2022.07.02.37
Files > Volume 7 > Vol 7 No 2 2022
1Department of Rheumatology and Rehabilitation, Ramadi Teaching Hospital, Anbar, Iraq
2* Department of Medicine, College of Medicine, University of Anbar, Anbar, Iraq
3 Department of Medicine, Ramadi Teaching Hospital, Anbar, Iraq
Available from: http://dx.doi.org/10.21931/RB/2022.07.02.37
ABSTRACT
Systemic lupus erythematosus (SLE) is a polygenic chronic inflammatory condition that influences several body organs. While renal and dermatological changes are among the most common presentations of the disease. The current study examines the possible association between human Resistin (h-Res) and signs of disorder activities such as inflammation, renal function, lipids, and Bone Mineral Density (BMD) in females with SLE.
We performed cross-sectional research on 50 females with SLE diagnosed using the American College of Rheumatology (ACR) criteria. Forty females were recruited as controls. They matched the following items, including gender and body mass index (BMI) with age. In SLE patients, we discovered a statistically significant positive relationship between h-Res levels and ESR, CRP, Cr, ds-DNA, C3, duration of steroid treatment, and other variables. Disorder activity as determined by systemic lupus erythematosus disease index (SLEDAI) and carotid intima-media thickness (CIMT) (p-value <0.05). The levels of h-Res and C3 are discovered to have a statistically significant negative relationship. In the case of SLE, the h-Res level can be used as a marker for Lupus Nephritis (LN) and atherosclerosis. In patients of SLE, more aggressive therapy of the underlying inflammatory process and better control of the traditional risk factors may be beneficial in reducing the risk of renal and atherosclerotic derangement.
Keywords. biomarker, lupus nephritis, systemic lupus erythematous, Atherosclerosis
INTRODUCTION
SLE is a chronic inflammatory illness that mainly affects women and for which there is now no recognized solution. Lupus nephritis (LN) is a severe symptom of SLE that damages the kidneys and is associated with renal failure, Patients with SLE, which affects 50% of the population and causes significant morbidity and mortality, are at an elevated risk of having a premature atherosclerotic cardiovascular disease (ASCVD) 1. Many hormones and cytokines with significant systemic metabolic effects have been discovered in adipose tissue, which has been investigated for its capacity to release them. It is commonly acknowledged that adipocytes and a variety of other cells found in adipose tissue, such as immunocompetent cells, contribute to the total endocrine production of the body 2. Resistin is a cysteine-rich secretory peptide that has just been found, and It is thought that adipocyte is the source of its synthesis. According to animal research, h-Res is produced mainly in white adipose tissue and might represent the link between obesity and insulin resistance (IR). In humans, the function of h-Res is not yet totally elucidated. There is a hypothesis that h-Res has a pro-inflammatory impact and is plentiful in inflammatory illnesses (for example, Crohn's disease and rheumatoid arthritis (RA), and similarly, it is produced together with other inflammatory markers in many individuals 3.h-Res seems to have some role in bone metabolism, perhaps by stimulation of osteoblast and osteoclast activity, this is mediated by the nuclear factor-kappa B either directly or indirectly (NF-B) pathway. SLE is a chronic inflammatory illness that affects the kidneys and other organs throughout the body. It is characterized by a state of chronic inflammation throughout the body 4. As a result, we wanted to determine if there was a relationship between h-Res and numerous indicators of disease activity, lipids, renal function, inflammation, and bone mineral density (BMD) in females with SLE.
MATERIALS AND METHODS
In this study, 50 females with SLE illness participated in a cross-sectional design. SLE was diagnosed using the American College of Rheumatology's criteria (ACR). A total of forty matched controls were included in the investigation. Because h-Res is associated with obesity, the controls and the experimental group had similar BMIs. All attendees received educational booklets as a part of the program. All participants, including the control individuals, provided written informed permission before participating in the study. The medical ethics committee at Ain Shams University approved the study.
Exclusion criteria
The following problems have been identified: gestational diabetes, malignancy, SLE linked with other diagnoses (overlap conditions), liver diseases, intestinal inflammation, and instances with a history of angina, stroke, myocardial infarction, and renal failure on hemodialysis.
Inclusion Criteria
The other patients, however, while the study included cases of subclinical atherosclerosis (dyslipidemia) and patients with concomitant hypertension, this was done because some of the conventional hazards for atherosclerosis can be caused or worsened by SLE and/or interventions (steroid intake), hypertension alone with no dyslipidemia may be secondary to renal dysfunction rather than SLE.
Clinical evaluation
History and physical examinations were completed focusing on the duration of illness, history of medications intake, and conventional cardiovascular risk factors. The complete clinical study was done for all patients, and controls included calculating BMI (kg per m 2) and BP measurement. Hypertension has been defined as follows: SBP ⩾140 mmHg or DBP ⩾90 mmHg.
Laboratory assessment
Venous blood specimens were taken after fasting overnight, and sera were kept at -70 C until analyzed. Standard laboratory procedures were used to assess CRP levels, blood cell count, erythrocyte sedimentation rate (ESR), C3, C4, Cr, and HDL, total cholesterol, triglycerides (Tg), and low-density lipoprotein both were investigated employing ordinary lab methods.
Bone biomarkers
The radioimmunoassay method was used to assess the quantitative levels of the bone reabsorption indicators Cross-linked carboxyterminal telopeptide of type I collagen (ICTP) and the bone formation markers Procollagen type 1 N-terminal Propeptide (P1NP) (Orion Diagnostical, Espoo, Finland). Threshold values for CTP were 0.7-μg/L and 2-μg/L for P1NP.
Human Resistin (h-Res)
h-Res levels have been determined with sandwiched enzyme-linked immunosorbent assays (ELISA) (R & D Systems, Inc., Minneapolis, MN, USA).
Cytokines
The pro-inflammatory cytokines such as TNF- α -, IL-1β, IL-6, and soluble IL-6 receptor (sIL-6R) were quantified using a quantitative sandwich ELISA kit with a diagnostic threshold of 0.12, 0.1, 0.7, and 6.5 pg/mL, respectively.
Bone mineral densities measures
This study used the non-dominant hip (femoral neck and entire hip), Lumbar spine (L2–L4), and According to the DEXA scan, the non-dominant distal forearm has been identified (Dual energies x-ray absorptiometry) with a Lunar Prodigy densitometer 12165 (GE Healthcare, Little Chalfont, UK).
Fractures
Using a visual semi-quantitative method, we detected prominent vertebral compression fractures in the thoracic and lumbar spines (Th4-L4) on lateral x-rays of these regions. Generally speaking, compression fractures are defined as any vertebral abnormality that results in a minimum of a 20-25 % drop in height at the frontal, middle, and/or back levels. The same radiologist reviewed all X-rays throughout the study.
Normal controls
The levels of h-Res were determined in ten healthy donors and thirty healthy female staff members and Ph.D. students in the Rheumatology department.
Statistical analysis
The statistical analysis was carried out using SPSS-12.0.1 (IBM Inc., USA). Descriptive parameters were provided as median and range or as mean and standard deviation (mean SD). The Kolmogorov-Smirnov test investigated the relationships between all of the variables. The Pearson correlation was used when the variables had a normal distribution; otherwise, the Spearman correlation was used. All tests were two-tailed, and the level of statistical significance was set at p<0.05.
RESULTS
According to the findings, the mean age of the patients under investigation was 25.26 yrs (±7.37 SD). The mean disorder (SLE) duration was 3.53 yrs (± 1.34 SD). The mean systolic blood pressure appeared to be 128.4 (± 15.5). Mean Diastolic blood pressure was 82.69 (±8.4 SD). The mean BMI was 28.09 (± 0.74 SD). Mean cholesterol was 225.01 (± 86.5 SD). Mean LDL was 149.05 (± 49.7 SD). Mean HDL was 40.5 (± 10.56 SD). Mean Triglycerides were 132.09 ± 57.25 SD) as in figure(1). There was a very significant difference in the levels of Cr, ESR, CRP, h-Res, or CIMT between the experimental and control groups, as in figure 2. Additionally, when comparing individuals with and those who do not have lupus nephritis, we found that those disparities were evident as well figure 3; in SLE cases, a significant positive association has been found between h-Res levels and CRP, ESR, Cr, ds-DNA, steroid use, disorder activities determined using CIMT and SLEDAI (p-value < 0.05). It was discovered that there was a significantly substantial negative relationship between h-Res levels and C3-figure 4.
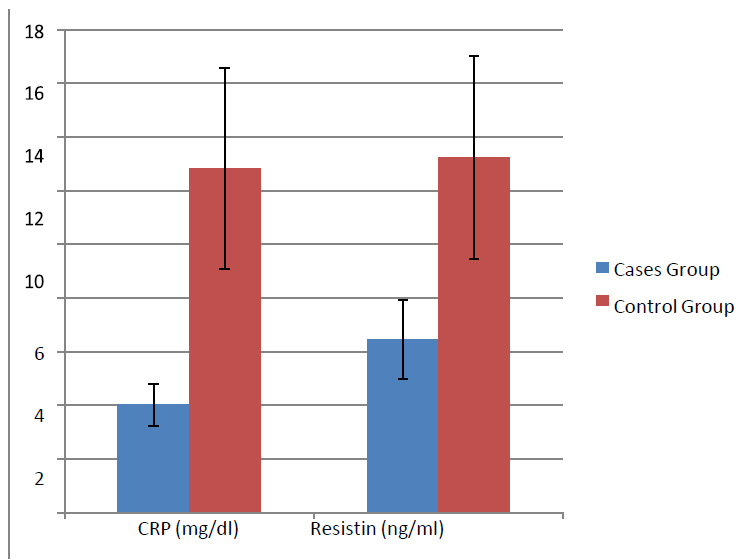
Figure 1. Comparing among the study groups regarding CRP and resistin
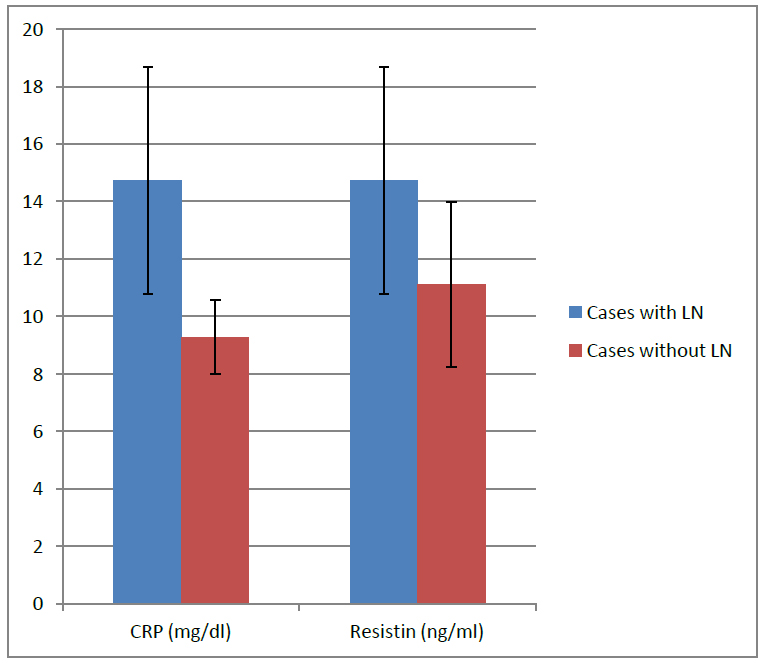
Figure 2. Comparing cases with LN and those without LN, regarding CRP with Resistin
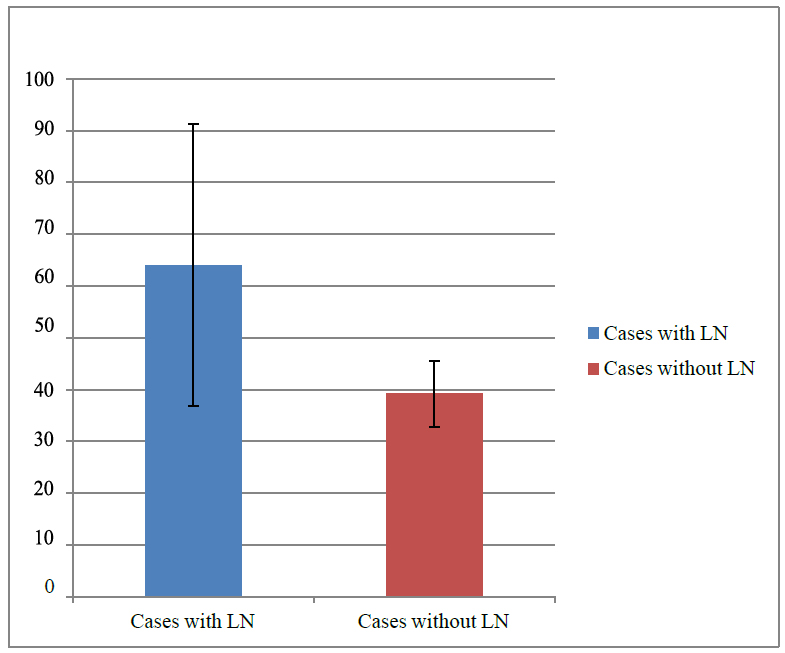
Figure 3. Comparing cases with LN and those without LN regarding ESR.
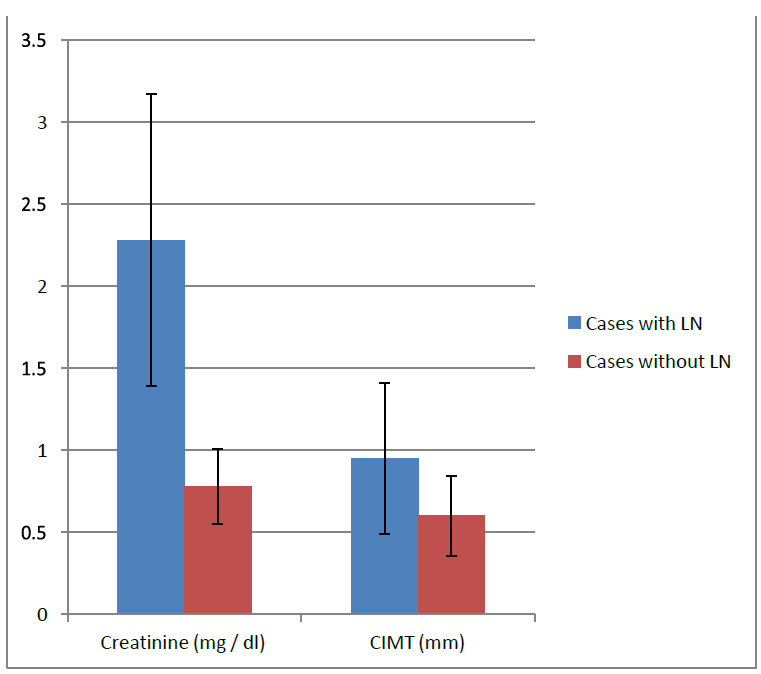
Figure 4. Comparing cases with LN and those without LN regarding creatinine and CIMT.
DISCUSSION
It has been shown that h-Res have pro-inflammatory and atherogenic properties related to the inflammatory response. It is widely believed to be connected with obesity and type 2 diabetes. Higher h-Res levels in the blood characterize obesity. Reduced glomerular filtration rates (GFR) and inflammation are related to high levels of h-Res in the blood. The researchers wanted to see whether h-Res might be used as a biomarker for nephritis and early atherosclerosis in SLE patients. Elshishtawy team enrolled 50 SLE females as well as 40 matching controls. All of the patients and participants in the control group were exposed to laboratory tests and carotid duplex exams. The SLE disorder Activity Index (SLEDAI) was developed to measure the severity of the disorder. A renal biopsy was conducted in individuals with SLE who also had LN. He reported elevated h-Res levels in SLE cases with LN compared to SLE cases with no nephritis, in concordance with other authors who revealed that renal dysfunctions in SLE were correlated with increased levels of h-Res. Elshishtawy team discovered a significant increase in cholesterol, LDL, triglycerides, and CIMT in individuals with SLE when compared to a control group of people with no SLE. This shows that females with SLE are at higher risk of developing early atherosclerosis and chronic vascular inflammation than men.
There was a statistically significant positive correlation between h-Res levels and CIMT, cholesterol, and triglyceride levels in the study participants 5. Almehed and his co-workers showed that 2.5% of his patients had reduced renal functions with GFR of <30-mL/min, and 14% had GFR of <50-mL/min using the projected GFR values 6. Over time, our findings showed a significant shift in Cr, ESR, CRP, h-Res, and CIMT. Even though the exact cause of elevated h-Res in SLE has not been determined, it is believed to be connected to changes in renal function, the direct effects of inflammatory mediators on h-Res production, changes in fat distribution, or a combination of these factors and others. Histamine's role in inflammation seems to be consistent with the relationship between h-Res levels, ESR, and CRP levels that have been identified before in studies7. Researchers have discovered that indicators of inflammation in SLE, including higher ESR, pro-inflammatory cytokines, immunoglobulin G (IgG), CRP, and low albumin, are related to high levels of h-Res in the blood 6. But, the Chung team observed a comparably modest association between h-Res and ESR but not with CRP; this might be due to the difference in sample size and the higher levels of disorder in our SLE patients. CRP persuaded both mRNA expressions and protein secretions of h-Res in a dose and period-reliant manner in peripheral blood mononuclear cells (PBMCs) 8. Our study demonstrated a highly significant change in SLE cases with LN and cases with non-LN in levels of Cr, ESR, CRP, h-Res or CIMT. But, Malyszko and his colleagues established a correlation between h-Res and renal functions 9, in concordance with a finding of Nu¨sken et al. in children on hemodialysis for chronic kidney disease (CKD) 10, and the limited number of patients with IgA renal dysfunction11.
H-Res was significantly correlated with GFR and inflammatory biomarkers in CKD. Because h-Res have a low molecular weight, The kidneys are thought to be the primary secretory channel. Chronic kidney disease (CKD) is a state of chronic inflammation characterized by a considerable increase in blood levels of pro-inflammatory cytokines at various stages of renal function impairment 12. Our findings revealed that among SLE patients, there is a statistically significant positive correlation between h-Res levels and ESR, CRP, Cr, dsDNA, steroid period, disorder activity as measured by the SLEDAI and CIMT, and a negative association between h-Res levels and ESR (p value< 0.05). A highly significant negative association was found between h-Res and C3. Our findings were also analogous to Baker 13, who found raised levels of h-Res in SLE patients with coronary artery calcifications. The early results of Kougias and co-workers 14, from their porcine vascular research revealed that h-Res might result in endothelial dysfunctions in the porcine coronary artery via oxidative stress and downregulation of endothelial nitric oxide (e-NO), consequently, has a direct effect on vascular disorders. The study done by Yaturu 15 revealed that levels of h-Res didn't correlate with GFR. This finding aligned with our findings though it contradicted the author's results, who found a significant negative association between h-Res and GFR 11. Still, their patients were not homogenous in the degree of CKD dysfunction. But some reports refer to a highly effective association between the level of resistance-to-insulin and TNF-a. Resistance-to-insulin was found to promote endothelially cell activations and was connected to cardiovascular disorders in metabolic disorders15. Inflammation of the vascular endothelial cells seems to result from insulin resistance, reduced by adiponectin 16 directly.
CONCLUSION
In SLE patients, the blood h-Res level may be used as a biomarker for LN and atherosclerosis, which can be measured. Controlling the underlying inflammatory process and traditional risk factors for both illnesses with more vigor may effectively lower the risk of renal and atherosclerosis dysfunction in rheumatoid arthritis and other autoimmune disorders.
Funding: Funded by self.
Acknowledgments: Thanks to all who support us.
Conflicts of Interest: The authors report no conflicts of interest.
REFERENCES
1. Parikh, S. V., Almaani, S., Brodsky, S., & Rovin, B. H. Update on lupus nephritis: core curriculum 2020. American Journal of Kidney Disorders. 2020; 76(2), 265-281.
2. Carrillo, J. L. M., Campo, J. O. M. D., Coronado, O. G., Gutiérrez, P. T. V., Cordero, J. F. C., & Juárez, J. V. Adipose tissue and inflammation. Adipose Tissue. 2018; 93.
3. Bakry, M., E Abd El-Hameed, N., El-Aziz, A., Reda, M., & MZ Hamada, M. Resistin; a physiological overview. Zagazig Veterinary Journal. 2021; 49(1), 78-91.
4. Acquarone, E., Monacelli, F., Borghi, R., Nencioni, A., & Odetti, P. Resistin: A reappraisal. Mechanisms of ageing and development. 2019; 178, 46-63.
5. Elshishtawy H, Ibrahim S, Helmi A, Farouk N, Elshinnawy A. hRes in systemic lupus erythematosus: Relation to lupus nephritis and premature atherosclerosis. The Egyptian Rheumatologist. 2012; 34(4), 137–146.
6. Almehed K, Forsblad-d'Elia H. Bokarewa M. Carlsten H. Role of hRes as a marker of inflammation in systemic lupus erythematosus. Arthritis research & therapy, 2008.
7. Poudel, B. The Role of Macrophages in the Development of Renal Injury Associated with Pre-Pubertal Obesity (Doctoral dissertation, The University of Mississippi Medical Center), 2021.
8. Chung CP, Long AG, Solus JF, Rho YH, Oeser A, Raggi P, et al. Adipocytokines in systemic lupus erythematosus: relationship to inflammation, insulin resistance and coronary atherosclerosis. Lupus 2009; 18(9):799–806.
9. Malyszko J, Malyszko JS, Pawlak K, Mysliwiec M. Resistin, a new adipokine, is related to inflammation and renal function in kidney allograft recipients. Transplant Proc 2006; 38:3434–6.
10. Nu¨sken KD, Kratzsch J, Wienholz V, Sto¨hr W, Rascher W, Do¨tsch J. Circulating hRes concentrations in children depend on renal function. Nephrol Dial Transplant 2006; 21:107–12
11. Kielstein JT, Becker B, Graf S, Brabant G, Haller H, Fliser D. Increased hRes blood levels are not associated with insulin resistance in cases with renal disorder. Am J Kidney Dis 2003; 42:62–6.
12. Podkowińska A., Formanowicz, D. Chronic kidney disorder as oxidative stress-and inflammatory-mediated cardio-vascular disorder. Antioxidants. 2020; 9(8), 752.
13. Baker JF, Morales M, Qatanani M, Cucchiara A, Nackos E, Lazar MA, et al. hRes levels in lupus and associations with disorder-specific measures, insulin resistance, and coronary calcification. J Rheumatol 2011; 38:2369–75.
14. Kougias P, Chai H, Lin PH, Lumsden AB, Yao Q, Chen C. Adipo-cyte-derived cytokine hRes causes endothelial dysfunction of porcine coronary arteries. J Vasc Surg 2005; 41(4):691–8.
15. Yaturu S, Daberry RP, Rains J, Jain S. hRes and adiponectin levels in subjects with coronary artery disorder and type 2diabetes. Cytokine 2006; 34:219–23.
16. Mourouzis, K., Oikonomou, E., Siasos, G., Tsalamadris, S., Vogiatzi, G., Antonopoulos, A., et al. Pro-inflammatory Cytokines in Acute Coronary Syndromes. Current pharmaceutical design. 2020; 26(36), 4624-4647.
Received: 1 December 2021 / Accepted: 9 March 2022 / Published:15 May 2022
Citation: Ismael khaleel S, Ghazzay H, Faeq Hammad A. Human Resistin as a Marker to Monitor Lupus Nephritis and Atherosclerotic Changes in Females with SLE. Revis Bionatura 2022;7(2) 37. http://dx.doi.org/10.21931/RB/2022.07.02.37
