2022.07.04.14
Files > Volume 7 > Vol 7 No 4 2022
Evaluation of ejection fraction in patients with Acute Myocardial Infarction in Mosul City, Iraq
1. Dept. of Basic Science / College of Nursing / University of Mosul, Iraq.
2. Dept. of Physiology / College of Medicine / University of Mosul, Iraq2. [email protected].
3. Dept. of Biology / College of Science / University of Mosul, Iraq3. [email protected].
Correspondence: [email protected]
Available from: http://dx.doi.org/10.21931/RB/2022.07.04.14
ABSTRACT
Between 1 January 2021 and 1 July 2021, 120 blood samples from acute myocardial infarction (AMI) patients—60 as controls and 60 patients—of both sexes who were accepted to the cardiac surgery unit at AL- Salam teaching hospital, the intensive cardiac care unit, and outpatient clinics in Mosul City/Iraq, were taken. In the presented research, the ejection fraction regarding patients with AMI was evaluated by echocardiography, and the blood-liver enzyme levels (ALP and AST \ ALT ratio) were examined in those patients. The findings indicate that patients with AMI in the age range of 35 to 45 years have a (52.41) % ejection fraction (EF) rate, which is closer to (51.344%) than it is in samples from healthy controls. In addition to that, findings indicate that patients in an age range of 46 to 56 years have heart failure with a mid-range EF (HFmrEF), with a (48.13%) percentage, whereas this heart failure type in healthy controls has been preserved ejection fraction (HFpEF) with (53.368 %). In the case of the comparison of the AST/ALT ratio and EF across all of the age groups that have been tested, the results suggest a significant level (P ≤ 0.050) relation between the ALP enzyme and EF for the patients within the (35-45 years) age group additionally, as there has been a positive and weak linear connection (r = 0.10650) and a nominal p-value (p = 0.47240) at a threshold of probability ≤ P 0.050, the link and correlation between the AST/ALT ratio and cardiac EF have been investigated.
Keywords: ALP enzyme, AMI patients, Ejection Fraction, AST \ ALT ratio.
INTRODUCTION
Worldwide, one of the significant causes of mortality is AMI 1. The patient's age is one of the essential factors diagnosed as a risk factor in AMI patients, as the death rate increases among patients, especially within the older age groups2. Elevated levels of liver enzymes are closely related to the development of the risk of cardiovascular disease (CVD). Their increase may lead to a rise in stenosis and thus lead to blood clots3. Elevated levels of ALP enzyme in the blood serum lead to vascular calcification and affect the heart's blood supply4. The increase in the rate of these calcifications increases the risk of developing cardiovascular diseases in the general population, especially in patients with acute myocardial infarction5. The AST/ALT ratio is considered a strong indicator of myocardial damage. It can be relied upon after a heart infarction as a rapid measurement vital sign available in clinical laboratories. It can be easily performed to diagnose patients at risk of developing CVD and can help prevent complications. After an MI6, AST/ALT ratio is commonly used as a marker of liver disease; in MI patients, elevated AST/ALT is often an indicator of myocardial damage 7. Ejection fraction or left ventricular ejection fraction (LVEF) is a medical term that refers to the ratio of the amount of blood ejected from the ventricle to the amount of blood remaining in the ventricle during a one-time ventricular contraction. The ejection fraction is usually measured only in the left ventricle as it pumps oxygen-rich blood to all cells of the body8; various patients are suffering from left ventricular dysfunction and post-heart attack heart failure, a high-risk long-term condition1. Left Ventricular Ejection Fraction (LVEF) after AMI is an important and reliable indicator for assessing the heart's integrity and ability to function properly9. The present study aims to determine the relationship and correlation between EF on echo-cardiography and liver function in acute myocardial infarction patients.
MATERIALS AND METHODS
Study Samples.
Between 1 January 2021 and 1 July 2021, 120 blood samples from AMI patients—60 as controls and 60 patients—of both sexes who were accepted to the cardiac surgery unit at AL- Salam teaching hospital, the intensive cardiac care unit, and outpatient clinics in Mosul City/Iraq, were collected. Samples have been divided into two groups (control and patients) and three age groups (35-45), (46-56) and (57-80) years for both genders (5 ml) of intravenous blood has been withdrawn for patients and healthy by medical syringes capacity (5ml). The samples were placed in a centrifuge quickly (3000 rpm) for 12 minutes for serum purposes. The serum was divided into several Eppendroff tubes and kept freezing at a temperature of (-20c) until the physiological and chemical tests were carried out.
Determination of Aspartate Transaminase (AST)
Principle
The concentration of (AST) enzyme activity in the blood serum has been measured using a kit supplied by the Italian company (Giesse Diagnostics) using a chemistry analyzer.
Determination of Alanine Aminotransferase Transaminase (ALT)
Principle
The concentration of the enzyme activity (ALT) in the blood serum has been measured using a ready-made estimation kit (Kit) supplied by the Italian company (Giesse Diagnostics) using a chemistry analyzer.
Determination of Alkaline Phosphatase (ALP)
Principle
The concentration of the enzyme activity (ALP) in the blood serum has been measured using a ready-made estimation kit (Kit) supplied by the Italian company (Giesse Diagnostics) using a chemistry analyzer. The alkaline Phosphatase enzyme is hydrolyzed to p-nitro phenyl phosphate (4-NPP) to produce (4-np) P-nitro phenol. The enzyme activity in the sample has been measured at a wavelength of 305 nm.
Assessment of Ejection Fraction in AMI Patients
Ejection fraction in acute myocardial infarction patients has been evaluated by Echocardiography (ECO) according to Simpson's method by measuring the area in simplicity and estimating the volume of content, and then calculating the area in contraction and then evaluating the size of the remaining ventricle by applying the following formula 10.
diastolic volume – systolic volume
EF = _________________________________________________
diastolic volume
Statistical Analysis
The SPSS v. 19 from IBM Company, US, has been used for all statistical analysis. P ≤ 0.05 are considered significant when using the x2 test to compare groups statistically.
RESULTS
According to Table 1's findings and Figure 1, patients with myocardial infarction who are between the ages of 35 and 45 had an EF rate of 52.41 %, which is close to the healthy control samples' EF rate of 51.344 %. In other words, heart failure in patients and healthy control samples has a preserved ejection fraction (HFpEF), whereas heart failure in elderly patients aged 57 to 80 years has a mid-range ejection fraction (HFmrEF). The rates between healthy samples and patients are also similar (43.048 % and 43.76 %, respectively).
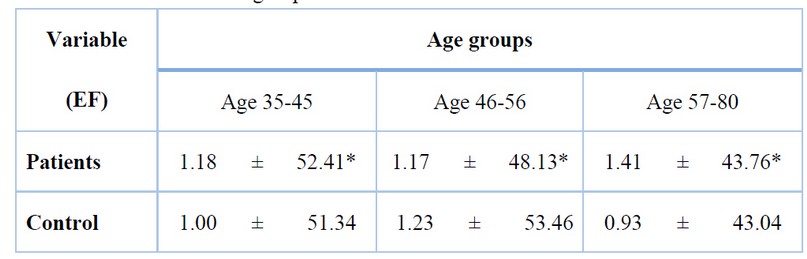
*Significant differences at P≤ 0.05, EF, Ejection Fraction
Table 1. Ejection fraction of patients and healthy people (control) for all age groups
The patients in the 46 to 56-year-old age range have an EF of heart failure with the mid-range EF type (HFmrEF), with a (48.13%) percentage, whereas the healthy control sample's ejection fracture is of the preserved ejection fraction type (HFpEF), with a percentage of (53.368 %).
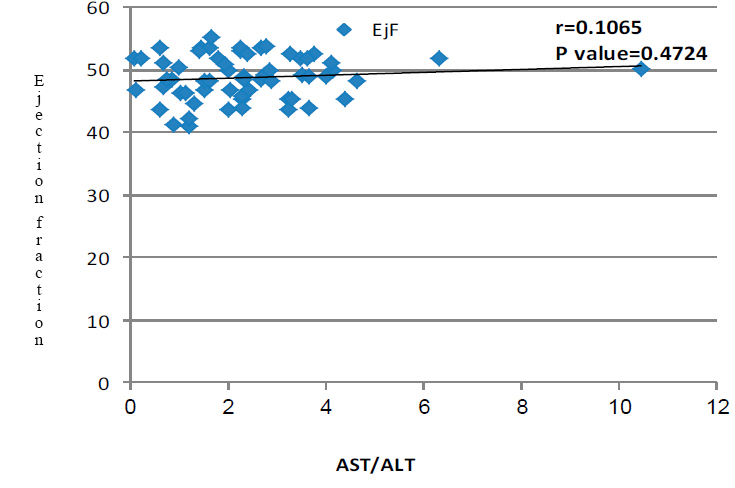
Figure 1. Ejection fracture of cardiac and healthy patients (control) for all age groups.
Relationship Between Liver Enzymes and Ejection Fraction
In the case when comparing the ratio of AST/ALT enzymes and the heart's ejection fraction across all age groups tested, the results, as presented in Table (2) demonstrate a significant level (P ≤ 0.050) association between the ALP enzyme and EF for the patients who are the age group (35-45 years). Results for the correlation and relationship between cardiac ejection fraction and AST/ALT enzymes are depicted in Figure 2. They reveal a weak and positive linear correlation (r = 0.10650) and no statistically significant differences (p = 0.4724) at a probability level of (P ≤ 0.050).
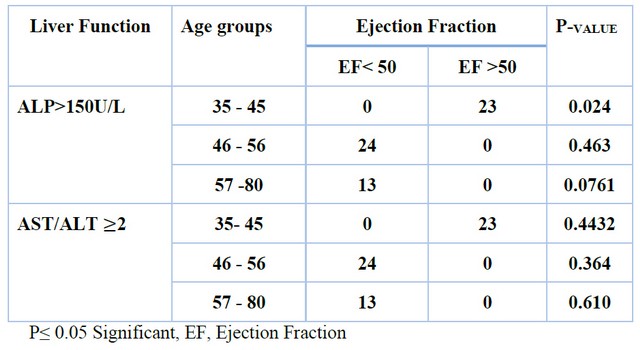
Table2. Correlation between liver enzymes and ejection fraction.
Figure 2. The correlation between ejection fraction and AST/ALT ratio.
DISCUSSION
The results of our study agree to some extent with many studies conducted to assess ejection fraction in patients, including patients with myocardial infarction11,12,13. Another study conducted by 14 to evaluate EF in patients with heart failure revealed that the elderly patients have preserved EF HFpEF, while the elderly patients in our study have a mid-range EF type HFmrEF. If the ejection fraction of the heart's left ventricle is ≤ 40%, it is considered heart failure with reduced ejection fraction (HFrEF). If the ejection fraction of the left ventricle of the heart is 40% and <50%, it is considered heart failure with mid-range ejection fraction (HFmrEF), but if the is LVEF ≤ 50%, it is considered a preserved ejection fraction HFpEF 11. so far, at present it remains ejection fraction EF is the first measure for diagnosing heart failure HF, one of the most common causes of which is a weakness or defect in the left ventricular muscle of the heart, which often occurs in patients with acute myocardial infarction12,15. HF and liver disease are among the most common mortality causes worldwide16. The heart's inability explains heart failure to sufficiently pump blood to all body organs due to a synthetic and functional heart disorder. Heart failure is measured by assessing the EF of the left ventricle of the heart LVEF15. An elevated AST/ALT ratio leads to an increased ejection fraction, and this convergence may be caused by the fact that patients are in the early stages of the disease. Many researchers in different countries117,118,19 have studied the correlation between liver defect and heart failure. The researcher 20 reveals that the deficiency in liver enzymes and the increased AST enzyme levels indicate heart failure that requires medical attention for hospital stewards. In the study conducted by researcher 21, there are normal levels of ALP enzyme or moderately high serum in patients, which disagrees with our study's results, as shown in Table (2). In a study conducted by the researcher19to find correlation between EF ejection fracture and liver functions in HF patients, he concludes that patients with ≤ 40% ejection fraction have an increase in the process of the liver by 92.50%, whereas there is an increase in the function of the liver by 61.7% in patients with ejection fraction > 40%.
The interaction between liver and heart diseases is predictable. There is a close interconnectedness between them, and the reason is that the liver receives 25% of the blood pumped by the heart22 and not only cardiovascular system is damaged by heart failure in the long term but the damage is done to the rest of the body organs and various tissues23,24. In a study conducted by the researcher15, it has been intended to create a relationship between EF and liver function in patients who have heart failure, by which it is concluded that the levels of ALP, ALT and AST enzymes are elevated in patients' serum who have an average ejection fraction ≤ 40% and lower levels in patients with an average ejection fraction > 40%. This is somewhat consistent with our findings, as shown in Table (2). Many studies have shown an increase or rise in ALP enzyme levels in the blood serum of HFpEF patients17,19,25. People with liver diseases related to heart failure are often not symptomatic for prolonged periods and are accompanied by a defect in liver enzymes or abnormal levels, which is the first sign of liver disease26,27,28,29.
CONCLUSIONS
The findings suggest that liver function and ejection fraction are related in those with AMI.
Author Contributions: The experiments were designed and carried out by all authors. The data were examined, and Duaa Mohammed Al-Nafoly wrote the manuscript. The article was read and approved by all the authors.
Funding: "This research received no external funding."
Institutional Review Board Statement: The Medical Research Ethics Committee at Mosul Univ. and Iraqi Medical Hospitals approved this work. The research's blood sample collection and all patient consent requirements have been approved. All patients' identities have been kept private as necessary.
Acknowledgments: The Dept. of Biology, College of Science, Univ. of Mosul, support this research. Many thanks to the nurses and doctors at the cardiac surgery unit at AL- Salam teaching hospital, the intensive cardiac care unit, and outpatient clinics in Mosul City/Iraq, who helped to complete the present research.
Conflicts of Interest: The funders did not have any impact on the design of this study; in the collection, analyses, or interpretation of data, manuscript writing, or decision to publish results.
REFERENCES
1.Teringova, E., Kozel, M., Knot, J., Kocka, V., Benesova, K., & Tousek, P. Relationship between TRAIL and left ventricular ejection fraction in patients with ST-elevation myocardial infarction treated with primary percutaneous coronary intervention. BioMed research international, 2018. https://doi.org/10.1155/2018/3709084
2.Li, J., Zhao, Z., Jiang, H., Jiang, M., Yu, G., & Li, X. . Predictive value of elevated alanine aminotransferase for in-hospital mortality in patients with acute myocardial infarction. BMC Cardiovascular Disorders,2021; 21(1), 1-9. https://doi.org/10.1186/s12872-021-01903-z
3.Baars, T., Sowa, J. P., Neumann, U., Hendricks, S., Jinawy, M., Kälsch, J., ... & Canbay, A. Liver parameters as part of a non-invasive model for prediction of all-cause mortality after myocardial infarction. Archives of Medical Science: AMS,2020; 16(1), 71-80. https://doi.org/10.5114/aoms.2018.75678
4.Edem, E. Relationship between alkaline phosphatase and impaired coronary flow in patients with ST-segment elevated myocardial infarction. Journal of International Medical Research,2018; 46(9), 3918-3927. https://doi.org/10.1177/0300060518785544
5.Wu, J. F., Jha, P., Doucette, S., & Abid, H. Significantly Elevated Alkaline Phosphatase Caused by Congestive Hepatopathy in the Setting of Heart Failure with Preserved Ejection Fraction. WMJ: Official Publication of the State Medical Society of Wisconsin,2022; 121(1), E14-E17.
6.Steininger, M., Winter, M. P., Reiberger, T., Koller, L., El-Hamid, F., Forster, S., ... & Sulzgruber, P. De-Ritis ratio improves long-term risk prediction after acute myocardial infarction. Journal of clinical medicine, 2018;7(12), 474. https://doi.org/10.3390/jcm7120474
7.Djakpo, D. K., Wang, Z. Q., & Shrestha, M. The significance of transaminase ratio (AST/ALT) in acute myocardial infarction. Archives of Medical Sciences. Atherosclerotic Diseases,2020; 5, e279. https://doi.org/10.5114/amsad.2020.103028
8.Ponikowski, P., Voors, A. A., Anker, S. D., Bueno, H., Cleland, J. G., Coats, A. J., ... & Van Der Meer, P. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Kardiologia Polska (Polish Heart Journal),2016; 74(10), 1037-1147.
9.Elkhader, B., Bala, A., & Omer, M. Assessment of ejection fraction in myocardial infarction patients after the use of beta-blockers. International Journal of Advanced Research in Biological Sciences,2014; 1(7): 30-35.
10.Yancy, C. W., Jessup, M., Bozkurt, B., Butler, J., Casey, D. E., Colvin, M. M., ... & Westlake, C. 2016 ACC/AHA/HFSA focused update on new pharmacological therapy for heart failure: an update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Journal of the American College of Cardiology,2016; 68(13), 1476-1488.
11.Park, C. S., Park, J. J., Mebazaa, A., Oh, I. Y., Park, H. A., Cho, H. J., ... & Choi, D. J. Characteristics, outcomes, and treatment of heart failure with improved ejection fraction. Journal of the American Heart Association,2019; 8(6), e011077. https://doi.org/10.1161/JAHA.118.011077
12.Ahmad, S. M. S., Farag, E. M., Eltahlawi, M. A., & Salama, A. E. Assessment of Left Ventricular Function by Global Longitudinal Strain in Patients with non-ST Elevation Myocardial Infarction. The Egyptian Journal of Hospital Medicine,2022; 86(1), 222-227. DOI: 10.21608/ejhm.2022.211054
13.Hedman, Å. K., Hage, C., Sharma, A., Brosnan, M. J., Buckbinder, L., Gan, L. M., ... & Lund, L. Identification of novel pheno-groups in heart failure with preserved ejection fraction using machine learning. Heart,2020; 106(5), 342-349. http://dx.doi.org/10.1136/heartjnl-2019-315481
14.Pastori, D., Ames, P. R., Triggiani, M., Ciampa, A., Cammisotto, V., Carnevale, R., ... & Athero-Aps Study Group. Antiphospholipid antibodies and heart failure with preserved ejection fraction. The multicenter athero-aps study. Journal of Clinical Medicine,2021; 10(14), 3180. https://doi.org/10.3390/jcm10143180
15. Lubis, I. H., Isnanta, R., & Safri, Z. Relationship Between The Ejection Fraction In Echocardiography With Liver Function In Heart Failure Patients. International Journal Of Scientific Research,2019,8(4),9-10.
16.Salah, H. M., Pandey, A., Soloveva, A., Abdelmalek, M. F., Diehl, A. M., Moylan, C. A., ... & Fudim, M. Relationship of Nonalcoholic Fatty Liver Disease and Heart Failure With Preserved Ejection Fraction. JACC: Basic to Translational Science,2021; 6(11), 918-932. https://doi.org/10.1016/j.jacbts.2021.07.010
17.Liang, W., He, X., Wu, D., Xue, R., Dong, B., Owusu-Agyeman, M., ... & Liu, C. Prognostic Implication of Liver Function Tests in Heart Failure With Preserved Ejection Fraction Without Chronic Hepatic Diseases: Insight From TOPCAT Trial. Frontiers in Cardiovascular Medicine,2021; 8, 330. https://doi.org/10.3389/fcvm.2021.618816
18.Drăghici, T., Negreanu, L., Bratu, O. G., Tincu, R., Socea, B., Iancu, M. A., ... & Diaconu, C. Liver abnormalities in patients with heart failure. Archives of the Balkan Medical Union,2018; 53(1), 76-81.
19.Sankar, K., Kumar, G. R., & Anandan, H. Correlation between ejection fraction and hepatic and renal functions in heart failure patients. INTERNATIONAL JOURNAL OF SCIENTIFIC STUDY,2016; 4(5), 164-167.
20.Vakilian, F., Rafighdoost, A. A., Rafighdoost, A. H., Amin, A., & Salehi, M. Liver enzymes and uric acid in acute heart failure. Research in Cardiovascular Medicine,2015; 4(4). doi: 10.5812/cardiovascmed.4(2)2015.22988
21.Dalos, D., Binder, C., Duca, F., Aschauer, S., Kammerlander, A., Hengstenberg, C., ... & Bonderman, D. Serum levels of gamma-glutamyltransferase predict outcome in heart failure with preserved ejection fraction. Scientific Reports,2019; 9(1), 1-9. https://doi.org/10.1038/s41598-019-55116-8
22.Carvalho, M. V. H., Kroll, P. C., Kroll, R. T. M., & Carvalho, V. N. Cirrhotic cardiomyopathy: the liver affects the heart. Brazilian Journal of Medical and Biological Research,2019; 52. https://doi.org/10.1590/1414-431X20187809
23.Ezzat, M. A., Boghdady, A. M., Ibrahim, K. F., & Dahab, L. H. A. Correlation between Serum Uric Acid Level and Left Ventricular Ejection Fraction in Patients with Congestive Heart Failure. World Journal of Cardiovascular Diseases,2019; 9(11), 857.doi: 10.21608/SMJ.2018.34708
24.Savarese, G., & Lund, L. H. Global public health burden of heart failure. Cardiac failure review,2017; 3(1), 7. doi: 10.15420/cfr.2016:25:2
25.Shamban, L., Patel, B., & Williams, M. (2014). Significantly elevated liver alkaline phosphatase in congestive heart failure. Gastroenterology research, 7(2), 64. doi: 10.14740/gr600w
26.Vélez-Paez JL, Montalvo MP, Esteban Jara F, Aguayo-Moscoso S, Tercero-Martínez W, Stalin Saltos L, Jiménez-Alulima G, Irigoyen-Mogro E, Castro-Reyes E, Mora-Coello C, López-Rondón E, Toapanta P, Vásconez-González E, Ortiz- Prado E. Predicting mortality in critically ill patients with COVID-19 in the ICU from a secondary-level hospital in Ecuador. Revis Bionatura, 2022;7(1) 1. http://dx.doi.org/10.21931/ RB/2022.07.01.1
27. Farhan, S. M., Abdulateef, S. M. Al-Enzy, A. F. M, Mohammed, Th. T., Saeid, Z. J. M., Al-Khalani, F. M. H. & Abdulateef, F. M. Effect of heat stress on blood alkalinity of broiler chicks and its reflection in improving the productive performance. Indian Journal of Ecology. 2020, 47: 107-109
28.Muwfaq Younis N , Efficacy of Health Beliefs Model-Based Intervention in Changing Substance Use Beliefs among Mosul University Students: A Randomized Controlled Trial. Revis Bionatura ,2022;7(2) 35. http://dx.doi.org/10.21931/RB/2022.07.02.35
29.Fathi Al-Obaidi R, Nazar Fadhel M, Rabeea Znad S. Evaluation of Heavy Metal Pollution in the Blood Serum of Industrial Workers, Mosul, Iraq. Revis Bionatura, 2022;7(2) 4. http://dx.doi.org/10.21931/RB/2022.07.02.4
Received: 20 July 2022 / Accepted: 15 October 2022 / Published:15 November 2022
Citation: Al-Nafoly D M, Alameen A M, Alshamaa S D. Evaluation of ejection fraction in patients with Acute Myocardial Infarction in Mosul City, Iraq. Revis Bionatura 2022;7(4) 14. http://dx.doi.org/10.21931/RB/2022.07.04.14
