2023.08.03.89
Files > Volume 8 > Vol 8 No 3 2023
Anthropometric indexes and cardiovascular risk in Ecuadorian university students: A comparison with international references
Silvia Cáceres-Vinueza1,2* , Evelyn Frias-Toral3*
, Evelyn Frias-Toral3* , Rosario Suárez4
, Rosario Suárez4 , Jorge Daher-Nader1
, Jorge Daher-Nader1 , Enrique Flor-Muñoz1
, Enrique Flor-Muñoz1 , Mirna Márquez-Vinueza5
, Mirna Márquez-Vinueza5 , Luisa Valeria Guevara-Flores6
, Luisa Valeria Guevara-Flores6 , Yan Duarte-Vera1,2
, Yan Duarte-Vera1,2
1 Ecuador. Faculty of Medical Science of the University of Guayaquil, Guayaquil, Ecuador
2 Ecuadorian Parenteral and Enteral Association. Ecuador.
3 Universidad Espíritu Santo, Samborondón, 0901952, Ecuador
4 School of Medicine, Universidad Técnica Particular de Loja, Calle París, San Cayetano Alto, Loja 110101, Ecuador.
5 Hospital of the Ecuadorian Institute of Social Security. Ceibos Norte, Guayaquil, Ecuador
6 School of Physical Education, Sports and Recreation Av. Delta, Guayaquil 090510, Ecuador
* Correspondence: [email protected]. [email protected].
Available from: http://dx.doi.org/10.21931/RB/2023.08.03.89
ABSTRACT
Some anthropometric measures help evaluate the cardiovascular (CV) risk and body fat areas considered more critical for CV risk than excess weight. This research aims to obtain anthropometric measurements from university students to establish risk predictors of cardio-metabolic alterations or cardiovascular disease (CVD). A descriptive cross-sectional study was carried out. Variables studied were height (m), weight (kg), body mass index (BMI), abdominal perimeter, waist-hip ratio (http://wsx5customurl.comWHR), and waist-to-height ratio (WHtR). One thousand two hundred fifty young adults participated; 62.4% were women, 31.04% were overweight, and 14.32% were obese. Mean values of all the evaluated parameters were lower in women than in men [height (1.58m vs. 1.70m), weight (61.46 kg vs. 76.38 kg), BMI (24.66 Kg/m2 vs. 26.32 Kg/m2), abdominal perimeter (78.49 cm vs. 88.81 cm), WHR (0.79 vs. 0.87), and WHtR (0.50 and 0.52)]. The mean BMI in men was overweight but normal in women. There were no significant differences between both genders concerning abdominal perimeter and WHR. Finally, mean WHtR was high in both women and men, establishing a prediction of CVD risk for both genders.
Keywords: Body Mass Index, Waist-Hip Ratio, Waist-Height Ratio, Medical Students, Cardiovascular Diseases, Cardiometabolic Risk Factors
INTRODUCTION
The fat compartment, adipose tissue, or storage fat representing 20% of an individual's weight comprises adipocytes1. Fat, also called fat tissue, which is usually considered metabolically inactive, has a critical reserve role and intervenes in hormone metabolism, among other functions2. According to its location, the fat found under the skin is called subcutaneous fat, and the one around the organs is fat of visceral or internal location 1 . Its excessive accumulation may be assessed through anthropometric measurements 3, 4 . Obesity is a chronic, multifactorial and complex disease that has become one of the world's most significant public health problems. Its increasing prevalence implies an increment in some of the most common diseases, such as diabetes, gestational diabetes mellitus, steatohepatitis, high BP (BP), sleep apnea syndrome, and atherogenic dyslipidemia, which are the cause of high cardiovascular morbidity and mortality 3-14.
Anthropometric indicators in some research can relate to body composition and assess the CVD risk for individuals with overweight or obesity 15 . For example, the Framingham study prospectively showed that for every 10% increase in weight, BP increases by 6.5 mmHg, plasma cholesterol by 12 mg/dl, and glycemia by 2 mg/dl 16 . Thus, central abdominal obesity is an indispensable criterion for diagnosing metabolic syndrome. Moreover, its presence, accompanied by a series of physical, physiopathological, and epigenetic manifestations17, provides an increased cardiovascular risk in all epidemiological series, both in developed countries and in countries such as Ecuador, in the developing world18, 19.
The WHR, also known as the Body Adiposity Index (BAI), accurately indicates visceral fat volume in the individual13, 20. Extensive studies have used it as an indicator of abdominal obesity and CV risk, especially the study by Salim Yusuf et al. (2004) called INTERHEART21, in which the WHR was shown to determine a gradual and highly significant association with the risk of myocardial infarction throughout the world. Furthermore, the redefinition of obesity based on WHR instead of BMI increases the estimate of myocardial infarction attributable to obesity in most ethnic groups13. Another large study that assessed WHR was the INTERSTROKE study, where this rate was determined to be a significant factor for ischemic stroke, and it was of significant risk for intracerebral hemorrhagic stroke 22 . This research was a standardized case-control study in 22 countries worldwide, being hypertension, smoking, waist-to-hip ratio waist-to-hip ratio (OR 1.65, 99% CI 1.36-1.99); 26.5%, 18.8-36.0, diet, and alcohol intake the most significant risk factors for intracerebral hemorrhagic stroke 23. Therefore, the WHR remains an essential anthropometric index in assessing some populations concerning CVD and endocrine risk factors 24, providing information on the possible development or future suffering of metabolic syndrome and other pathologies25-27.
There is contradictory information about BMI, which is ambiguous as a risk factor for CVD, being an anthropometric indicator inversely correlated with cholesterol-HDL and positively with arterial hypertension and body fat, so the indices to be studied provide beneficial information 28.
Finally, the information obtained by Bermúdez et al., in a cross-sectional study with 2.230 participants, where the application of BMI, abdominal circumference, WHR, and WHtR was estimated to identify which of these best-detected CVD. Their Analysis showed that the WHtR was the variable most associated with the presence of CV risk factors, demonstrating the positive predictive power of this index, proposing it as a good predictor of CV risk29. Additionally, it strongly correlates with BP in young adult subjects30. More recently, the WHtR has begun predicting metabolic risk over general obesity 31-33. Given that height hardly changes during the adult stage of life, it is assumed that the WHtR will change only when there is a change in the waist circumference measurement. In contrast, the WHR is more sensitive to changes in body size since both the waist and the hip increase or decrease proportionally 34.
On the other hand, the importance of age as an independent predictor factor for CVD is well known. The risks associated with CVD increase with age, mostly related to an overall decline in sex hormones, but less has been described CVD risk factors in young adults; however, they are not exempted from incident premature CVD, considering some group-related factors such as familial hypercholesterolemia, drug or tobacco consumption and elevated BP/hypertension, family history of premature atherosclerotic cardiovascular diseases (ASCVD) among others35. On the contrary, a prospective study on late adolescence or young adulthood has described that high cardiovascular health (CVH) is associated with meager rates of premature CVD and mortality over 32 years of follow-up. This research aims to analyze the body composition of university students, divided by gender, using different anthropometric indices to assess their nutritional status and the risk to their health or CVD since the latter are among the five leading causes of death in Ecuador.
MATERIALS AND METHODS
Subjects and study protocol
This is a descriptive character of cross-sectional and comparative study. It was conducted at the Center for the Prevention of CVD within the School of Medicine of the University of Guayaquil (FCM-UG), created to research cardiometabolic character. The data were collected directly by the investigators. University students from the FCM-UG were invited to participate in the study. The students were informed of the purpose of this study before giving their written consent. The Ethics Committee from Luis Vernaza Hospital in Guayaquil approved the study protocol. Also, it was certified by the National Agency for Regulation, Control, and Sanitary Surveillance (ARCSA). The study started data collection on July 5, 2017, on December 22, 2019.
The following inclusion criteria were considered: students of the FCM-UG, over 18 years old, signed informed consent and completed all the procedures established in the protocol. Subjects who did not match the inclusion criteria and refused to participate in the study were excluded from it. Considering these criteria, the population that participated in the study was 1450 subjects, 780 women and 470 men. (Supplementary Materials, S1).
Measurements and calculations
Anthropometry
The students were summoned for the evaluations between 07:00 am and 3:00 pm, fasting for 2 to 4 hours in comfortable clothes. Data were collected on age, gender, and semester level. Three measurements were taken, separated by two minutes, of their systolic and diastolic BP and pulse rate with an OMRON model HEM-741CINT automatic BP monitor, according to the AHA technique for monitoring BP. The anthropometric data were obtained by previously well-trained staff and researchers to minimize the coefficients of variation. The weight (kg) and height (cm) were assessed using a scale of 0.1 kg and a stadiometer of 1 mm, RICE LAKE brand. The person was measured barefoot with the heels together, arms next to the body, and the head in the Frankfurt position. The waist circumference was measured at an intermediate distance between the edge of the last rib and the iliac crest and the hip at the maximum posterior buttock bulge level, as previously reported 37-41.
It was taken using a SILUET HERGOM medical tape measure. The World Health Organization (WHO) sets the standard value at <82 cm and <95 cm, a high-risk value between 82 - 88 cm and 95 - 102 cm, and a very high risk >88 cm and >102 cm in women and men, respectively. The WHR obtained with the equation waist (cm) / hip (cm) was considered an index greater than 0.85 in women and 0.95 in men as the risk of CVD (14). BMI was calculated with the weight (kg) divided by the height (m) squared (kg / m2). The criteria used to define the nutritional category were those of the WHO, which considers overweight ≥ 25 kg/m2 and obesity when the BMI ≥ 30 kg / m2. Finally, the WHtR was established by dividing the waist circumference (cm) by the height (cm). As an independent predictor of CVD and dysglycemia, the optimal cut-off value of the WHtR was 0.50 in women and 0.49 in men. The population was divided into 2 groups, female and male, with a mean age of 23.09 (SD 2.83), ranging from 18 to 40 years.
Statistical Analysis
The results are expressed as means, standard deviations (±), and percentages when required. The Kolmogorov-Smirnov test assessed the normality of the variables. The Student t-test for unpaired data evaluated differences in anthropometric characteristics between genera (Table 1). Statistical significance was defined as a value of p <0.05. All the collected data were input into an Excel reference table, and the IBM SPSS 23 statistical system was used to conduct the statistical Analysis, the output of which would be tables and graphs exported in Word format.
RESULTS
Anthropometric variables showed normal behavior since they did not show statistically significant differences between the role of the empirical data and the normal distribution model. Table 1 shows the evaluated variables distributed by sex, where it is evident that women have a normal mean BMI while men are in the overweight range, according to the WHO classification. All anthropometric parameters found significant differences (p<0.05) between men and women. As expected, men were taller, heavier, and had higher BMI values. The WHtR is also statistically significant in favor of men, but its average level implies risk prediction in both genders.
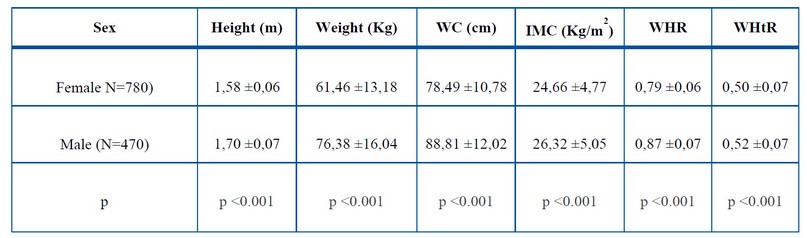
Table 1: Mean and standard deviation of variables distributed according to sex.
In table 2, it is specified according to the BMI categories. For female participants, it was found that most of the sample was located at the normal weight level, 56.3 %, in the category of low weight, which is also considered a risk to health (not related to this work), was 4.7 %.
Although 3 % of them were overweight, regarding obesity, they joined the category of obesity I-II-II in a single percentage, representing 12.7 %. These data show us that approximately 1 of every 4 women in this study is overweight, and more than 1 of each 10 presents some degree of obesity; according to this parameter, the female sample is considered relatively healthy. About the male sex, 42.6% had normal weight, only 1.5% were underweight, and 38 % were overweight. 9 % and 17 % had some degree of obesity, less than half of the university men evaluated were at the adequate weight level, a low percentage at the underweight level, and a little more than 55 % in the overweight and obesity categories. Hence, the male sample is presented as less healthy, considering many subjects with increased weight levels. If we consider the total number of students, it can be seen in Table 2 that 51% had normal weight, and 45% were overweight or obese. Thus, as a whole, it was not shown as a healthy population.
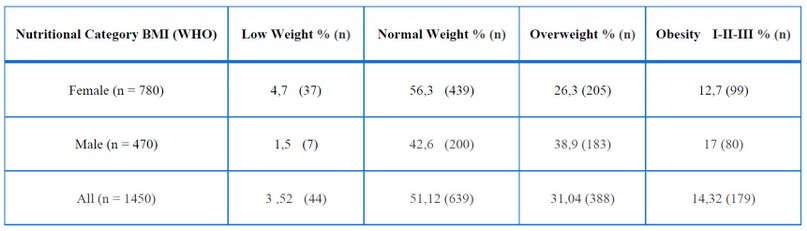
Table 2: Distribution of the sample by sex and according to BMI nutritional category
The distribution by gender according to their abdominal circumference and cardiometabolic risk category is established; in the group of women, 67.95% have a normal category, the high risk was present in 17.82%, and 14.23% are considered very high risk. On the other hand, in men, 72.98%, 14.26%, and 12.77% present a normal, high, and very high-risk category, respectively (Table 3).
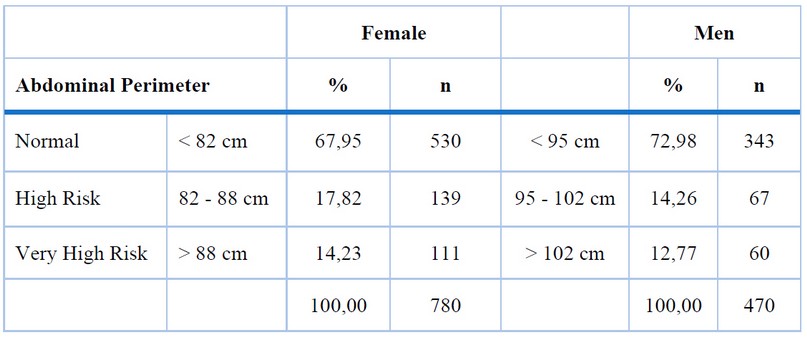
Table 3. Distribution of the sample by sex according to abdominal circumference and cardiometabolic risk category
Similarly, about WHR, 83.8% had no risk in the group of women, and only 16.2% had a CV risk level. (Figure 1); in the group of men, only 9.4% had a level of risk, and 90.6% had no risk. (Figure 2). Therefore, according to this anthropometric parameter, they were placed as a low-risk group for CVD.
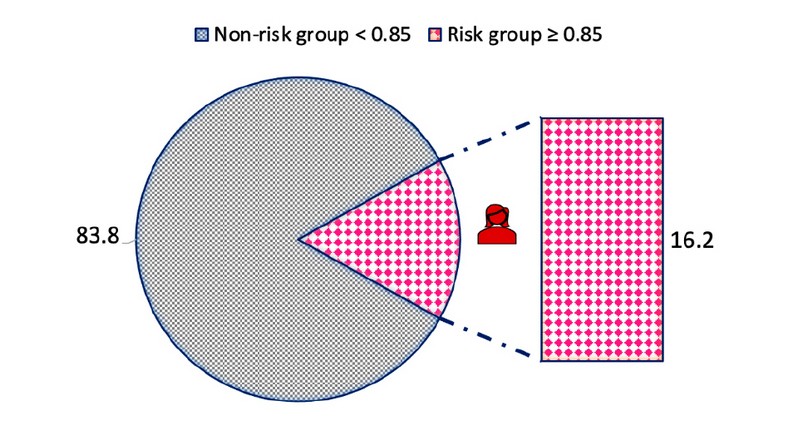
Figure 1. Distribution of the female group with the waist/hip index variable (WHR)
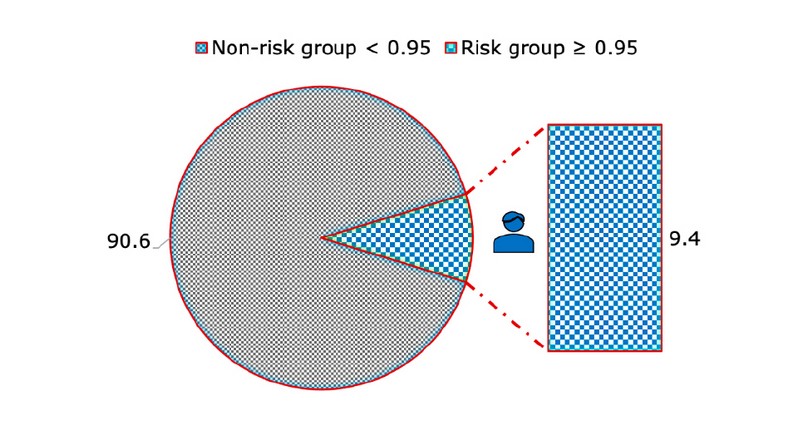
Figure 2. Distribution of the male group with the waist/hip index variable (WHR)
Finally, an anthropometric parameter that is less widely used in our environment but is scientifically supported is the WHtR 24. In university women, 49.4%, and in men, 57.2% had a cardiometabolic risk, according to this parameter (Figures 3 and 4). Therefore, these findings mean that a significant percentage could be at risk of the pathologies mentioned above, being in the area of health risk.
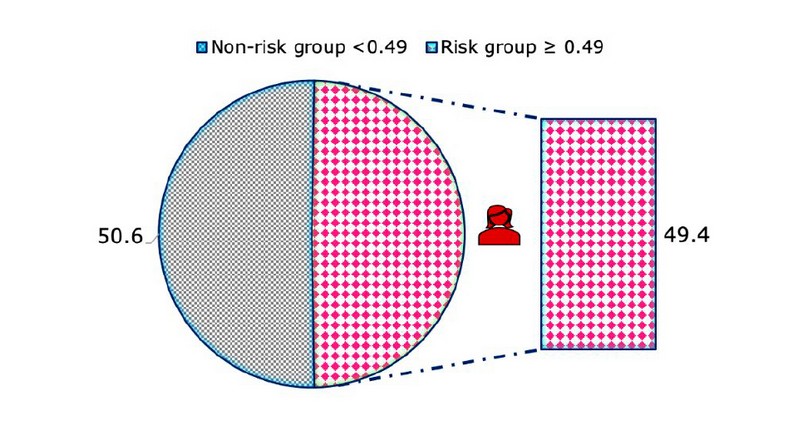
Figure 3. Distribution of the female group with the waist/height index variable (WHtR)
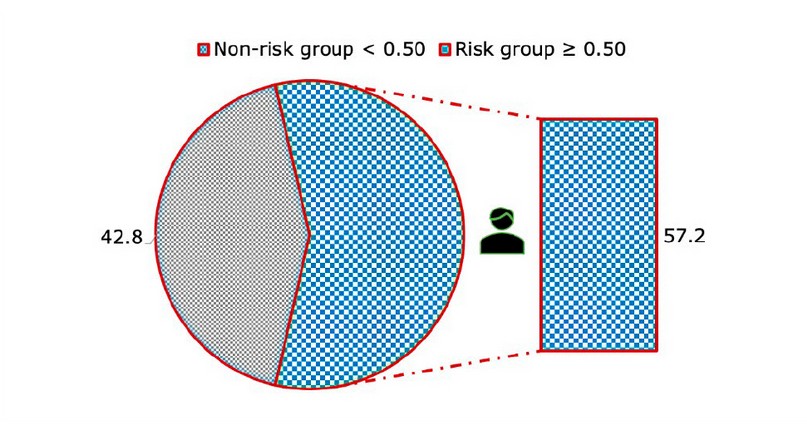
Figure 4. Distribution of the male group with the waist/size index variable (WHtR)
DISCUSSION
The presence of overweight and obesity is associated with multiple conditions that affect health. The anthropometric indicators that define obesity help to identify individuals or populations exposed to a particular risk of experiencing various health problems. When evaluating the diagnosis of the possibility of developing CVD due to BMI, an average of 24.66 and 26.32 kg/m2 was established in women and men, respectively. In the sample of university women, it is noteworthy that overweight and obesity make up 39%, while in the male group, it is 56%, significantly higher in men. The same occurs when both genders are added together. This result is higher than those reported in Mexican university students with an average age slightly younger than 20.9 years, where a result of 31.6% was obtained, corresponding to an overweight and obesity category 43 .
Similarly, our sample shows more overweight or obesity than the study in university engineering students with 334 participants. The women obtained an average of 21.9 kg/m2, where 15.8% were overweight and obese; likewise, men reached a BMI of 23.9 kg/m2, while 32.9% presented overweight or obesity figures. Compared to this study conducted at the University of Carabobo, our results are higher in a population of students of both genders with equal average age, where the male group had an excess weight of 51.9%. In comparison, the female group had 19.1 %44 . In the present report, the results of overweight or obesity of a total of 1450 students of the FCM-UG surpass those obtained by Arroyo M. et al.45 , Boutahar K. et al.46 , Soto N. et al.47 and López-Sánchez et al.48 , obtained 10.7 %, 11.4 %, 18.4 %, and 22.75 %, respectively.
About the WHR, as in other research carried out in populations similar to ours, the values obtained for most subjects were within normal limits: 83.5 % in women and 90.6 % in men. Only 16.2 % of women and 9.4 % of men were in the CV risk category. These WHR data are also similar to the Raya-Cano et al. study49, in which 98.7% of women and 96.0% of men presented values lower than those considered at risk. Thus, this anthropometric measure should not be used to classify them as at-risk populations. This research is related to the work of López-Sánchez et al.48, which was carried out with university students in Madrid, where both genders obtained values within the ranges reported as normal, in addition to having a slightly lower average age (22 years) and not considering this sample as being at risk of suffering CVD.
The WHtR assessment showed that 51.5% and 60.9% of women and men, respectively, were in the normal range, which means that more than half of the university population has abdominal obesity and the future possibility of CVD using this anthropometric measure. On the other hand, it was very challenging to find studies with this variable in university students 50; one of the few is the study by Corvos et al.44, where only 13.5% of the sample studied presents high values, comparatively lower than those found in our Faculty.
One of the highlights of the current report is that it includes a significant number of university students that surpassed the sample we had taken as a goal of 687 students for a population of 6500 students of the FCM-UG. It additionally represents the initial research project to assess the relationship of different anthropometric measures, including WHtR, to determine the health of university students in Ecuador. However, the limitations inherent in being a cross-sectional study therefore, the direction of the association is subject to uncertainty, without establishing definitive judgments of causality due to temporal ambiguity. Other limitations are that it only included young adults and that nutrition habits were not assessed, which could be investigated in future research since this is an important parameter to consider when evaluating CD risk, as well as the use of anti-obesity drugs, physical activity level, smoking, stress, and inadequate sleeping 51.
CONCLUSIONS
There are significant differences between the anthropometric measures between women and men. The average BMI in men determines a category of overweight in this population. There were no differences in the average abdominal perimeter and WHR; both were within normal parameters. Remarkably, the altered average of the WHtR in both women and men predicts CVD risk. These findings mean that more than half of the university population presents abdominal obesity and risk of CVD using this anthropometric measure. Furthermore, indicators of abdominal obesity showed a more significant association with cardiometabolic risk. Therefore, strategies such as comprehensive nutrition talks are accompanied by anti-obesity drugs, depending on the case and counseling in being physically active, not smoking, managing stress and getting enough sleep, following most important AHA recommendations.
Supplementary Materials: Figure S1: Flowchart of study participants
Author Contributions: Substantial contributions to the conception or design of the work: SC, EFT and YD; the acquisition, Analysis, or interpretation of data for the work: JD, EF, MM; Drafting the work or revising it critically for important intellectual content: SC, EFT, RS and YD; Final approval of the version to be published: YD; agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: SC, EFT, RS and YD. All authors read and approved the final manuscript.
Funding: This research has not received specific grants from public, commercial, or non-profit agencies.
Institutional Review Board Statement: "The study was conducted according to the guidelines of the Declaration of Helsinki and approved by The Ethics Committee from Luis Vernaza Hospital in Guayaquil. Also, it was certified by the National Agency for Regulation, Control, and Sanitary Surveillance (ARCSA).
Informed Consent Statement: Informed consent was obtained from all subjects involved in the study
Data Availability Statement: This section provides details regarding where data supporting reported results can be found, including links to publicly archived datasets analyzed or generated during the study. Please refer to the suggested Data Availability Statements in the "Bionatura Research Data Policies" section at https://www.revistabionatura.com/policies.html. You might exclude this statement if the study did not report any data.
Acknowledgments: none
Conflicts of Interest: The authors have nothing to disclose.
REFERENCES
1. Rosen ED, Spiegelman BM. What we talk about when we talk about fat. Cell. 2014;156(1-2):20-44. doi:10.1016/J.CELL.2013.12.012
2. de Arriba Muñoz A, López Úbeda M, Rueda Caballero C, Labarta Aizpún JI, Ferrández Longás Á. Valores de normalidad de índice de masa corporal y perímetro abdominal en población española desde el nacimiento a los 28 años de edad. Nutr Hosp. 2016;33(4):887-893. doi:10.20960/NH.388
3. Latorre-Román PÁ, Martínez-López EJ, Ruiz-Ariza A, Izquierdo-Rus T, Salas-Sánchez J, García-Pinillos F. Validez y fiabilidad del cuestionario de disfrute por el ejercicio físico (PACES) en adolescentes con sobrepeso y obesidad. Nutr Hosp. 2016;33(3):595-601. doi:10.20960/NH.266
4. Brown RE, Randhawa AK, Canning KL, et al. Waist circumference at five common measurement sites in normal weight and overweight adults: which site is most optimal? Clin Obes. 2018;8(1):21-29. doi:10.1111/COB.12231
5. Šimják P, Anderlová K, Cinkajzlová A, Pařízek A, Kršek M, Haluzík M. The possible role of endocrine dysfunction of adipose tissue in gestational diabetes mellitus. Minerva Endocrinol. 2020;45(3):228-242. doi:10.23736/S0391-1977.20.03192-2
6. García-Álvarez M, Climent V. Sleep apnea and cardiovascular complications of the acromegaly. Response to the medical treatment. Minerva Endocrinol. 2019;44(2). doi:10.23736/S0391-1977.18.02930-9
7. Kinlen D, Cody D, O’Shea D. Complications of obesity. QJM. 2018;111(7):437-443. doi:10.1093/QJMED/HCX152
8. Mariscalco G, Wozniak MJ, Dawson AG, et al. Body Mass Index and Mortality Among Adults Undergoing Cardiac Surgery: A Nationwide Study With a Systematic Review and Meta-Analysis. Circulation. 2017;135(9):850-863. doi:10.1161/CIRCULATIONAHA.116.022840
9. Tinsley GM, La Bounty PM. Effects of intermittent fasting on body composition and clinical health markers in humans. Nutr Rev. 2015;73(10):661-674. doi:10.1093/NUTRIT/NUV041
10. Sepúlveda Cáceres X, Méndez Cornejo J, Duarte Farfán C, et al. [Relationship between body adiposity and horizontal jump in school children and adolescents]. Rev Chil Pediatr. 2018;89(6):0-0. doi:10.4067/S0370-41062018005001003
11. Connolly LJ, Nordsborg NB, Nyberg M, Weihe P, Krustrup P, Mohr M. Low-volume high-intensity swim training is superior to high-volume low-intensity training in relation to insulin sensitivity and glucose control in inactive middle-aged women. Eur J Appl Physiol. 2016;116(10):1889-1897. doi:10.1007/S00421-016-3441-8
12. Zaki ME, Kamal S, Reyad H, et al. The Validity of Body Adiposity Indices in Predicting Metabolic Syndrome and Its Components among Egyptian Women. Open Access Maced J Med Sci. 2016;4(1):25-30. doi:10.3889/OAMJMS.2016.036
13. Martín-Castellanos Á, Armesilla MDC, Durán FJB, Castellanos PM, Barrado JJG. [Obesity and risk of myocardial infarction in a sample of European males. Waist to-hip-ratio presents information bias of the real risk of abdominal obesity]. Nutr Hosp. 2017;34(1):88-95. doi:10.20960/NH.982
14. Porto-Arias JJ, Lorenzo T, Lamas A, Regal P, Cardelle-Cobas A, Cepeda A. Food patterns and nutritional assessment in Galician university students. J Physiol Biochem. 2018;74(1):119-126. doi:10.1007/S13105-017-0582-0
15. Borel AL, Coumes S, Reche F, et al. Waist, neck circumferences, waist-to-hip ratio: Which is the best cardiometabolic risk marker in women with severe obesity? The SOON cohort. PLoS One. 2018;13(11). doi:10.1371/JOURNAL.PONE.0206617
16. Hiriart-Urdanivia M, Sánchez-Soto C, Velasco M, Sabido-Barrera J, Ortiz-Huidobro RI. El receptor soluble de insulina y el síndrome metabólico. Gac Med Mex. 2019;155(5):541-545. doi:10.24875/GMM.19005185
17. Doulberis M, Papaefthymiou A, Polyzos SA, et al. Rodent models of obesity. Minerva Endocrinol. 2020;45(3):243-263. doi:10.23736/S0391-1977.19.03058-X
18. Miguel-Soca PE. Alteraciones metabólicas durante la obesidad. Salud Publica Mex. 2014;56(6):572-573. Accessed April 2, 2023. https://pubmed.ncbi.nlm.nih.gov/25604404/
19. Karatas O, Calan M, Yuksel A, et al. The level of the neudesin in Type-2 Diabetic patients and the relationship between the metabolic parameters and carotid intima-media thickness. Minerva Endocrinol. Published online January 2021. doi:10.23736/S0391-1977.20.03217-4
20. Asif M, Aslam M, Altaf S, Mustafa S. Developing waist circumference, waist-to-height ratio percentile curves for Pakistani children and adolescents aged 2-18 years using Lambda-Mu-Sigma (LMS) method. J Pediatr Endocrinol Metab. 2020;33(8):983-993. doi:10.1515/JPEM-2019-0527
21. Yusuf PS, Hawken S, Ôunpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937-952. doi:10.1016/S0140-6736(04)17018-9
22. Langhorne P, O’Donnell MJ, Chin SL, et al. Practice patterns and outcomes after stroke across countries at different economic levels (INTERSTROKE): an international observational study. Lancet. 2018;391(10134):2019-2027. doi:10.1016/S0140-6736(18)30802-X
23. O'Donnell MJ, Denis X, Liu L, et al. Risk factors for ischaemic and intracerebral hemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010;376(9735):112-123. doi:10.1016/S0140-6736(10)60834-3
24. Rhee EJ, Cho JH, Kwon H, et al. Relation between Baseline Height and New Diabetes Development: A Nationwide Population-Based Study. Diabetes Metab J. 2019;43(6):794-803. doi:10.4093/DMJ.2018.0184
25. Ma C, Lu Q, Wang R, Yin F. Using height-corrected definition of metabolic syndrome in children and adolescents. J Pediatr Endocrinol Metab. 2019;32(5):429-438. doi:10.1515/JPEM-2018-0414
26. de Oliveira RG de, Guedes DP. Performance of anthropometric indicators as predictors of metabolic syndrome in Brazilian adolescents. BMC Pediatr. 2018;18(1). doi:10.1186/S12887-018-1030-1
27. Liu X, Li X, Li C, Gong C, Liu S, Shi Y. Study on regulation of adipokines on body fat distribution and its correlation with metabolic syndrome in type 2 diabetes mellitus. Minerva Endocrinol. 2019;44(3):259-263. doi:10.23736/S0391-1977.17.02773-0
28. Diemer FS, Brewster LM, Haan YC, Oehlers GP, van Montfrans GA, Nahar-van Venrooij LMW. Body composition measures and cardiovascular risk in high-risk ethnic groups. Clin Nutr. 2019;38(1):450-456. doi:10.1016/J.CLNU.2017.11.012
29. Bermúdez V, Salazar J, Rojas J, et al. Diabetes and Impaired Fasting Glucose Prediction Using Anthropometric Indices in Adults from Maracaibo City, Venezuela. J Community Health. 2016;41(6):1223-1233. doi:10.1007/S10900-016-0209-3
30. Zhang Q, Mahapatra T, Huang F, et al. Association between Anthropometric Measures and Indicators for Hypertension Control among Kazakh-Chinese Hypertension Patients in Xinjiang, China: Results from a Cross-sectional Study. PLoS One. 2017;12(1). doi:10.1371/JOURNAL.PONE.0170959
31. Song YM, Sung J, Lee K. Associations Between Adiposity and Metabolic Syndrome Over Time: The Healthy Twin Study. Metab Syndr Relat Disord. 2017;15(3):124-129. doi:10.1089/MET.2016.0100
32. Yang XY, Zhang M, Luo XP, et al. [Body mass index, waist circumference and waist-to-height ratio associated with the incidence of type 2 diabetes mellitus: a cohort study]. Zhonghua Yu Fang Yi Xue Za Zhi. 2016;50(4):328-333. doi:10.3760/CMA.J.ISSN.0253-9624.2016.04.009
33. Sangrós FJ, Torrecilla J, Giráldez-García C, et al. Association of General and Abdominal Obesity With Hypertension, Dyslipidemia and Prediabetes in the PREDAPS Study. Rev Esp Cardiol (Engl Ed). 2018;71(3):170-177. doi:10.1016/J.REC.2017.04.035
34. Aranceta-Bartrina J, Pérez-Rodrigo C, Alberdi-Aresti G, Ramos-Carrera N, Lázaro-Masedo S. Prevalence of General Obesity and Abdominal Obesity in the Spanish Adult Population (Aged 25-64 Years) 2014-2015: The ENPE Study. Rev Esp Cardiol (Engl Ed). 2016;69(6):579-587. doi:10.1016/J.REC.2016.02.009
35. Rodgers JL, Jones J, Bolleddu SI, et al. Cardiovascular Risks Associated with Gender and Aging. J Cardiovasc Dev Dis. 2019;6(2). doi:10.3390/JCDD6020019
36. Perak AM, Ning H, Khan SS, et al. Associations of Late Adolescent or Young Adult Cardiovascular Health With Premature Cardiovascular Disease and Mortality. J Am Coll Cardiol. 2020;76(23):2695-2707. doi:10.1016/J.JACC.2020.10.002
37. Muscogiuri G, Barrea L, Di Somma C, et al. Sex Differences of Vitamin D Status across BMI Classes: An Observational Prospective Cohort Study. Nutrients. 2019;11(12). doi:10.3390/NU11123034
38. Barrea L, Muscogiuri G, Di Somma C, et al. Coffee consumption, metabolic syndrome and clinical severity of psoriasis: good or bad stuff? Arch Toxicol. 2018;92(5):1831-1845. doi:10.1007/S00204-018-2193-0
39. Barrea L, Di Somma C, Macchia PE, et al. Influence of nutrition on somatotropic axis: Milk consumption in adult individuals with moderate-severe obesity. Clin Nutr. 2017;36(1):293-301. doi:10.1016/J.CLNU.2015.12.007
40. Barrea L, Tarantino G, Somma C Di, et al. Adherence to the Mediterranean Diet and Circulating Levels of Sirtuin 4 in Obese Patients: A Novel Association. Oxid Med Cell Longev. 2017;2017. doi:10.1155/2017/6101254
41. Savastano S, Di Somma C, Colao A, et al. Preliminary data on the relationship between circulating levels of Sirtuin 4, anthropometric and metabolic parameters in obese subjects according to growth hormone/insulin-like growth factor-1 status. Growth Horm IGF Res. 2015;25(1):28-33. doi:10.1016/J.GHIR.2014.10.006
42. Behboudi-Gandevani S, Ramezani Tehrani F, Cheraghi L, Azizi F. Could “a body shape index” and “waist to height ratio” predict insulin resistance and metabolic syndrome in polycystic ovary syndrome? Eur J Obstet Gynecol Reprod Biol. 2016;205:110-114. doi:10.1016/J.EJOGRB.2016.08.011
43. Gómez-Landeros O, Galván-Amaya G del C, Aranda-Rodríguez R, Herrera-Chacón C, Granados-Cosme JA. [Prevalence of overweight, obesity and history of chronic disease in Mexican students]. Rev Med Inst Mex Seguro Soc. 2019;56(5):462-467. Accessed April 3, 2023. https://pubmed.ncbi.nlm.nih.gov/30777414/
44. Corvos CA, Corvos A, Salazar A. Índices antropométricos y salud en estudiantes de ingeniería de la Universidad de Carabobo. Nutricion Clinica y Dietetica Hospitalaria. 2014;34(2):45-51. doi:10.12873/342carabobocorvos
45. Arroyo Izaga M, Ansotegui L, Pereira E, et al. [Body composition assessment and body image perception in a group of University females of the Basque Country]. Nutr Hosp. 2008;23(4):366-372. Accessed April 3, 2023. https://pubmed.ncbi.nlm.nih.gov/18604323/
46. Boutahar K, Chetoui A, Kaoutar K, Najimi M, Chigr F. Anthropometric status and body image perception among Moroccan university students. Rev Epidemiol Sante Publique. 2019;67(5):311-317. doi:10.1016/J.RESPE.2019.04.057
47. Nelia Soto Ruiz M, Fernández BM, Ontoso IA, et al. [Analysis of body image perception of university students in navarra]. Nutr Hosp. 2015;31(5):2269-2275. doi:10.3305/NH.2015.31.5.7418
48. López-Sánchez G, Radzimiński Ł, Skalska M, et al. Body Composition, Physical Fitness, Physical Activity and Nutrition in Polish and Spanish Male Students of Sports Sciences: Differences and Correlations. Int J Environ Res Public Health. 2019;16(7):1148. doi:10.3390/IJERPH16071148
49. Raya-Cano E, Molina-Recio G, Romero-Saldaña M, Álvarez-Fernández C, Hernández-Reyes A, Molina-Luque R. [Comparison of classic and new anthropometric indexes for the screening of metabolic syndrome on the working population]. Rev Esp Salud Publica. 2020;94. Accessed April 3, 2023. https://pubmed.ncbi.nlm.nih.gov/32493897/
50. Tian Q, Wang H, Kaudimba KK, et al. Characteristics of Physical Fitness and Cardiometabolic Risk in Chinese University Students with Normal-Weight Obesity: A Cross-Sectional Study. Diabetes Metab Syndr Obes. 2020;13:4157-4167. doi:10.2147/DMSO.S280350
51. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults a report of the American College of Cardiology/American Heart Association Task Force on Clinical practice guidelines. Hypertension. 2018;71(6):E13-E115. doi:10.1161/HYP.0000000000000065
Received: 25 June 2023/ Accepted: 26 August 2023 / Published:15 September 2023
Citation: Cáceres-Vinueza S, Frias-Toral E, Suárez R, Daher-Nader J, Flor-Muñoz E, M Márquez-Vinueza, Guevara-Flores L V, Duarte-Vera Y. Anthropometric indexes and cardiovascular risk in Ecuadorian university students: A comparison with international references. Revis Bionatura 2023;8 (3) 89 http://dx.doi.org/10.21931/RB/2023.08.03.89
