2022.07.03.49
Files > Volume 7 > Vol 7 No 3 2022
Estimation of primer efficiency in multiplex PCR for detecting SARS-Cov-2 variants
Lubna Muhi Rasoul1, Mohanad M. Nsaif 2, Mohammed T.Al-Tameemi 3, Bahaa Abdullah Laftaah Al-Rubaii 4
1,4 Department of Biology, College of Science, University of Baghdad, Baghdad, Iraq
2 ministry of health, Baghdad, Iraq
3 Al-Qasim Green University\ Biotechnology College, Baghdad, Iraq
*Corresponding author: [email protected], mobile: 009647709780888
Available from: http://dx.doi.org/10.21931/RB/2022.07.03.49
ABSTRACT
In periodontology, polymerase chain reaction (PCR) has emerged as a standard diagnostic and research instrument. According to the findings in research, its sensitivity and specificity make it an efficient and speedy method for detecting, identifying, and quantifying organisms. The spike (S) gene, the envelope (E) gene, the membrane (M) protein, the nucleocapsids (N) gene, and the open reading frame (ORF) were used for the molecular identification of various variations of SARS-Cov-2 infection since they are critical components in the viral genome. Using kits approved by the Iraqi Ministry of Health following the spread of the covid-19 pandemic, this study sought to shed light on the significance of primers in the identification of various SARS-COV-2 variations involving many genes such as spike (S), envelope (E), membrane (M) protein, nucleocapsid (N), and ORFab1. A total of (150) clinically diagnosed patients for COVID-19 were screened for this study to estimate the accuracy and efficacy of primers used in detecting these genes are precise in diagnosing the infection in correspondence with clinical findings. The findings revealed that 18 (22.666%) of the cases had severe symptoms such as fever, unproductive hacking, breathlessness, muscle aches, and weariness, Whereas 42 (28%) of patients had lesser symptoms, and 74 (49.333%) of cases had minor signs on their own.. Results showed that all genes were accurate and efficient in the molecular diagnosis of the virus during the period from the beginning of March 2021 up to the writing of this manuscript in December 2021; the conclusion indicates that primers used in detecting these genes are efficient and accurate in the diagnosis of different variations of SARS-CAV-2 and there is no alteration in the viral genome in those genes that can disturb the result.
Keywords: SARS-Cov-2 variations, spike (S) gene, envelope (E) gene, membrane (M) protein, Nucleocapsids (N), multiplex PCR
INTRODUCTION
SARS-Cov-2 is a B-genus virus. Since approximately July 2021, four major variations of (SARS-CoV-2-) have been prevalent among many populations all over the world: the alpha () Variant, which was formerly known as the UK Variant and formally did refer to as B 1 1 7_, was initially discovered in England as well as Kent; the Beta Modified version, which was first found in England and Kent; and the Chikungunya Variant (formerly known as the South African Variant and formally referred to as .B.1.351.) The Gamma (ᴕ)Variant (previously known as the Brazil Variants and legally started referring to as . P. 1), and the Delta (Δ) Variant (previously known as the Indian Variant & officially referred to as . B . 1. 617 . 2 .) 1. A primer is a small collection of 18 to 24 DNA nucleotides that can be used in several additional investigations. A primer targets a particular locus in a polymerase chain reaction (PCR) to enable amplification and subsequent examination. This is done so that the locus in question can be studied further. In a sequencing reaction, a primer is first used to direct the reaction to a particular location, and then the length of the DNA molecule is determined 2. Multiplex PCR is a polymerase chain reaction technique used to amplify multiple DNA sequences simultaneously (as if performing several detach of PCR reactions in a single reaction). In a thermocycler, via numerous primers and a temperature-mediated DNA polymerase enzyme, this technique amplifies DNA in samples. All primer pairs must have their designs optimized so that during PCR, they can all work at the same annealing temperature. Primer sets are combined in one PCR mixture yielding amplicons of various sizes unique to multiple DNA sequences. Each primer set's annealing temperatures must be tuned for optimal performance within a single reaction 3. COVID has wrapped infections with the single-abandoned RNA-genome ( 26 _32 kb ) in the positive sense 4 . Human Covids (HCoVs) have been identified in the Covid (H-CoV-229E as well as NL63) and b-Covid (MERS-Co V, SARS-CoV, H-CoV-OC 43 and H-CoV-HKU1 ) genera 5. On the other side, the ORF region is responsible for nonstructural coding proteins. These proteins include 3-RNA-dependent RNA polymerase, chymotrypsin-like protease, and papain-like protease. The S, E, and M regions, as well as the Open Reading Frame 1ab area, code for structural proteins; the ORF region, meanwhile, codes for structural proteins 6. The SARS spike CoV-2 (S) protein comprises its two primary components, the S 1 protein and the S 2 protein. The SARS virus causes an increase in the production of the CoV-2 (S) protein, which is necessary for the fusion of cell membranes and the recognition of receptors on target cells. The receptor-binding area of the S1 subunit recognizes and binds to the host receptor angiotensin converting enzyme2. The two-heptad repeat domain of the S2 subunit contributes to the fusion of viral cell membranes by generating a six-helical bundle. Both of these functions are carried out by the S2 subunit. These two domains can be found on the S1 subunit of the protein7.
S-proteins play a vital role in the virus replication cycle and may be utilized as targeted therapies 8. Even though the S protein of SARS-CoV-2 is involved in receptor recognition, viral attachment, and host cell penetration, this protein is, for the most part, the same in all human coronaviruses (H-CoVs). Because of its vital roles, it is one of the most important targets for research involving the COVID-19 vaccine and potential treatments. Usually, the S protein will be in a metastable prefusion conformation. However, when the virus comes into contact with the host cell, the S protein goes through a significant amount of structural remodeling, which enables the virus to fuse with the membrane of the host cell; The spikes are covered in polysaccharide molecules so that they will not be recognized by the human immune system when they enter the body 9. The CoV-2 envelope (E) protein is a tiny, integral protein membrane involved in many stages of the viral life span, including assembling, budding, envelopes creation, and pathogenicity. However, it is also the most mysterious. It interacts with other Co-V proteins and host cell proteins and its activities as an ion-channeling viroporin 10. E-is extensively expressed inside the infected cell during the replication cycle, but just a tiny percentage of it is integrated into the virion-envelope 11. The preponderance of the protein is localized in intracellular trafficking sites such as the Endoplasmic Reticulum, Golgi apparatus, & ERGIC, in which it is involved in Co-V (assembly and budding) 12. Recombinant Co-Vs lacking E have much lower viral titers and are unable to mature, or generate propagation-incompetent progeny, highlighting the relevance of E in the development and maturation of viruses 13. The most common structural protein in coronaviruses is the M-glycoprotein, which spans the membrane bilayer and has a short NH2-terminal region outside the virus and a lengthy COOH terminal (cytoplasmic domain) within the virus14. The M-protein can make bonds with any of the other structural proteins. The internal virion's N protein-RNA complex can be kept stable 15. Viral attaching and entry into the host cell may be affected by mutations in the M-protein, which works with the S protein 16. The virus's S protein has become glycosylated, which may help it avoid detection by the immune system 17,18.
Nevertheless, the glycosylation of the S protein is unknown. The M protein's function is similarly not well understood. The viral genome of SARS-CoV-2 is enclosed in nucleocapsids, a helical protein essential structural element covered via the viral membrane. Since infected cells produced significant amounts of the SARS-CoV-2nucleocapsid protein, which improves the effectiveness of viral-RNA transcription and replication, it is reliable in virus identification using PCR19.
MATERIALS AND METHODS
Patients
Hospitalized COVID-19-infected patients participated in multicenter trial research in Baghdad, and the municipal Ethics Committees approved (University of Baghdad- College of science- dept. Of Biology Bioethics Committee Ref. no. CSEC/0221/0095. The study included (150) COVID 19 patients admitted at the public health laboratory who were diagnosed by RT-PCR with Fever, lethargy, dry coughing, nasal congestion, muscle aches, rhinorrhea, and difficulty breathing are the most common symptoms, with diarrhea occurring in a minority of cases.
Specimen
Oropharyngeal swabs and nasopharyngeal swabs samples were collected in sterile tubes. Contamination should be avoided during the samples' collection, storage, and transportation.
Kit description
Using a technology called multiplex PCR with a fluorescent probe, it is possible to identify SARS-Cov-2 nucleic acid. Preliminary studies have shown that it can detect infection in respiratory samples, such as oropharyngeal, saliva, mucus (sputum), and bronchoalveolar lavage fluid (BAL). Moreover, it is also applied to detect SARS-C0v-2 in respiratory specimens. FAM-tagged primers and probes are being developed for the detection of SARS-Cov-2 (Open Reading Frame 1ab gene) SARS-Cov 2 N-gene and a human RNase P-gene, both extracted at the same time as the test sample, served as an internal control to verify the nucleic extraction method and reagent integrity. Marking a probe with CY5 allows it to specifically target the human RNase P gene as well as the nucleocapsid gene of the SARS-CoV-2 genome (N).
Protocol
All the reagents were thawed entirely before use, then vertex and spin down at 6000 rpm.
a- Extract RNA with a viral RNA extraction kit; positive control and negative control were used without extraction.
b- PCR tubes were prepared for reaction solution (N=negative control number + RNA sample number + positive control number) then 1.3 µl reaction solution and 1.7 µl enzyme mixture were added to each tube. 20 µl of RNA sample, negative control, and positive control were added to the PCR tubes, then capped tightly and centrifuged at 6000 rpm for 10 min. Then transported to the PCR amplification area. PCR tubes were disposed of in sealed bags after reaction and were treated as medical waste.
Settings for result analysis
The 3' end of the probe contains a quencher dye, whereas the 5' end contains a reporter dye. The quencher absorbs the reporter dye's fluorescence signals, making them invisible. Taq-DNA polymerase (5'-3'exonuclease) activity destroys probes coupled to amplified templates during the PCR amplification process. As a result, the fluorescence emissions rise with each cycle because the reporter dye and quencher are separated. Each optical channel in the PCR machine receives a real-time amplification curve, which is then used to compute the cycle threshold (Ct). The Ct values indicate the point at which the fluorescence is detectable above the background, and the operator uses those values to determine whether or not SARS-CoV-2RNA is present. Then qPCR master mix was prepared by using (Lifotronic® SARS-C0v-2 qPCR PreMix kit for nucleic acid determination. Multiplex PCR with fluorescent probes. China's Shanghai). The qPCR-master mix reaction has been made according to the kit's instructions. This reaction was performed in a thermocycler (mini-Opticon RT PCR, BioRadCFX96/USA) under the following criteria: initial-denaturation temperatures of 95°C for thirty minutes; followed by 30-cycles at 95°C for thirty seconds, annealed and extension 60 °C for 40-cycles.
The Statistical Analysis
The Statistical Analysis System- SAS (2012) program was used to detect the effect of different factors on study parameters. The Chi-square test was used to compare the percentage (0.05 and 0.01 probability) in this study 20.
RESULTS
Clinical findings
Fever, dry coughing, nasal congestion, muscle aches, weariness, runny nose, dyspnea, and sore throat were among the clinical symptoms reported by COVID-19 patients. Acute, severe, and mild clinical features were observed in specific individuals, as well as normal or reduced leukocyte levels and radiographic signs of pneumonia. Results are shown in table (1).
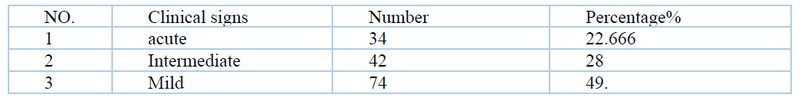
Table 1. Acute, severe, and mild clinical features were observed in specific individuals
Our findings revealed that 18 (22.666%) of the cases had symptoms such as fever, unproductive hacking, breathlessness, muscle aches, and weariness, Whereas 42 (28%) of patients had lesser symptoms, and 74 (49.333%) of cases had minor symptoms on their own. According to the F-test, the difference in clinical signs was important (p<0.05).
SARS-Cov-2 infection detection via spike (S) gene by RT-PCR
Since the kit uses a multiplex PCR technique, gene up-stream and down-stream ends of particular primers have been included using the spike (S) gene-specific primers.
SARS-Cov-2 infection detection via envelope (E) gene by RT-PCR
Although the kit uses a multiplex PCR technique, gene up-stream and down-stream ends of particular primers were incorporated using envelope (E) gene-specific primers.
DISCUSSION
Sensitivity and Specificity: 200 copies\ml no cross-reaction with SARS-Cov, MERS-Cov, Cov-HKU1, Cov-OC43, Cov-229E, Cov-NL63, and H1N1, H3N2, H5N1, H7N9, influenza-B, Para-influenza virus (1,2,3) , Rhinovirus (A,B, C), Adenovirus (1,2,3,4,5,7,55), Human interstitial pneumovirus, Human metapneumovirus, EBV, Measles virus, Human cytomegalovirus, Rotavirus, Norovirus 21.
Viral–cell membrane fusions are formed when SARS-CoV-2 S-protein engages host cell receptors, allowing the virus to enter. CoV-2's SARS infectivity is boosted by the S-affinity proteins for (ACE2). A better understanding of the virus's invasion and pathology could lead to developing antiviral medicines and tailored immunization programs. According to a study, the role of several viral proteins has not been well defined in the past. The viral life cycle continues despite the deletion of some viral genes, showing that other virus genes can recompense for this lack 22. This is also obvious in the varying E protein requirements for various CoV s, and the reason(s) for this is unclear. Deleting E-from SARS_CoV - 2 weakens the virus, while (MERS-CoV) virions are incapable of propagation 13, 23. In processes including Co-V assembly, release, and pathogenesis, Some Co-V accessories proteins seem to be capable of compensating for the lack of E 24,25. CoV2 E has been linked with numerous steps in the viral replication cycle: from initiation of membrane curvature and assembly to apoptosis or autophagy through the release of the virus from the host cell. Despite recent improvements in studying this protein, there is still much to learn about CoV-E.
The most common envelope protein of coronaviruses is a membrane (M)-glycoprotein. According to in silico research, the protein of (SARS-CoV-2M) is 98% similar to bat SARS-Co-V, 98% identical to pangolin SARS-CoV, and 90% similar to SARS-CoV; however, the protein of MERS-M CoV2 is only 38% comparable. WARNING: GRAPHIC CONTENT: SARS-CoV-2 M proteins are 96.2 % more compared to bats (Ra TG-13) and pangolins (Ra TG-11) than MERS-CoV. According to Zhang et al., the (M) protein is a key component of SARS-COV-2 in all variants. SARS-Co-V-2 is an example of an enveloped virus that releases its genetic material into the cell in a two-step process. First, they connect to specific receptors on the target cell membrane; second, they merge virus and cell membranes. This phase can occur at the cell surface or after the virus particle has been internalized by endocytic 26. The virus's M proteins have yet to be fused to the host cell membrane. The M-protein might hypothetically serve as a sugar transport if connected to the host cell membrane.ORF1ab, PP1ab and PP1a polyprotein are encoded by the most significant gene, which has overlapping ORF. The polyprotein is broken into NSP1-16, which are non - structural proteins. (SARS-CoV-2) nonstructural proteins were implicated in virus transcription, replication, proteolytic process, control of host immunological responses, and suppression of host gene expression. The RNA-dependent RNA polymerase is the target of antiviral medicines 27.
CONCLUSION
SARS-Cov-2 primer sets and FAM-labeled probes have been developed to detect SARS-Cov-2 (Open Reading Frame 1ab gene). Internal control using a VIC labeled probe for SARS-Cov 2 N-gene and human RNase P-gene extracted concurrently with the test sample to validate the integrity of the nucleic extraction technique and reagents. The findings of this study confirm that the studied genes are essential components of different variations of SARS-Cov-2 and that they have not undergone any changes or genetic variation in any of them, implying that the primers used for the detection of these genes in the molecular diagnosis of infection via multiplex PCR are accurate and reliable when combined with the clinical findings of the patients and that the variation in different strains of SARS-Cov-2 is based on this.
Acknowledgment: Thanks going for all who support us.
Conflict between authors: No conflict
Funds: self by authors
REFERENCES
1. Shahhosseini N, Babuadze GG, Wong G, Kobinger GP. Mutation signatures and in silico docking of novel SARS-CoV-2 variants of concern. Microorganisms. 2021;9(5):926.
2. Cox, Michael M. Molecular Biology: Principles and Practice. 41 Madison Avenue, New York, NY 10010: W. H. Freeman and Company. pp. 2015; 221–238, 369–376, 592–593.
3. Perchetti GA, Nalla AK, Huang ML, Jerome KR, Greninger AL. Multiplexing primer/probe sets for detection of SARS-CoV-2 by qRT-PCR". Journal of Clinical Virology. 2020;129: 104499.
4. Su S, Wong G, Shi W, et al. Epidemiology, Genetic recombination, and pathogenesis of coronaviruses. Trends Microbiol. 2016;49(6) 490-502.
5. Perlman S, Netland J. Coronaviruses post-SARS: update on replication and pathogenesis. Nature reviews microbiology. 2009 Jun;7(6):439-50.
6. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China. N Engl J Med. 2020;382:727–33.
7. Yuan Huang, Chan Yang, Xin-feng Xu, Wei Xu & Shu-wen Liu. Structural and functional properties of SARS-CoV-2 spike protein: potential antivirus drug development for COVID-19. Acta Pharmacologica Sinica 2020; volume 41, pages1141–1149.
8. Morse JS, Lalonde T, Xu S, Liu WR. Learning from the past: possible urgent prevention and treatment options for severe acute respiratory infections caused by 2019-nCoV. Chembiochem. 2020; 21:730–8.
9. Watanabe Y, Allen JD, Wrapp D, McLellan JS, Crispin M. Site-specific glycan analysis of the SARS-CoV-2 spike. Science. 2020; 369:330–3.
10. Schoeman D, Burtram C. Fielding. Coronavirus envelope protein: current knowledge; Virology Journal 2019; volume 16, Article number: 69.
11. Venkatagopalan P, Daskalova SM, Lopez LA, Dolezal KA, Hogue BG. Coronavirus envelope (E) protein remains at the site of assembly. Virology. 2015; 478:75–85.
12. Nieto-Torres JL, DeDiego ML, Álvarez E, Jiménez-Guardeño JM, Regla-Nava JA, Llorente M, et al. Subcellular location and topology of severe acute respiratory syndrome coronavirus envelope protein. Virology. 2011; 415(2):69–82.
13. DeDiego ML, Álvarez E, Almazán F, Rejas MT, Lamirande E, Roberts A, et al. A severe acute respiratory syndrome coronavirus that lacks the E gene is attenuated in vitro and in vivo. J Virol. 2017; 81(4):1701–13
14. Mousavizadeh L, Ghasemi S. Genotype and phenotype of COVID-19: Their roles in pathogenesis. J Microbiol Immunol Infect pii: 2020; S1684-1182(20)30082-7.
15. Astuti I, srafil Y. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2): An overview of viral structure and host response. Diabetes Metab Syndr 2020; 14:407–412.
16. Bianchi M, Benvenuto D, Giovanetti M, Angeletti S, Ciccozzi M, Pascarella S. Sars-CoV-2 envelope and membrane proteins: Structural differences linked to virus characteristics? Biomed Res Int 2020; 4389089.
17. Watanabe Y, Berndsen Z.T, Raghwani J, et al. Vulnerabilities in coronavirus glycan shields despite extensive glycosylation. Nat Commun a; 2020; 11, 2688.
18. Watanabe Y, Allen JD, Wrapp D, McLellan JS, Crispin M. Site-specific glycan analysis of the SARS-CoV-2 spike. Science b; 2020; 369: 330–333.
19. McBride R, van Zyl M, Burtram Fielding C. The Coronavirus Nucleocapsid Is a Multifunctional Protein. Viruses. Aug 2014; 6(8): 2991–3018.
20. SAS. 2012. Statistical Analysis System, User's Guide. Statistical. Version 9.1th ed. SAS. Inst. Inc. Cary. NC. USA.
21. Chao Jiang, Xingang Yao, Yulin Zhao, Jianmin Wu, a Pan Huang, a Chunhua Pan,D , Shuwen Liu,c, Chungen Pana. Comparative review of respiratory diseases caused by coronaviruses and influenza A viruses during epidemic season. Microbes Infect. 2020 July-August; 22(6): 236–244.Published online 2020 May 13.
22. Abidin AZ, DSouza AM, Nagarajan MB, Wang L, Qiu X, Schifitto G, et al. Alteration of brain network topology in HIV-associated neurocognitive disorder: a novel functional connectivity perspective. Neuroimage Clin. 2018; (17):768–77.
23. Liu B, Panda D, Mendez-Rios JD, Ganesan S, Wyatt LS, Moss B. Identification of Poxvirus Genome Uncoating and DNA Replication Factors with Mutually Redundant Roles. J Virol. 2018; 92(7):e02152–17.
24. Almazán F, DeDiego ML, Sola I, Zuñiga S, Nieto-Torres JL, Marquez-Jurado S, et al. Engineering a replication-competent, propagation-defective Middle East respiratory syndrome coronavirus as a vaccine candidate. MBio. 2013; 4(5):e00650–13.
25. Liu DX, Fung TS, Chong KK-L, Shukla A, Hilgenfeld R. Accessory proteins of SARS-CoV and other coronaviruses. Antivir Res. 2014; 109:97–109.
26. Zhang T, Wu Q, Zhang Z. Probable pangolin origin of SARS-CoV-2 associated with the COVID-19 outbreak. Curr Biol 2020; 6;30(7):1346–1351.e2.
27. White JM, Whittaker GR. Fusion of enveloped viruses in endosomes. Traffic 2016;17: 593–614.
Received: 13 March 2022 / Accepted: 25 July 2022 / Published:15 August 2022
Citation: Rasoul L M, Nsaif M M, Al-Tameemi M T, Laftaah Al-Rubaii B A. Estimation of primer efficiency in multiplex PCR for detecting SARS-Cov-2 variants. Revis Bionatura 2022;7(3) 49. http://dx.doi.org/10.21931/RB/2022.07.03.49
