2023.08.03.15
Files > Volume 8 > Vol 8 No 3 2023
1 Universidad Nacional de Chimborazo-Ecuador; [email protected].
2 Universidad Nacional de Chimborazo-Ecuador; [email protected].
3 Universidad Nacional de Chimborazo-Ecuador; [email protected].
4 Universidad Nacional de Chimborazo-Ecuador; [email protected].
* Correspondence: [email protected]
Available from: http://dx.doi.org/10.21931/RB/2023.08.03.15
ABSTRACT
The study aimed to analyze the theoretical references of obesity as a public health problem at the international level. Obesity has been associated with a high risk of chronic diseases such as hypertension, heart failure, and diabetes mellitus type II. However, it is unpredictable to calculate the social costs and losses of psychosocial well-being, causing stress and depression. However, to correctly treat this pathology that affects us so much, it is necessary to start with a correct and effective diagnosis, which should be carried out by physicians, nutritionists and other specialists in primary health care. To this end, a review of the literature on the subject was carried out in the databases of academic journals: Web of Science (Core Collection) Scopus, Medline through Pubmed and Scielo. Obesity is a severe social health problem since it affects many people worldwide, and only through scientific and technological development can it be adequately treated, diagnosed and prevented.
Keywords: obesity; health; quality of life; chronic diseases
INTRODUCTION
Science and technology are social processes, and their functioning and development are unthinkable without the social context that surrounds and conditions them. Obesity is a severe social health problem affecting many worldwide; it can only be adequately treated and prevented through scientific and technological development.
According to the World Health Organization (WHO)1, obesity is the most frequent chronic non-communicable disease, and being overweight is its precursor. It is defined as an "abnormal or excessive accumulation of body fat that may be detrimental to health" 1. There are more than 1 billion overweight adults worldwide, and according to this source, in 2015, the figure will reach 3 billion. Cuba is not free from this danger, and according to surveys conducted by the National Institute of Hygiene and Epidemiology, 15.44% of women are obese, and 31.5% are overweight. It is then the female sex the most affected and the one that suffers and worries the most about this disease, according to several studies 2,3.
This pathology has been associated with a high risk of chronic diseases such as hypertension, heart failure, and type II diabetes mellitus. However, it is unpredictable to calculate the social costs and the loss of psychosocial well-being caused by stress and depression. However, to correctly treat this pathology that affects us so much, it is necessary to start with a correct and effective diagnosis, which should be carried out by physicians, nutritionists and other specialists in primary health care 2-4.
Defining obesity as a body weight above the values considered normal for height would be incorrect and far from the actual concept of obesity since body fat is only one component of total body weight. Obesity, especially central obesity, is associated with chronic non-communicable diseases, and the association is independent of hypertension, diabetes and metabolic syndrome 5.
The indicator used and validated to evaluate obesity in adults is the Body Mass Index (BMI BMI), but this has several difficulties in the sense that what it evaluates is overweight and not obesity. On the other hand, other indicators, such as waist circumference (WCWC) and waist height index (WHIWHI), have yet to be studied in these populations. Specifically, the latter has been even less studied and could be a valuable and effective method for determining obesity. The ECIECI in Asian studies (in Chinese adults) is a better indicator of coronary risk factors, dyslipidemias and type 2 diabetes than other anthropometric indicators such as BMIBMI, CC and Hip-Waist Index in some epidemiological studies. The results indicated that the ECIECI could be an optimal anthropometric predictor of metabolic syndrome risk factors 6-12.
Based on these assessments, the following objective of the study is proposed: to analyze the theoretical references of obesity and overweight as a public health problem at the international level.
MATERIALS AND METHODS
The search strategies were based on the authors' descriptive terms and keywords: scientific production, health, scientific articles, and databases, in Spanish and English. The search was performed in Spanish and English using the same methodology. These keywords were combined from the following academic journal databases: Web of Science (Core Collection), Scopus, Medline through Pubmed and Scielo.
The advanced metasearch option was performed using the resources inherent to each database. The search strategy was carried out by two independent, blinded reviewers, who performed the initial search using the list of keywords prepared for this analysis by the authors who wrote the article.
The following screening procedures were applied to determine whether the articles obtained in the initial searches were relevant to the present study: a) reading the titles: if the titles appeared relevant, all duplicates would be eliminated after the initial review; b) reading the abstracts: if the abstracts did not provide sufficient information related to the inclusion criteria, they would be excluded from the study; c) reading the full-text articles.
RESULTS AND DISCUSSION
Adults between 20 and 60 years of age comprise the age group on which the capacity for production and services is almost totally based and on which those under 20 years of age depend for the most part, a group made up to a large extent of individuals in training both from a physical and intellectual point of view, as well as those over 60 years of age, also made up of a more significant proportion of individuals who are not incorporated into production or services because they have retired from these activities. That is why the nutritional evaluation of this group, whose social importance is indisputable, acquires excellent relevance in the study of any population from the point of view of their state of health 13.
Obesity in women has peculiar nuances that are beginning to be understood. The higher prevalence of obesity in women is a product of biological and psychological characteristics and social situations. Biological factors. Compared to men, the higher percentage of fat mass in women determines a lower energy expenditure per kilogram of weight, which makes it more challenging to lose the excess weight gained. Pregnancies favor obesity, as suggested by data showing an association between the number of pregnancies and the development of obesity. Menopause has unfavorable effects on body composition, leading to an increase in obesity between the ages of 40 and 60, mainly if the necessary adjustments in energy balance are not made—psychological factors. Women have a higher prevalence of eating disorders. Some studies show a higher prevalence of depression and anxiety among women with obesity. These psychological factors are both cause and consequence of obesity 14.
Effect of the environment. The "obesogenic" environment may have a more significant effect on women because the portions they eat are usually greater than their needs since their energy requirements are lower than those of men due to their phenotype and activity level 15.
According to the World Health Organization (WHO), obesity is the world's most common chronic non-communicable disease, called "The Epidemic of the 21st Century". 2005, there were 400 million obese adults, and in 2015, the figure may reach more than 700 million. If we add to this figure the number of overweight people, which will reach 3 billion, we will realize the importance of this disease. In Cuba, 7.95% of men and 15.44% of women are obese, while 29.7% of men and 31.5% of women are overweight 1-14.
However, what is obesity?
Overweight and obesity are defined as an abnormal or excessive accumulation of fat that can be detrimental to health 1,15.
Facts about overweight and obesity
Overweight and obesity are the fifth leading risk factor for death worldwide. At least 2.8 million adults die annually due to being overweight or obese. In addition, 44% of the burden of diabetes, 23% of the burden of ischemic heart disease and between 7% and 41% of the burden of some cancers are attributable to overweight and obesity 16.
Anthropological configuration of obesity
The word "obese" comes from the Latin "obedere". Formed from the roots ob (over, or all-embracing) and here (to eat), i.e., "someone who eats everything." The first known use of this word was in 1651 in English, in a medical book by Noha Biggs (Biggs, Noha (fl. 1651), medical practitioner and social reformer)17.
From an anthropological point of view, obesity became a problem approximately 10,000 years ago, particularly with the emergence of agricultural art, with which nomadic life was abandoned and civilization began, although with little incidence due to the physical labor that existed and whose particularity was intense. However, this problem intensified with the advent of the Industrial Revolution18.
From a socio-anthropological context, obesity has been observed from two perspectives, as a favorable adaptive condition or an ailment, depending on how the provision of reserves impacts as a protective factor in the face of food shortage or crystallizes in a metabolic overload. In one way or another, obesity has been present in the history of humanity, with a changing social significance according to the characteristics and conditions of life in the different evolutionary moments of humanity. Especially 200 years ago, when a very preponderant capacity arose for societies to produce, collect and distribute food regularly, which decreased famines and tacitly began the epidemic of obesity, a product of the ways of acting of individuals concerning disorderly consumption or excess of food for various cultural, religious or customary characteristics, in which the act of eating came to have interpretations or negative connotations. This system of interrelationships, which incorporates the experiences, ideas and perceptions of the members of society, influence the biological, psychosocial and cultural factors that influence their eating pattern and perception of body image 16-19.
Obesity, as a sociocultural expression, has become an epidemic that demands from society general strategies that include preventive and control activities, which should focus on reducing exposure to an environment that favors the development of this disease. Particularly leading to more excellent knowledge of the population about the determinants and whose geographical variation and cultural diversity predispose this susceptibility to weight gain among people. Culture refers to learned behavior patterns and beliefs, characteristic of a society or social group. It includes values of all kinds, from food, the means of production, and the management of its economy to ideological elements such as body aesthetics, which must be permanently modified to reduce obesity.
Medical approach to obesity as a disease
The medical approach to obesity has predominated in the 20th and 21st centuries, where obesity and overweight have been characterized as a clinical public health entity that requires treatment and prevention, as well as the identification of risk factors with food in the foreground and its relationship with a large number of chronic diseases, a decrease in life expectancy and an increase in mortality in people who suffer from it 20.
Obesity is a health problem of enormous dimensions that reaches epidemiological significance and extends to large masses, regardless of race, sex, age, social status, economic solvency and other factors.
In the last 20-30 years, overweight and obesity threaten the world's entire population. Enormous budgets are allocated for their prevention and control. However, the numbers are increasing unchecked, without the intervention policies of governmental and non-governmental institutions and organizations achieving the desired success. However, at the same time, great efforts are being made to achieve scientific advances that provide promising results. The influence of eating habits on obesity, genetic factors, the role played by lifestyle, in particular, the systematic practice of physical exercise through an active life, the discovery of neurophysiological mechanisms of food consumption control and the existence of drugs that stimulate appetite or depress it have been demonstrated, the incidence of social and psychological factors that condition psychiatric diseases, such as the unbridled appetite of bulimia, and surgical treatments such as liposuction or gastric interventions to reduce stomach capacity 18-21.
All this intemperance of obesity and tendencies to be overweight have undoubtedly come along with the advances brought about by a "civilized," "developed," "modern," and "fast" society. Let us analyze the medical approach to obesity in history. It is evident that before the 20th century and especially the 21st century, obesity did not represent or manifest itself with the importance, incidence and transcendence that it has reached in today's world.
Although Hippocrates (460-377? b.c. ) and his disciple Galen (129-216) made mention of obesity in their texts associated with infertility in women, sudden death and other disorders with recommendations for frequent and vigorous physical exercise, restriction of food and consumption of certain foods to control appetite, it is preferred that the first text where obesity is the main topic appeared in the XVII century, a time when the human models of mechanistic medicine predominated, where obesity is related to gastrointestinal fermentation and putrefaction disorders regulated by chemical reactions 21.
In the 18th century, under the predominance of medical trends led by the Dutchman H. Boeerhaave (1688-1738) and his disciples, the published monographs on obesity referred to the lack of balance of the human body systems and its influence on obesity. In this regard, light diets and physical exercise were recommended. Later, still under the importance of European medicine and with the advances in thermodynamics, the concept of energy balance significantly influenced the appearance of dietary recommendations to treat or prevent obesity 22.
In the first part of the 20th century, the fat cell or lipocyte was identified in Germany and with it, the relationship between obesity and the endocrine system. This is the period in which the hormonal approach to obesity was very influential, with some attributing a metabolic origin. Years later, in 1994, leptin was discovered in the mouse, and subsequent studies related this peptide, synthesized mainly in adipose tissue, to body fat, the size of adipose cells, the functions of regulating food intake, and the body's energy balance. This becomes particularly important, considering, among other factors, that serum leptin levels are much higher in obese people with body mass index (BMI BMI) above 30 than in people of average weight. Thus, the circulating levels of leptin are much higher in obese people with body mass indexes (BMI BMI) above 30 than in people of average weight. Thus, circulating leptin levels in the blood increase as body fat increases 20-22.
In the present 21st century, the multifactorial orientation of obesity stands out since this disease only has a predominantly endocrine or genetic origin in a minority of people, and the factors of imbalance between energy consumption and expenditure from uncontrolled food intake prevail.
Obesity and overweight. World prevalence
The geometric progression that characterizes the increase of obesity and overweight in the adult population requires multidisciplinary attention, in which physical activity is a fundamental pillar of its prevention and treatment. According to the World Health Organization (WHO), obesity is the most frequent chronic non-communicable disease, and overweight is its precursor. Its March 2011 report defines it as an "abnormal or excessive accumulation of body fat that can be harmful to health." Globally, there are more than 1 billion overweight adults, and according to this source, by 2015, the figure will reach 3 billion 23.
Obesity was considered a worldwide epidemic by the World Health Organization (WHO) in 1998 because globally, there are over one billion overweight adults, and at least 300 million are obese. It affects children and adults, especially women, both in developed and developing countries; in the latter, there is a "double burden of disease" or face a double challenge, obesity along with malnutrition problems. This "double burden" is a consequence of several factors, among which the modification of eating patterns and lifestyles due to migration to urban areas, demographic changes and the decrease in physical activity stand out 24.
It was not until 1999 that the Milan Declaration was published, in which the countries belonging to the European Union assumed that obesity constitutes a fundamental disorder from which comorbidities of all kinds (cardiac, rheumatological, digestive, endocrine, etc.) develop. In 2002, the World Health Organization, in its resolution WHA 55.23, developed the Global Strategy on Diet, Physical Activity and Health, which was approved by the member states in May 2004 (Resolution WHA 57.17), at which time obesity was labeled as the "epidemic of the 21st century" 25.
In Latin American countries, there are worrying levels of obesity and overweight prevalence 26, as shown in Table 1.
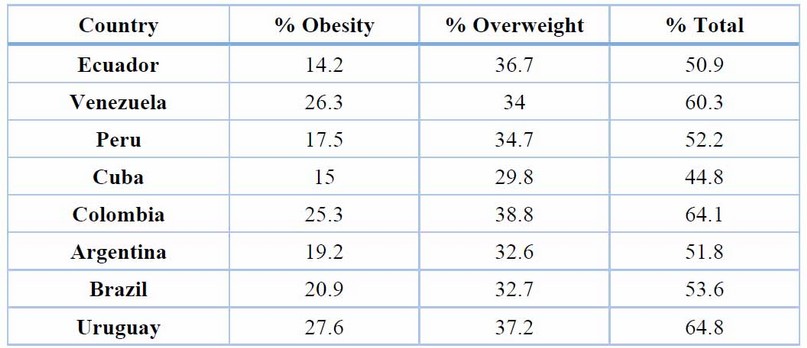
Table 1. Prevalence of overweight and obesity in some Latin American countries 26
Other countries also report high and worrying levels of obesity 26-28 (see Table 2).
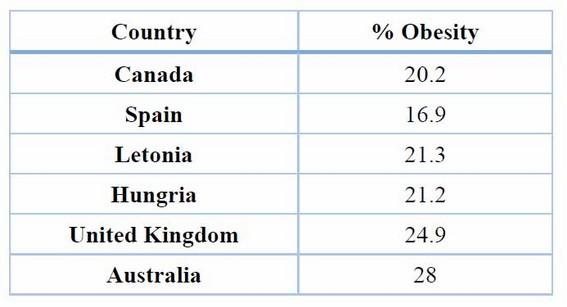
Table 2. Prevalence of overweight and obesity in other countries of the world 26-28
Social changes and sedentary lifestyles
Several social influences are driving the environmental changes implicated in the obesity epidemic. These include modernization, increasing urbanization, scientific and technical development, and changes in types of employment. Although these factors are considered social advances, they have also caused negative changes, such as urban overcrowding and the breakdown of traditional family values. In most countries, urbanization has significantly affected physical activity levels. It has led to lower consumption of complex carbohydrates and higher levels of fat and animal products, more sugar, more processed food and more food consumed outside the home 29.
Significant variations in the structure of the type of jobs worldwide have occurred, with a massive shift towards jobs that require less physical exercise. In developing countries, there has been a shift in recent years towards knowledge-based employment that is much less dependent on physical activity. Jobs have become less physically demanding, and the proportion of people working in agriculture, services and industry is declining, as is the type of work performed in most occupations. The increasing use of automated transportation, technological advances in the performance of household chores, and the search for more idle ways to spend leisure time have also contributed to sedentary lifestyles. Thus, the increase in the number of hours spent in front of the computer or television and the decrease in the use of bicycles as a means of transportation are clear examples that explain the persistent change in the energy balance that favors the prevalence of obesity 30.
There are already identified groups at increased risk of weight gain and obesity due to biological, genetic, lifestyle, etc. These include a family history of obesity, smoking cessation, excessive alcohol consumption, some pharmacological treatments, certain diseases and changes in social circumstances.
Consequences of obesity
A higher frequency of obesity is described in people with ischemic heart disease. There is no doubt that in the obese, and particularly in those with morbid obesity or with abdominal predominance, other additional risk factors are associated, such as arterial hypertension, type 2 diabetes mellitus (non-insulin-dependent), insulin resistance and hyperinsulinism, dyslipidemia (alterations in blood fats), among others, which are closely related to the development of accelerated atherosclerosis and all its consequences.
Multiple national and international studies have shown that arterial hypertension is associated with obesity (particularly abdominal obesity), advanced age and decreased physical activity. The prevalence of arterial hypertension can reach figures close to 80% in the obese population 31-33.
The accelerated atherosclerosis observed in obese people explains why obese people frequently develop cerebral infarction or cerebral hemorrhages, severe situations that can endanger the patient's life. Obesity compromises venous circulation, which favors the development of edema and varicose veins of the lower limbs, as well as hemorrhoids and thromboembolic disease of the lower limbs and vena cava 34.
Obesity can compromise respiratory function, a compromise that is greater the more severe the obesity. In obese individuals, a decrease in lung volume is usually confirmed. In people with morbid (severe) obesity, there is hypoventilation of the pulmonary alveoli, which predisposes to pulmonary infections, breathing difficulties, drowsiness, and increased concentration of carbon dioxide (CO2) in the blood. The latter can cause a state of acidosis and favor the development of congestive heart failure 35.
The strong correlation between obesity and type 2 (non-insulin-dependent) diabetes is well known. Obesity is the most potent known risk factor for developing type 2 diabetes. The severity and duration of obesity are two important considerations. Obesity contributes to the development of diabetes by promoting insulin resistance. Resistance has significant pathophysiological effects on the development of type 2 diabetes, hypertension and metabolic syndrome 36.
The Journal of Clinical Endocrinology & Metabolism study clearly states these complex consequences 37 (see Figure 1).
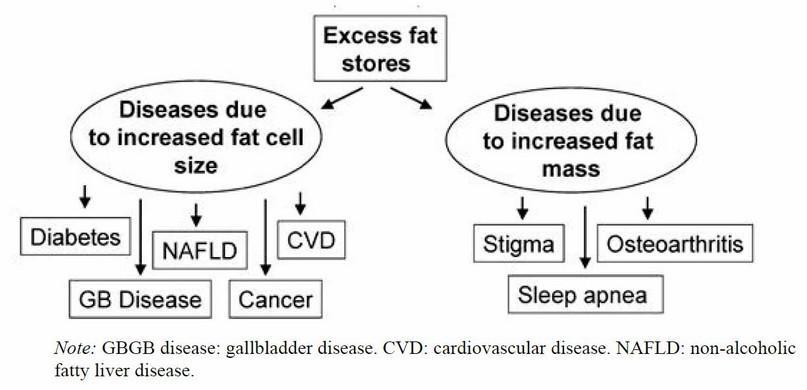
Figure 1. Some health consequences of obesity 37
Studies conducted in the United States 38-46 identified some determinants and consequences of obesity. Weight gain and overweight or obesity were shown to be significant risk factors for type 2 diabetes, cardiovascular disease, certain cancers and premature death. Cohorts have elucidated the role of dietary and lifestyle factors in obesity, especially sugar-sweetened beverages, poor diet quality, and physical inactivity. Genome-wide association and gene-lifestyle interaction studies have shown that genetic factors predispose to obesity but that this susceptibility can be attenuated by healthy lifestyle choices (see Figure 2).
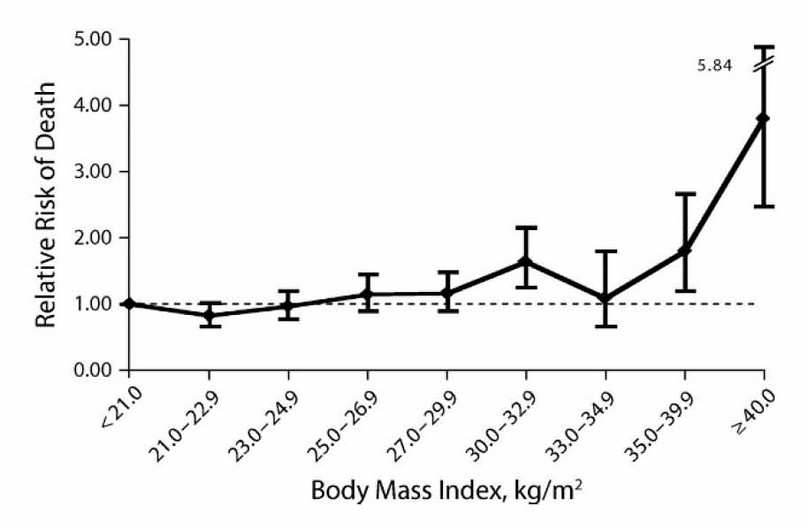
Figure 2. The relative risk of death from different causes according to body mass index in the United States 38
The pathology of obesity produces a myriad of health-related problems. These health-related problems can be attributed to either the increased mass of fat or the increased release of peptides from enlarged fat cells. CVD, Cardiovascular disease; GBGB, gallbladder.
In the skin of obese people, different alterations can be frequently observed, among which are acanthosis nigricans (blackish spots in regions of the body where there are folds, e.g., neck, armpit), hirsutism (an increase of body hair in unusual areas), intertrigo (infections usually caused by fungi in areas of folds, furunculosis, plantar calluses due to excess weight and multiple papillomas. As a result of the increase in body weight, the joints may be compromised. It is common in these individuals to confirm osteoarthritis of the knees and spine, a higher frequency of heel spurs, and hip disorders (coxavara, epiphysiolysis of the femoral head). In those with postural defects, these are often aggravated (flat feet, scoliosis, varus genus) 47,48.
Endometrial, breast, colon and gallbladder cancer incidence is increased in obese women. Obese men suffer more colon and prostate cancer when compared to non-obese people. A higher risk of obstetric complications has been described in obese women, including toxemia, arterial hypertension, gestational diabetes, prolonged labor and frequent cesarean sections 49.
Psychosocial problems These disorders are more relevant the more significant the severity of obesity. The deterioration of self-image and difficulties in social communication should be highlighted. Not infrequently, these people are socially and economically discriminated against and, therefore, have more significant abstention from work. Depending on the degree of obesity, the mobility of these people may be compromised. The above can make these people more susceptible to developing psychoneurotic states 50.
CONCLUSIONS
Obesity is a severe social health problem since it affects many people worldwide, and only through scientific and technological development can it be adequately treated, diagnosed and prevented. Despite the great variety of existing anthropometric indicators to diagnose obesity in adults, all of them have difficulties with their application and generalization. It is, therefore, necessary to develop research to validate new indicators adjusted to the characteristics of the population being evaluated.
Author Contributions: A short paragraph specifying their contributions must be provided for research articles with several authors. The following statements should be used: "Conceptualization, YRRYRR; methodology, YRRYRR; software, MOPMOP; validation, YRRYRR, and MOPMOP; formal analysis, YRRYRR and BLGBLG; investigation, YRRYRR; resources, FMLFML; data curation, MOPMOP; writing—original draft preparation, YRRYRR and MOPMOP; writing—review and editing, YRRYRR; visualization, MOPMOP; supervision, YRRYRR; project administration, YRRYRR All authors have read and agreed to the published version of the manuscript." Please turn to the CRediT taxonomy for the term explanation. Authorship must be limited to those who have contributed substantially to the work reported.
Funding: "This research received no external funding."
Institutional Review Board Statement: "Not applicable."
Informed Consent Statement: "Not applicable."
Conflicts of Interest: "The authors declare no conflict of interest."
REFERENCES
1. Organización Mundial de la Salud. [Internet]. Washinton; 2022-03 [actualizado 2023 may 12]. Disponible en: http://www.who.org/.
2. Pérez Moreno J, de la Mata Navazo S, López-Herce Arteta E, Tolín Hernani M, González Martínez F, González Sánchez MI, Rodríguez Fernández R. Influencia del estado nutricional en la evolución clínica del niño hospitalizado. An Pediatr (Engl Ed). 2019;91(5):328-335.
3. Rubio MA, Salas-Salvado J, Barbany M, Moreno B, Aranceta J, Bellido D, et al. Consenso SEEDO 2007 para la evaluación del sobrepeso y la obesidad el establecimiento de criterios de intervención terapéutica. Rev Esp Obes. 2007; 7-48
4. Saraf-Bank S, Ahmadi A, Paknahad Z, Maracy M, Nourian M. Effects of curcumin on cardiovascular risk factors in obese and overweight adolescent girls: a randomized clinical trial. Sao Paulo Med J. 2019 Sep-Oct;137(5):414-422.
5. Lim LL, Seubsman SA. Validity of self-reported abdominal obesity in Thai adults: A comparison of waist circumference, waist-to-hip ratio and waist-to-stature ratio. Nutr Metab Cardiovasc Dis. 2010; 14(4).
6. Lean, EJEJ. Waist circumference as a measure for indicating the need for weight management, BMJBMJ. 1995; 311:158-161.
7. Silveira EA, Mendonça CR, Delpino FM, Souza GVE. Sedentary behavior, physical inactivity, abdominal obesity and obesity in adults and older adults: A systematic review and meta-analysis. Clinical nutrition ESPEN. 2022; 50: 63-73.
8. Donini LM, Busetto L, Bischoff SC, Cederholm T, Ballesteros-Pomar MD, Batsis JA, Barazzoni R. Definition and diagnostic criteria for sarcopenic obesity: ESPEN and EASO consensus statement. Obesity facts. 2022; 15(3): 321-335.
9. Romain AJ, Marleau J, Baillot A. Association between physical multimorbidity, body mass index and mental health/disorders in a representative sample of people with obesity. J Epidemiol Community Health. 2019; 73(9): 874-880.
10. Gómez-del-Río N, González-González CS, Toledo-Delgado PA, Muñoz-Cruz V, García-Peñalvo F. Health promotion for childhood obesity: An approach based on self-tracking of data. Sensors. 2020; 20(13): 3778.
11. Sasaki E, Ota S, Chiba D, Kimura Y, Sasaki S, Yamamoto Y, Ishibashi Y. Early knee osteoarthritis prevalence is highest among middle-aged adults with obesity based on a new set of diagnostic criteria from a large sample cohort study in the Japanese general population. Knee Surgery, Sports Traumatology, Arthroscopy. 2020; 28: 984-994.
12. Tutunchi H, Ebrahimi-Mameghani M, Ostadrahimi A, Asghari-Jafarabadi M. What are the optimal cut-off points of anthropometric indices for prediction of overweight and obesity? Predictive validity of waist circumference, waist-to-hip and waist-to-height ratios. Health promotion perspectives. 2020; 10(2): 142.
13. Rubino D, Abrahamsson N, Davies M, Hesse D, Greenway FL, Jensen C, Lingvay I, Mosenzon O, Rosenstock J, Rubio MA, Rudofsky G, Tadayon S, Wadden TA, Dicker D; STEP 4 Investigators. Effect of Continued Weekly Subcutaneous Semaglutide vs Placebo on Weight Loss Maintenance in Adults with Overweight or Obesity: The STEP 4 Randomized Clinical Trial. JAMA. 2021 Apr 13;325(14):1414-1425.
14. Zaki M, Robaayah Z. Malaysia Shape of the Nation: a primary care-based study of abdominal obesity in Malaysia. B. Med J Malaysia. 2010; Jun; 65 Suppl A: 143-9.
15. Patil VC, Parale GP. Generalized and abdominal adiposity are important risk factors for chronic disease in older people: results from a nationally representative survey. J Nutr Health Aging. 2011; 15(6):469-78.
16. Molina-Luque R, Romero-Saldaña M, Álvarez-Fernández C, Rodríguez-Guerrero E, Hernández-Reyes A, Molina-Recio G. Waist to Height Ratio and Metabolic Syndrome as lung dysfunction predictors. Sci Rep. 2020 Apr 29;10(1):7212.
17. Vaquero-Álvarez M, Molina-Luque R, Fonseca-Pozo FJ, Molina-Recio G, López-Miranda J, Romero-Saldaña M. Diagnostic Precision of Anthropometric Variables for the Detection of Hypertension in Children and Adolescents. Int J Environ Res Public Health. 2020 Jun 19;17(12):4415.
18. Han TS. Waist circumference predicts intra-abdominal fat better than waist-to-hip ratio in women. Proc Nutrition Soc. 1995; 54:152.
19. Poletto JE, Rizzo DT, Almeida AMN, Cândido EC, Cazzo E, Chaim ÉA. Evolution of anthropometric data and quality of life in active bariatric individuals. Rev Assoc Med Bras. 2021 Sep;67(9):1274-1278.
20. Żurawiecka M, Wronka I. Association between age at menarche and body mass index, waist circumference, waist to hip ratio, and waist to height ratio in adult women. Am J Hum Biol. 2021 Nov;33(6): e23523.
21. Özkaya İ. Nutritional status of the free-living elderly. Cent Eur J Public Health. 2021 Mar;29(1):68-75.
22. Booth ML, Hunter C. The relationship between body mass index and waist circumference: implications for estimates of the population prevalence of overweight. Int J Obes Relat Metab Disord. 2000; Aug;24(8):1058-61
23. Hsieh T. La relación cintura y estatura como simple índice antropométrico para identificar riesgo metabólico, Internac J of Obesity. 2003; 27(5): 610-616
24. Shao J, Yu L. Waist-to-height ratio, an optimal predictor for obesity and metabolic syndrome in Chinese adults. J Nutr Health Aging. 2010; Nov;14(9):782-5.
25. Wei J, Liu X, Xue H, Wang Y, Shi Z. Comparisons of Visceral Adiposity Index, Body Shape Index, Body Mass Index and Waist Circumference and Their Associations with Diabetes Mellitus in Adults. Nutrients. 2019 Jul 12;11(7): 1580.
26. Hernández-Rodríguez J, Domínguez YA, Moncada-Espinal OM. Prevalencia y tendencia actual del sobrepeso y la obesidad en personas adultas en el mundo. Rev cubana Endocrinol. 2019; 30(3): e193. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1561-29532019000300009&lng=es.
27. Colectivo de autores. II Consenso Latinoamericano de Obesidad 2017. Federación Latinoamericana de Sociedades de Obesidad. [Internet] 2017 [citado 30/05/2017]; 144 págs. Disponible en: http://fliphtml5.com/hvov/cxpr/basic
28. World Obesity Federation. World Obesity Atlas 2023. https://data.worldobesity.org/publications/?cat=19
29. Rosales Ricardo Y. Evaluaciones antropométricas en mujeres obesas. Saarbrücken. Editorial Académica Española; 2011.
30. Bojanic D, Ljubojevic M, Krivokapic D, Gontarev S. Waist circumference, waist-to-hip ratio, and waist-to-height ratio reference percentiles for abdominal obesity among Macedonian adolescents. Nutr Hosp. 2020 Aug 27;37(4):786-793.
31. He YH, Chen YC. Evaluation of anthropometric indices for metabolic syndrome in Chinese adults aged 40 years and over. Eur J Nutr. 2011; Apr 11.
32. Kulkarni PM, Patil HV. Relation of anthropometric variables to coronary artery disease risk factors. Indian J Endocrinol Metab. 2011; Jan; 15(1):31-7.
33. Zhang FL, Ren JX, Zhang P, Jin H, Qu Y, Yu Y, Guo ZN, Yang Y. Strong Association of Waist Circumference (WCWC), Body Mass Index (BMIBMI), Waist-to-Height Ratio (WHtR), and Waist-to-Hip Ratio (WHRWHR) with Diabetes: A Population-Based Cross-Sectional Study in Jilin Province, China. J Diabetes Res. 2021; 2021:8812431.
34. Oumer A, Ale A, Tariku Z, Hamza A, Abera L, Seifu A. Waist-to-hip circumference and waist-to-height ratio could strongly predict glycemic control than body mass index among adult patients with diabetes in Ethiopia: ROCROC analysis. PLoS One. 2022 Nov 9;17(11): e0273786.
35. Shao J, Yu L. Waist-to-Height Ratio, an Optimal Predictor for Obesity and Metabolic Syndrome in Chinese Adults. J Nutr Health Aging. 2010; 14(9):782-5.
36. Rakesh M. Limit your waist size to half of your height. Indian J Endocrinol Metab. 2011; Jul-Sep; 15(3): 228–229.
37. George AB. Medical Consequences of Obesity. The Journal of Clinical Endocrinology & Metabolism. 2004; 89 (6): 2583–2589. https://doi.org/10.1210/jc.2004-0535
38. Hruby A. Determinants and Consequences of Obesity. American Journal of Public Health. 2016; 106(9): 1656-1662. https://doi.org/10.2105/AJPH.2016.303326
39. Demeulemeester F, de Punder K, van Heijningen M, van Doesburg F. Obesity as a risk factor for severe COVID-19 and complications: a review. Cells. 2021; 10(4): 933.
40. Raud B, Gay C, Guiguet-Auclair C, Bonnin A, Gerbaud L, Pereira B, Coudeyre E. Level of obesity is directly associated with the clinical and functional consequences of knee osteoarthritis. Scientific reports. 2020; 10(1): 3601.
41. Hong SH, Choi KM. Sarcopenic obesity, insulin resistance, and their implications in cardiovascular and metabolic consequences. International journal of molecular sciences. 2020; 21(2): 494.
42. Jastreboff AM, Kotz CM, Kahan S, Kelly AS, Heymsfield SB. Obesity as a disease: the obesity society 2018 position statement. Obesity. 2019; 27(1): 7-9.
43. Pillon, N. J., Loos, R. J., Marshall, S. M., & Zierath, J. R. (2021). Metabolic consequences of obesity and type 2 diabetes: Balancing genes and environment for personalized care. Cell, 184(6), 1530-1544.
44. Hojjat, T. A., & Hojjat, T. A. (2021). Consequences of Obesity. The Economics of Obesity: Poverty, Income Inequality, and Health, 21-26.
45. Endalifer, M. L., & Diress, G. (2020). Epidemiology, predisposing factors, biomarkers, and prevention mechanism of obesity: a systematic review. Journal of Obesity, 2020.
46. Tsatsoulis, A., & Paschou, S. A. (2020). Metabolically healthy obesity: criteria, epidemiology, controversies, and consequences. Current obesity reports, 9, 109-120.
47. Lee HS, Lee J. Influences of Ketogenic Diet on Body Fat Percentage, Respiratory Exchange Rate, and Total Cholesterol in Athletes: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2021 Mar 12;18(6):2912.
48. Bergman R. A better index of body adiposity. Obesity, 2011; 9(5).
49. Durá-Travé T, Gallinas-Victoriano F, Malumbres Chacón M, Moreno González P, Ahmed-Mohamed L, Urretavizcaya-Martínez M. Reference values of fat mass index and fat-free mass index in healthy Spanish adolescents. Nutr Hosp. 2020 Oct 21;37(5):902-908.
50. Kocaadam-Bozkurt B, Karaçil Ermumcu MŞ, Erdoğan Gövez N, Bozkurt O, Akpinar Ş, Mengi Çelik Ö, Köksal E, Acar Tek N. Association between adherence to the Mediterranean diet with anthropometric measurements and nutritional status in adolescents. Nutr Hosp. 2023 Apr 20;40(2):368-376.
Received: 28 May 2023/ Accepted: 15 July 2023 / Published:15 September 2023
Citation: Rosales-Ricardo Y, Ortiz-Perez M, Lopez-Merino F and Perez-Garcia B. Obesity and overweight as an international public health problem. Revis Bionatura 2023;8 (3) 15. http://dx.doi.org/10.21931/RB/2023.08.03.15
