure, and indwelling time. Thus, the use of ureter stents should be reduced to a short dwelling time. Otherwise, every measure should be taken to reduce the sent colonization, especially in diabetics and patients with chronic renal failure, such as regular urine analysis and prophylactic broad-spectrum antibiotics.
Conflict of interest
The authors declare no conflict of interest.
Authors' Declaration
The authors at this moment declare that the work presented in this article is original and that they will bear any liability for claims relating to the content of this article.
REFERENCES
- Shinde S, Al Balushi Y, Hossny M, Jose S, Al Busaidy S. Factors Affecting the Outcome of Extracorporeal Shockwave Lithotripsy in Urinary Stone Treatment. Oman Med J. 2018;33(3):209-217.
- Joshi HB, Stainthorpe A, Keeley FX, MacDonagh R, Timoney AG. Indwelling ureteral stents: evaluation of quality of life to aid outcome analysis. J Endourol. 2001;15:151-154.
- Ranganathan M, Akbar M, Ilham MA, Chavez R, Kumar N, Asderakis A. Infective complications associated with ureteral stents in renal transplant recipients. Transplant Proc. 2009;41(1):162-4.
- Bossa L, Kline K, McDougald D, Lee BB, Rice SA. Urinary catheter-associated microbiota changes in accordance with treatment and infection status, PLoS One. 2017;12(6):e0177633.
- Valentin Z, Patrick B, Werner A, Matthias B, Qun R, Hans-Peter S, Dominik A. Biofilm formation on ureteral stents – incidence, clinical impact and prevention. Swiss Med Wkly. 2017;147:w14408.
- Rahman MA, Alam MM, Shamsuzzaman SM, Haque ME. Evaluation of bacterial colonization and bacteriuria secondary to internal ureteral stent. Mymensingh Med J. 2010;19, 366–371.
- Ozgur BC, Ekıcı M, Yuceturk CN, Bayrak O. Bacterial colonization of double J stents and bacteriuria frequency. Kaohsiung J Med Sci. 2013;29(12):658-61.
- Ulkar V, Yilmaz N, Agus N, Can E, Cakmak O, Yucel C, Celik O, Libey YO. Bacterial colonization of ureteral double-J stents in patients with negative urine culture. J Urological Surg 2019;2:125-129.
- Lojanapiwat B. Colonization of internal ureteral stent and bacteriuria. World J Urol. 2006;24(6):681-683.
- Kehinde EO, Rotimi VO, Al-Hunayan A, Abdul-Halim H, Boland F, Al-Awadi KA. Bacteriology of urinary tract infection associated with indwelling J ureteral stents. J. Endourol. 2004;18:891-896.
- Lifshitz DA, Winkler HZ, Gross M. Predictive value of urinary cultures in assessment of microbial colonization of ureteral stents. J Endourol. 1999;13:735–738.
- Reid G, Denstedt JD, Kang YS, Lam D, Nause C. Microbial adhesion and biofilm formation on ureteral stents in vitro and in vivo. J Urol. 1992;148:1592-1594.
- Farsi HM, Mosli HA, Al-Zemaity MF, Bahnasy AA, Alvarez M. Bacteriuria and colonization of double-pigtail ureteral stents: long-term experience with 237 patients. J Endourol. 1995;9:469–472 2.
- Akay AF, Aflay U, Gedik A. Risk factors for lower urinary tract infection and bacterial stent colonization in patients with a double J ureteral stent. Int Urol Nephrol. 2007;39:95-98.
- Aydin HR, Irkilata H, Aydin M, Gorgun S, Demirel HC, Adanur S, Keles M, Atilla A, Atilla MK. Incidence of bacterial colonisation after indwelling og double-J ureteral stent. Arch Ital Urol Androl. 2016;87:291-294.
- Nevo A, Mano R, Schreter E, Lifshitz DA. Clinical implications of stent culture in patients with indwelling ureteral stents prior to ureteroscopy. J Urol. 2017;198:116-121.
- Paick SH, Park HK, Oh SJ, Kim HH. Characteristics of bacterial colonization and urinary tract infection after indwelling of double-J ureteral stent. Urol. 2003;62(2):214-217.
- Altunal N, Willke A, Hamzaoğlu O. Ureteral stent infections: a prospective study. Braz J Infect Dis. 2017;21(3):361-364.
- Richa C, Bhushan CS, Kumar SP, Dev PN, Nabaraj P. Bacteriology of Urinary Tract Infection of Chronic Renal Failure Patients Undergoing for Hemodialysis. J Microbiol Exp. 2016;3(3): 00089.
- Coskun AK, Harlak A, Ozer T, Eyitilen T, Yigit T, Demirbas‚ S. Is removal of the stent at the end of 2 weeks helpful to reduce infectious or urologic complications after renal transplantation? Transplant Proc. 2011;43:813e5.
- Shabenaa KS, Bhargava R, Manzoor MAP, Mujeeburahiman M. Characteristics of bacterial colonization after indwelling double-J ureteral stents for different time duration. Urol Ann. 2018;10:71-75.
Received: 20 April 2021
Accepted: 15 July 2021
Ekremah K. Shaker1, Fatima A. Chaloob*2
1Medical Laboratory Technique/ Al-Rasheed University College/ Iraq
https://orcid.org/0000-0002-7240-5715
*Corresponding author email: [email protected],
2Al-Dewaniyah Technical Institute, Al-Furat Al-Awsat Technical University/Iraq
