2023.08.03.86
Files > Volume 8 > Vol 8 No 3 2023
Insulin resistance profile as an indicator for Incidence of thyroid cancer
Ali, Reda Hussein*; Sanaa Jameel Thamer1 ; Dhamia Kasim Suker2; Majid Hameed Abbood3; Rafid R. Al-Tuma4; Loma Al-Mansouri5
*PhD student, Physiology/Biology Department, College of Sciences, Basrah University, Iraq; [email protected]. ORCID 0000-0003-3033-1516
1 Biology Department, College of Sciences, Basrah University, Iraq; [email protected]. ORCID 0000-0002-6793-5893
2 Biology Department, College of Sciences, Basrah University, Iraq; http://[email protected] Orcid 0000-0002-6315-4360
3 Al Zahraa College of Medicine, Basrah University, Iraq; [email protected]. ORCID 0000-0002-2625-8013
4 Basrah Nuclear Medicine Center. Iraq; [email protected]
5 College of Medicine University of Basrah. Iraq; [email protected]; ORCID 0000-0002-5138-8055
Available from: http://dx.doi.org/10.21931/RB/2023.08.03.86
ABSTRACT
Thyroid nodules are commonly prevalent in human populations and have global concerns due to the high raped increase during the last decades. Some of them have malignant potential and cause life-threatening. The prospective cross-sectional study was conducted on 104 persons with thyroid nodules (25 with thyroid cancer and 79 samples were benign lesions) in Basrah, Iraq, from November 2019 to April 2022. To investigate the association of insulin resistance, Glucose, insulin hormone and obesity on thyroid cancer, Results: the thyroid cancer samples have higher serum levels of metabolic parameters, insulin hormone, Glucose, and insulin resistance (HOMA-IR) than benign samples, the male samples have a significant difference in HOMA-IR than females in all samples (malignant and benign samples), No substantial difference has been observed in BMI between thyroid cancer and harmless subjects; Conclusions: the serum metabolic parameters, insulin hormone, Glucose, and HOMA-IR play a vital role in future as an indicator for the diagnosis of thyroid cancer (papillary carcinoma) due to their increased levels in thyroid cancer samples than benign samples, no clear association between obesity and thyroid cancer incidence.
Keywords: Metabolic parameters; Insulin resistance; Glucose; Insulin hormone; Thyroid cancer; Homa -IR
INTRODUCTION
Cancer is a significant global health concern that affects public health on a large scale 1. The uncontrolled division of cells and their invasive potential into nearby or remote tissues are defining features of a group of diseases known as Cancer (metastasis) 2,3. Also, Cancer is considered an abnormal growth of cells caused by multiple changes in gene expression, leading to a dysregulated balance of cell proliferation and cell death and ultimately evolving into a population of cells that can invade tissues and metastasize to distant sites, causing significant morbidity and, if untreated, end of the host 4. Thyroid cancer is becoming the most dominant Cancer in the endocrine system. It is prevalence has increased during the last three decades over the world 5–7, consisting of about 2.3% of all new cancer cases in the US 7. It accounts for ≤1% of all human malignancies, and the thyroid nodules are the majority of lesions that can be found in 19%-68% of randomly selected people have nodules in there thyroid gland, most of them benign nodules 8 7% of them may have a suspicious nodule for thyroid cancer depending on age, gender, radiation exposure, family history and other factors 5,9, in Iraqis population the thyroid nodules are ordinary. However, thyroid cancer is 1.7% of these nodules (10), while Mansour et al. (2020) 11 found that the prevalence of thyroid cancer was 0.4% (n=77) from 17878 patients presented with thyroid lesions in the Iraqi population/ Basrah province.
Despite thyroid cancer being the most common type of endocrine Cancer 12, it is a relatively rare disease and is responsible just for ≤1% of all human Cancer and responsible for six deaths per million persons annually 8; many studies documented that the overall Incidence of thyroid carcinoma has increased more rapidly than that of any other malignancy in recent years, especially in women 13 dysregulated cellular growth is a feature of the cancer disease to provide more energy, to sustain the cellular proliferation, growth, made new vessels (angiogenesis). Strong evidence proved that dysregulated metabolism has an essential role in cells to promote oncogenesis 14 due to the thyroid gland having a significant role in all body metabolism, so any lesion of the thyroid gland will affect the metabolism, particularly glycemic 15. Previous studies have failed to demonstrate the effect of dysregulated metabolism during thyroid cancer and have only focused on studying the pathological impact of metabolism syndromes like diabetes, hypertension, and obesity. This paper introduces a novel approach to investigating the role of metabolic syndrome during thyroid cancer disease, which has not been previously explored in the literature and needs more cross-sectional studies.
In this paper, we investigate the effect of some metabolic parameters like Glucose, Insulin hormone and Insulin resistance on thyroid cancer.
MATERIALS AND METHODS
Study Design and Subjects. A clinical cross-sectional study was used to investigate the effect of Insulin resistance, Glucose and Insulin hormone on thyroid cancer; The study population consisted of 36 patients (25 serum samples and 36 tissues) with thyroid cancer (11 men, 25 women) and 79 samples (79 serum and 23 tissues) with benign thyroid lesions (7 men, 72 women) since the mean age of thyroid cancer samples was 36.166±16.84 years. The mean age of harmless subjects was 40.016±10.519 years (Figure 2-1). All subjects undergoing health checkups in Iraq/Basra province hospitals and medical centers from November 2019 to April 2022. All blood samples were collected at the first assessment of thyroid nodules (Ultrasound examination and Fine Needle Aspiration procedure). Our representatives in this study have a thyroid nodule different from the normal parenchyma of the normal thyroid gland on ultrasound examination. The collected data included gender, age, weight and height, thyroid function (T3, T4 and TSH) in addition to collected fasting blood serum samples for more tests, insulin hormone (by using Elabsceince ELIZA hormones kits, cat. No. E-EL-H2665) and fasting Glucose (Glucose kit by Biotech diagnostic company, UK). The BMI was determined according to 16, Insulin resistance 17. The data underwent statistical analysis and was processed using the statistical software IMP-SPSS-version 26 computer facilities. All data were presented in simple mean and standard deviation measures. ANOVA was applied to test the significance of difference among different means, correlation (person) was used to study the relationship between parameters, and a P value equal to or less than the 0.05 significance level was considered statistically significant.
.
RESULTS
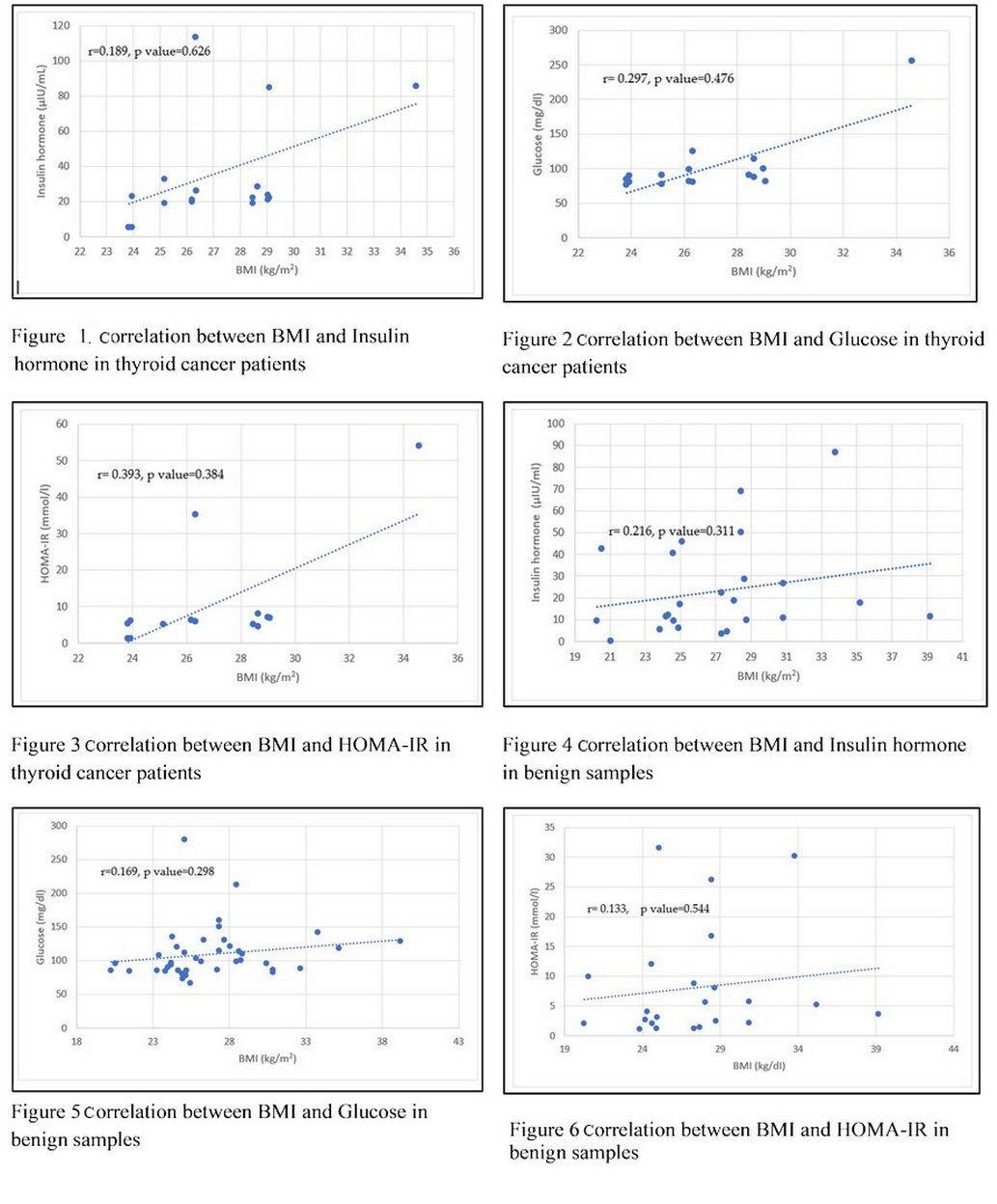
The biological and biochemical parameters of the present study show there is no significant difference between Cancer and benign group samples according to gender in BMI (kg/m2) and age (years) parameters; the mean of BMI (kg/m2) was 2.27±0.64, 1.88±0.526 (kg/m2) (males, females respectively) in thyroid cancer patients, and 1.79±0.53 kg/m2, 1.91±0.55kg/m2 (males, females respectively) in benign thyroid disorder. While the mean age (years) in thyroid cancer was 47.55±11.75years, 38.88±13.15 years (males, females respectively) and 40.58±12.17 years, 41.07±11.87 years (males, females respectively), as well, no significance was detected between two groups (Cancer and benign groups) for thyroid function T3, T4 and TSH hormones, The concentration of Insulin hormone, Glucose, Insulin resistance and Quicki insulin resistance that were investigated by mean of (HOMA-IR) and Insulin sensitivity index (Quicki insulin resistance) using blood samples obtained from malignant thyroid cancer and benign (thyroid disorder) revealed that all parameters were higher in cancer patients in comparison with harmless subjects, except Quicki index was higher in mild than cancer samples. Since the value in cancer patients' Insulin hormone was 99.63±19.765 μIu/ml in males,28.04±10.48 μIu/ml in females, Glucose was was190.00±91.92mg/dI in males, 123.80±6.172 mg/dI in female and HOMA-IR 44.50±13.342 mmol/l in males, 12.488±6.797 mmol/l in females. In contrast, the value in benign subjects' insulin hormone was 28.23±10.879 μIu/ml in males, 24.88±11.612 μIu/ml in females, Glucose was 149.00±88.662mg/dL in males, 122.38±48 mg/dI in females and HOMA-IR was 13.502±9.94 mmol/l in males, 8.417±3.614 mmol/l in females. Moreover, statistically, there was a significant difference (p≤0.05) between the cancer patients and benign subjects table (1). According to the comparison between males and females, the malignant groups showed there were significant differences (p≤0.05) between the males and females in Insulin hormone (98.638±19.76 μIu/ml and 28.04±10.48 μIu/ml, respectively, males and females) table (2). However, the benign samples table showed no significant difference between genders (3). when investigating the influence of gender according to age group on metabolic parameters, the age group was divided into two categories, the less than 50 years group and the more than group, as shown in table (4); in thyroid samples, the mean of metabolic parameters, Insulin resistance (μIu/ml), glucose (mg/dl) and HOMA-IR (mmol/l) were a lowest in age group less than 50 years (70.74±16.193 μIu/ml, 103.67±41.861 mg/dl and 6.967±9.75 mmol/l) respectively than age group more than 50 years, in males group the results show there was the significant difference at p<0.05 to thyroid cancer group on benign subjects in Insulin hormone (in both age groups), Glucose (in age group more than50 years) and HOMA-IR (in both age groups). In contrast, there was no significant difference between age groups in female samples in all metabolic parameters (Table 5). The results of thyroid cancer samples correlation reveal that BMI correlated positively but non-significant with Insulin hormone (r=0.189, p value= 0.626), glucose (r=0.297, p value=0.476) and HOMA-IR (r=0.393, p value=0.384) figures (1,2 and 3), in benign samples the BMI has positively correlated with Insulin hormone (r=0.216, p value= 0.311), Glucose (r= 0.169, p value= 0.298) and HOMA-IR (0.133, p value=0.544) (Figures 4-6).
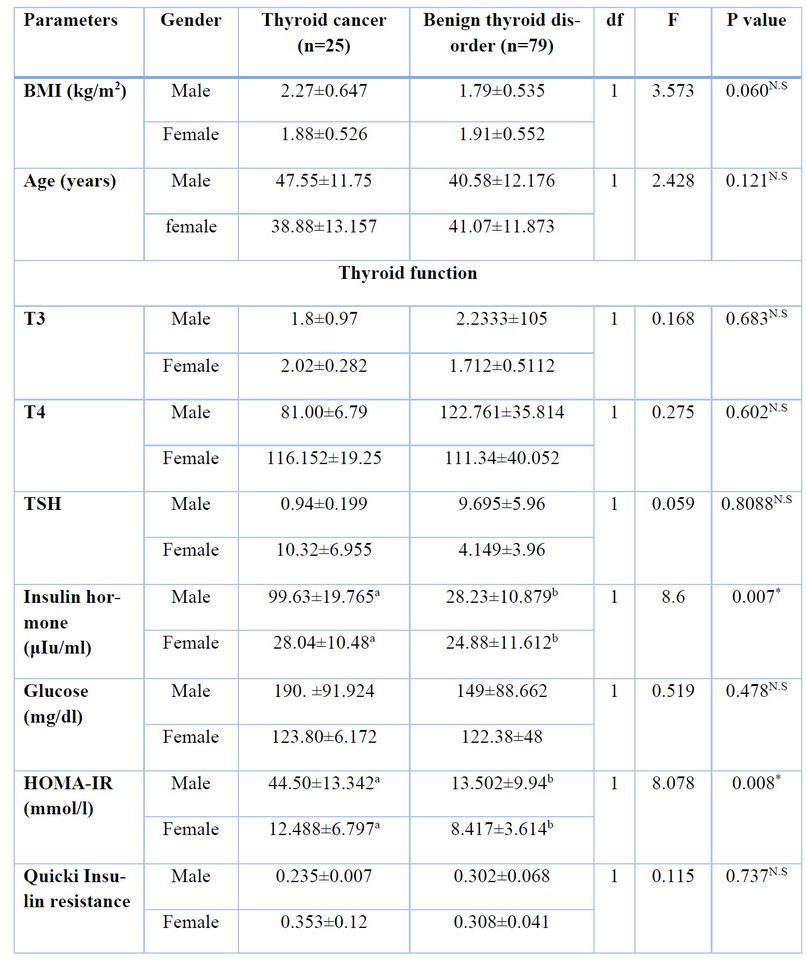
Table 1. Biological and biochemical parameters of all study samples (thyroid cancer and benign group)
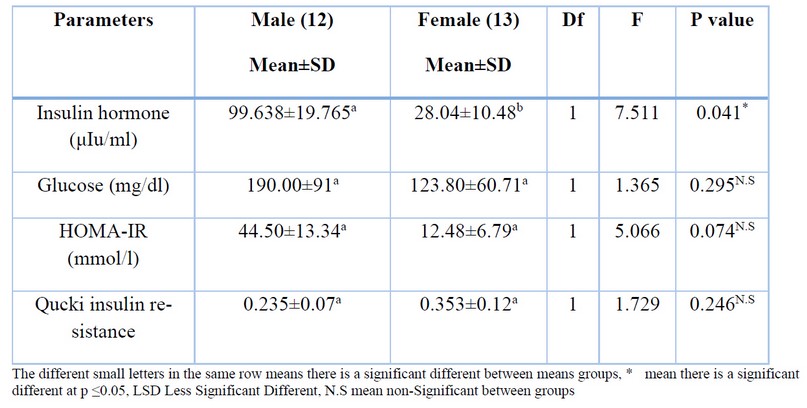
Table 2. Relationship between some of the metabolic parameters according to both genders (Male and Female) in thyroid cancer patients
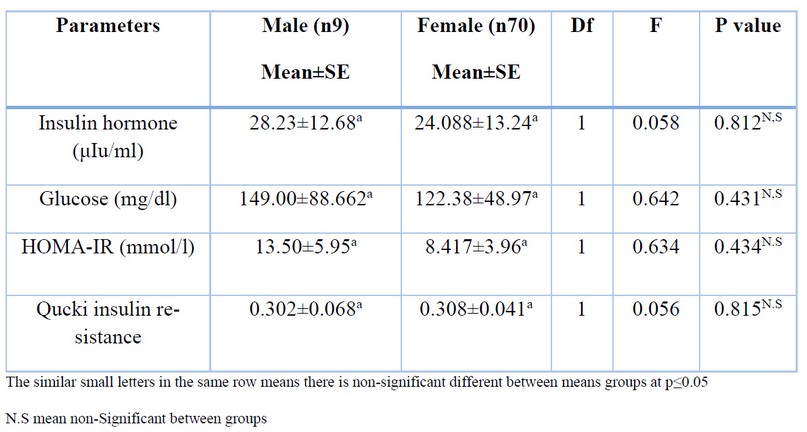
Table 3. Relationship between some of the metabolic parameters according to both genders (Male and Female) in the control group
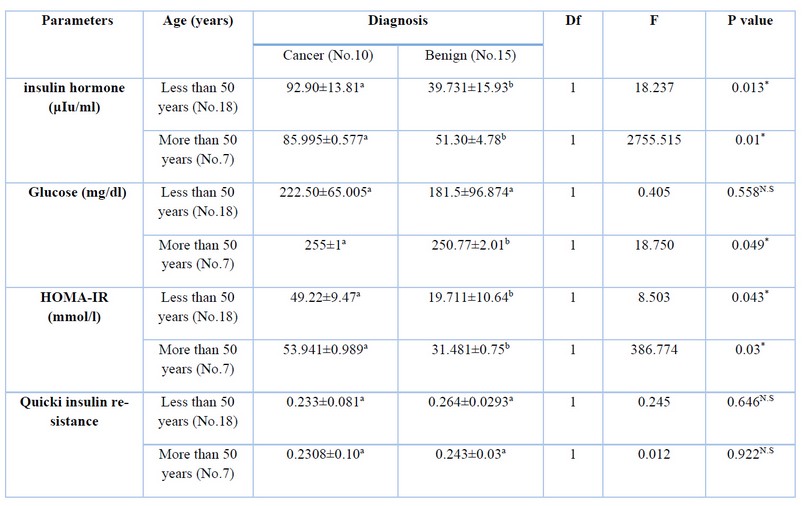
Table 4. The levels of metabolic parameters according to age group in male samples
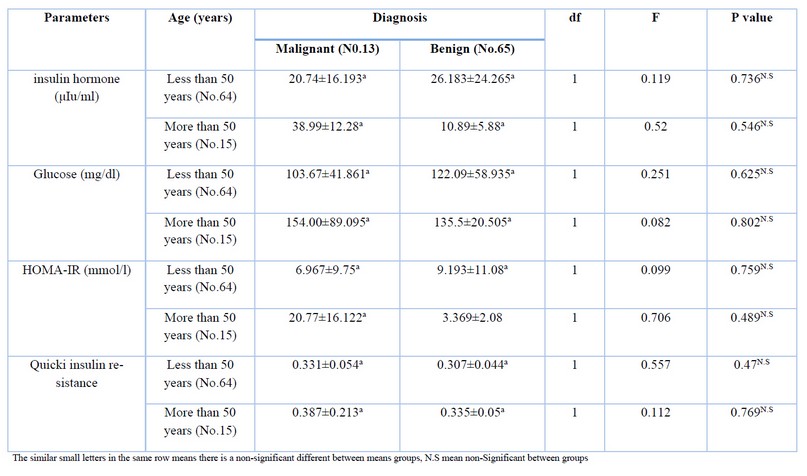
Table 5. the levels of metabolic parameters according to age group in females' sample
DISCUSSION
Abnormal cellular metabolism has been considered one of the hallmarks of malignant, which plays a vital role in oncogenesis 14. Because cancer cells need high bioenergetic requirements to activate and maintain cell growth. The malignant cells preferred glycolysis to generate lactate compared to the more energy-efficient oxidative phosphorylation pathway, which produces more ATP per molecule of Glucose than glycolysis 18,19. Choi et al. (2021) 20 indicated that insulin resistance (Homa-IR index) could be helpful as an indicator for patients with a thyroid disorder. Furthermore, a positive correlation has been found between insulin resistance and hypothyroidism, especially in women.
The current study revealed a significant difference in Homa-IR between thyroid cancer patients and benign subjects; these findings agree with 21,22. The results of the present study confirm that insulin resistance (Homa-IR) is a risk factor for thyroid cancer.
Mittal et al. (2012) and Şahin et al. (2013) 23,24 also found a significant association between insulin resistance and papillary thyroid cancer.
Li et al. (2019) 25 concluded that the thyroid nodules were higher in patients with metabolic syndrome than without metabolic syndrome due to the role of hyperglycemia in developing the thyroid nodules. Also, Arcidiacono et al.(2012) 26 demonstrated that Insulin resistance has an essential role in malignant cells' proliferation and progression by an increase in circulating Insulin hormone, which leads to overproduction of reactive oxygen species (ROS) that can damage DNA, contributing to mutagenesis and carcinogenesis. By his role in mitochondrial exhaustion, these initiating events lead to mitochondrial dysfunction and increased ROS 27. Zhao et al. (2021) 28 found that Abnormal glucose metabolism, high levels of Insulin hormone, and insulin resistance were significantly associated with the Incidence of thyroid cancer.
In the current study, the insulin hormone and Glucose levels were higher in thyroid cancer than in benign subjects. However, a previous study has reported that the fasting serum insulin level is higher in thyroid carcinoma patients than in controls 29. other studies did not show the same result 30–32, but they refer that the insulin hormone was not prevalent in patients with thyroid cancer. Some other pathologic mechanisms may be more prominent during thyroid carcinogenesis.
It has been demonstrated that in the present study, insulin resistance was higher in men than women, and this is in agreement with Geer and Shen (2010) 33, who demonstrated that the elevated visceral and hepatic adipose tissue in men, in conjunction with the lack of a possible protective effect of estrogen and lower adiponectin levels, may contribute to their higher insulin resistance in men compared with women.
The results of our study showed that the metabolic parameters in all samples have a positive correlation with BMI index, which agrees with Timóteo et al. (2014) 34, which concluded that Insulin resistance HOMA-IR was directly correlated with BMI and can be an Indicator for metabolic syndrome.
CONCLUSIONS
The levels of serum insulin hormone, Glucose, Homa-IR, and quick were higher in thyroid cancer than in benign subjects. The females of the thyroid cancer group have a lower level of insulin hormone, Glucose, and insulin resistance than the males group.
The present study indicated that the serum metabolic parameters, insulin hormone, Glucose and HOMA-IR may play a vital role in the future as indicators for diagnosis of thyroid cancer (papillary carcinoma) due to their increased levels in thyroid cancer samples than benign samples; no clear association has been detected between obesity and thyroid cancer incidence.
Supplementary Materials: All supplementing data for this manuscript are viable with the corresponding author.
Author Contributions: All authors were contribute to accomplished and write this article
Funding: This research received no external funding
Informed Consent Statement: Informed consent was obtained from all subjects involved in the study
Data Availability Statement: all data of this study can be found with corresponding author
Conflicts of Interest: The authors declare no conflict of interest.
REFERENCES
1. 1. Akker, M. et al. (2014) 'Investigation of insulin resistance gene polymorphisms in patients with differentiated thyroid cancer', Molecular Biology Reports, 41(5), pp. 3541–3547. doi: 10.1007/s11033-014-3218-2.
2. Al-Rikaby, H. and Al-Subaiee, I. N. (2019) 'Prevalence of thyroid incidentaloma detected by high-resolution ultrasound and their potential risk of malignancy in healthy individuals in Basrah Province', Medical Journal of Babylon, 16(3), p. 252. doi: 10.4103/mjbl.mjbl_31_19.
3. American Cancer Society (2021) 'American Cancer Society. Cancer Facts & Figures 2021. Atlanta: American Cancer Society; 2021'. Available at: https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2021.html.
4. Arcidiacono, B. et al. (2012) 'Insulin resistance and cancer risk: An overview of the pathogenetic mechanisms', Experimental Diabetes Research, 2012. doi: 10.1155/2012/789174.
5. Balkan, F. et al. (2014) 'Is there any association between insulin resistance and thyroid cancer?: A case control study’, Endocrine, 45(1), pp. 55–60. doi: 10.1007/s12020-013-9942-x.
6. Bernet, V. J. and Chindris, A. M. (2021) 'Update on the Evaluation of Thyroid Nodules', Journal of nuclear medicine : official publication, Society of Nuclear Medicine, 62, pp. 13S-19S. doi: 10.2967/jnumed.120.246025.
7. Chambers, A. F., Groom, A. C. and Macdonald, I. C. (2002) 'DISSEMINATION AND GROWTH OF CANCER CELLS IN METASTATIC SITES', 2(August). doi: 10.1038/nrc865.
8. Choi, Y. M. et al. (2021) 'Association between thyroid hormones and insulin resistance indices based on the Korean National Health and Nutrition Examination Survey', Scientific Reports, (0123456789), pp. 1–7. doi: 10.1038/s41598-021-01101-z.
9. Curry, J. M. et al. (2013) 'Cancer metabolism, stemness and tumor recurrence : MCT1 and MCT4 are functional biomarkers of metabolic symbiosis in head and neck cancer', Cell Cycle, 12(9), pp. 1371–1384. doi: 10.4161/cc.24092.
10. Fallahi, P. et al. (2015) 'New Therapies for Dedifferentiated Papillary Thyroid Cancer', pp. 6153–6182. doi: 10.3390/ijms16036153.
11. Geer, E. B. and Shen, W. (2010) 'Gender Differences in Insulin Resistance, Body Composition, and Energy Balance', Gend Med. NIH, 6(1), pp. 60–75. doi: 10.1016/j.genm.2009.02.002.Gender.
12. Giusti, M. et al. (2008) 'Metabolic and cardiovascular risk in patients with a history of differentiated thyroid carcinoma: A case-controlled cohort study', Thyroid Research, 1(1), p. 2. doi: 10.1186/1756-6614-1-2.
13. Guth, S. et al. (2009) 'Very high prevalence of thyroid nodules detected by high frequency (13 MHz) ultrasound examination', European Journal of Clinical Investigation, 39(8), pp. 699–706. doi: 10.1111/j.1365-2362.2009.02162.x.
14. Haugen, B. R. et al. (2016) 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer, Thyroid, 26(1), pp. 1–133. doi: 10.1089/thy.2015.0020.
15. Heidari, Z., Abdani, M. and Mansournia, M. A. (2018) 'Insulin resistance associated with differentiated thyroid carcinoma: Penalized conditional logistic regression analysis of a matched case-control study data,' International Journal of Endocrinology and Metabolism, 16(1), pp. 1–7. doi: 10.5812/ijem.14545.
16. Vander Heiden, M. G., Cantley, L. C. and Thompson, C. B. (2009) 'Understanding the Warburg Effect: The Metabolic Requirements of Cell Proliferation,' Encyclopedia of Neuroscience, 324(5930), p. 12. doi: 10.1007/978-3-540-29678-2_5605.
17. Hirschey, M. D. et al. (2015) 'Dysregulated metabolism contributes to oncogenesis,' Seminars in Cancer Biology, 35, pp. S129–S150. doi: 10.1016/j.semcancer.2015.10.002.
18. Holloszy, J. O. (2013) '"Deficiency" of mitochondria in muscle does not cause insulin resistance,' Diabetes, 62(4), pp. 1036–1040. doi: 10.2337/db12-1107.
19. Jemal, A. et al. (2019) 'Cancer Statistics, 2019', CA: A Cancer Journal for Clinicians, 57(1), pp. 43–66. doi: 10.3322/canjclin.57.1.43.
20. Li, Z. et al. (2019) 'A Mechanism Exploration of Metabolic Syndrome Causing Nodular Thyroid Disease,' Hindawi International Journal of Endocrinology, pp. 1–7. doi: 10.1155/2019/9376768.
21. Liu, H. and Lin, F. (2015) 'Application of immunohistochemistry in thyroid pathology,' Archives of Pathology and Laboratory Medicine, 139(1), pp. 67–82. doi: 10.5858/arpa.2014-0056-RA.
22. Mansour, A. A. (2011) 'The association of diabetes and hyperthyroidism in Basrah', New Iraqi Journal of Medicine, 7(1), pp. 30–34.
23. Mansour, A. A. et al. (2020) 'Patterns of thyroid disease in Basrah, Iraq. Retrospective study, Jour. Endocrine Society, 4(1), pp. 276–277. doi: 10.1210/jendso/bvaa046.
24. Mittal, A. et al. (2012) 'Metabolic changes enhance the cardiovascular risk with differentiated thyroid carcinoma - A case-control study from Manipal Teaching Hospital of Nepal,' Asian Pacific Journal of Cancer Prevention, 13(5), pp. 2335–2338. doi: 10.7314/APJCP.2012.13.5.2335.
25. NIH, National Hert, L. and B. I. (2022) 'Calculate the Body Mass Index.' Available at: https://www.nhlbi.nih.gov/health/educational/lose_wt/BMI/bmicalc.htm.
26. Rego-Iraeta, A. et al. (2009) 'Time Trends for Thyroid Cancer in Northwestern Spain: True Rise in the Incidence of Micro and Larger Forms of Papillary Thyroid Carcinoma', pp. 333–340.
27. Rezzónico, J. N. et al. (2009) 'Increased Prevalence of Insulin Resistance in Patients With Differentiated Thyroid Carcinoma,' Metabolic Syndrome and Related Disorders, 7(4), pp. 375–380. doi: 10.1089/met.2008.0062.
28. Ruddon, R. W. (2007) Cancer Biology. FOURTH. Oxford University Press.
29. Şahin, M. et al. (2013) 'Vitamin D3 levels and insulin resistance in papillary thyroid cancer patients', Medical Oncology, (30), pp. 1–10.
30. Salgado, A. L. F. D. A. et al. (2010) 'Insulin resistance index (HOMA-IR) in the differentiation of patients with non-alcoholic fatty liver disease and healthy individuals,' Arquivos de Gastroenterologia, 47(2), pp. 165–169. doi: 10.1590/S0004-28032010000200009.
31. Seyfried, T. N. and Huysentruyt, L. C. (2013) 'On the Origin of Cancer Metastasis,' Crit Rev Oncog, 18(2), pp. 43–73. doi: 10.1615/critrevoncog.v18.i1-2.40.
32. Timóteo, A. T. et al. (2014) 'Optimal cut-off value for homeostasis model assessment (HOMA) index of insulin-resistance in a population of patients admitted electively in a portuguese cardiology ward', Acta Medica Portuguesa, 27(4), pp. 473–479. doi: 10.20344/amp.5180.
33. Zhao, J. et al. (2021) 'High prevalence of thyroid carcinoma in patients with insulin resistance: a meta-analysis of case-control studies', Aging, 13(18), pp. 22232–22241. doi: 10.18632/aging.203529.
34. Zhao, J. et al. (2022) 'Abnormal Glucose Metabolism Parameters and the Aggressiveness of Differentiated Thyroid Carcinoma: A Hospital-Based Cross-Section Study in China', Frontiers in Endocrinology, 13(March), pp. 1–9. doi: 10.3389/fendo.2022.806349.
Received: 25 June 2023/ Accepted: 26 August 2023 / Published:15 September 2023
Citation: Reda Hussein A; Jameel Thamer S; Kasim Suker D; Hameed Abbood M; Al-Tuma R R; Al-Mansouri L. Insulin resistance profile as an indicator for Incidence of thyroid cancer. Revis Bionatura 2023;8 (3) 86. http://dx.doi.org/10.21931/RB/2023.08.03.86
