2023.08.02.47
Files > Volume 8 > Vol 8 No 2 2023
Estimation of Immunological and Physiological Parameters in Diabetic Patients with COVID-19
Hayder Fadhil Okab1,*, Hussam Khazaal Yassir1 and Marwa Mohammed Majed1
1 Thi-Qar Health Office, Ministry of Health, Iraq
Correspondance author: [email protected]
Available from: http://dx.doi.org/10.21931/RB/2023.08.02.47
ABSTRACT
The covid-19 pandemic affects the world. It has spread to more than 200 countries and threatens the lives of millions. Diabetes affects people all over the world, especially in developing countries. Nowadays, diabetes and COVID-19 are major global health concerns. Evidence regarding the impact of diabetes and COVID-19 is limited in the literature. It is unclear whether or not people with diabetes have an increased tendency toward COVID-19. However, risk factors lead to higher mortality rates among patients with diabetes and COVID-19. The physiological and immunological parameters involved in the current study included high sensitivity to CRP (Hs-CRP), fasting blood sugar (FBS), insulin, Homo IR, and interleukin-10 (IL-10). A spectrophotometer analyzed FBS, while ELISA performed other parameters. The results showed a significant increase in all immunological and physiological parameters of patients compared with the control group in both categories of total comparison and sex comparison. In the same way, the results recorded a significant increase in all parameters of patients whose condition is critically compared with severe conditions, except Hs-CRP did not record significant differences; on the other hand, the study did not show significant differences in patients according to age groups. The current study showed a positive relationship between insulin and homo IR; between insulin and interleukin-10, the concentration of FBS and IL-10 increases with disease severity.
Keywords: Covid-19, Diabetic, IL-10, Hs-CRP, Insulin, Homo-IR.
INTRODUCTION
The Human Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV-2) was detected first in September 2019 in female patients in Wuhan (Hubei Province, China) suffered from Sevier respiratory illness and that disease has been popularized as corona-virus disease or COVID-19. The disease was declared an international public health emergency on January 30, 2020; a few months later, on March 11, 2020, it was declared a pandemic by the World Health Organization1. In patients with COVID-19, an excessive or un-controlled innate immune response leads to cytokine storm status and acute respiratory distress syndrome; the S protein of COVID-19 ligament to the angiotensin-converting enzyme receptor (ACE2) on the host cell and causes it to appear of genomic RNA (dsRNA) in the cytoplasm of the infected host cell 2. Type DM2 is a chronic disease characterized by abnormal hyperglycemia resulting from impaired insulin action and secretion 3. A piece of evidence for increased inflammation in T2D individuals, based on the presence of a higher percentage of CD8+ T cells, an increase in the Th1/Th2 ratio, and elevated levels of cytokines such as IL-10, IL-4, IL-13, IFN-γ, and TNF-α 4.
Diabetes mellitus and its level of hyperglycemia are associated with an elevated risk of COVID-19 and mortality and morbidity 5. Recent studies recorded that typical complications of diabetes, such as cardiovascular disease and chronic kidney disease, increase the risk of COVID-19 morbidity and mortality.3 A possible reason for this increased risk may be high blood glucose supporting the proliferation of the virus 6,7. Insulin is a powerful anabolic hormone that stimulates glucose uptake in adipocytes and skeletal muscle cells, promotes glycogen synthesis in skeletal muscle, inhibits hepatic glucose production, and inhibits lipolysis in adipocytes 8. In the presence of insulin resistance and hyperglycemia, the standard insulin signaling pathways in metabolic and cardiovascular tissues are affected, contributing to the interrelationship between insulin resistance and endothelial dysfunction 3.
So far, it is still unclear whether individuals with diabetes have a higher susceptibility to COVID-19 or not. However, there is a perception that the risks of infection and severe disease are higher in individuals with diabetes. A meta-analysis included 1527 patients with COVID-19 reported that the prevalence of diabetes was 9.7% and that the incidence of diabetes in severe and critical status was twice that of their uninfected counterparts 9. In a recent study on a small group in Wuhan, diabetes accounted for approximately 20% of intensive care unit admissions 10. More recent data from Italy showed that more than two-thirds of those who died from COVID-19 had diabetes11. Thus, exploring the clinical characteristics of COVID-19 patients with diabetes will reduce the incidence of severity. We conducted a single-center retrospective study of 50 confirmed cases of COVID-19 to discuss the relationship between diabetes and secondary hyperglycemia and COVID-19, along with potential response mechanisms.
MATERIALS AND METHODS
Sample Collection
The current study was conducted at Al-Hussein Teaching Hospital for COVID-19 patients in Thi-Qar Province and included 50 T2DM patients who have Covid-19 infection and 25 as a control group, the patient information was collected; for example, demographic data, CT scan results of the chest, and clinical features included fever, fatigue, cough, chest tightness, shortness of breath, diarrhea, and other symptoms, and according to this symptoms the respiratory physician classified patients into critical and severe cases. The laboratory tests included high-sensitivity CRP (Hs-CRP), Fasting blood sugar (FBS), insulin, Homo IR and interleukin-10 (IL-10). A spectrophotometer analyzed the FBS, and an ELISA conducted the other rest.
Statistical analyses
The current data were analyzed by SPSS version 26 statistical software using One-way ANOVA, Independent t-test and Person correlation at p. value < 0.05.
RESULTS
Immuno-physiological Parameters Comparison between DM2 Group and Control Group
The statistical results recorded a highly significant difference in immunological and physiological parameters in the DM2 group compared with the control group at p. value < 0.01, as shown in Table 1.
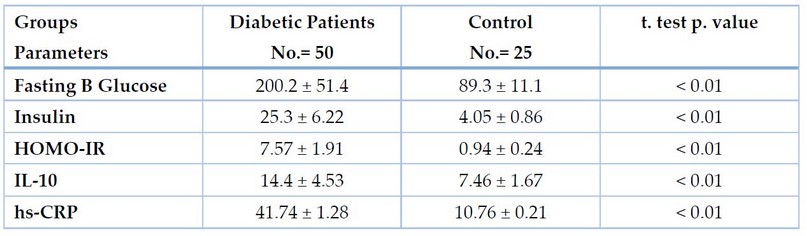
Table 1. Immuno-physiological comparison between DP and Control
Immuno-physiological Parameters Comparison between DM2 Group and Control According to Gender
The statistics of the current study illustrated a highly significant increase in both immunological and physiological parameters in both gender of the DM2 group compared with the matching gender of the control group at p. value < 0.01, as shown in Table 2
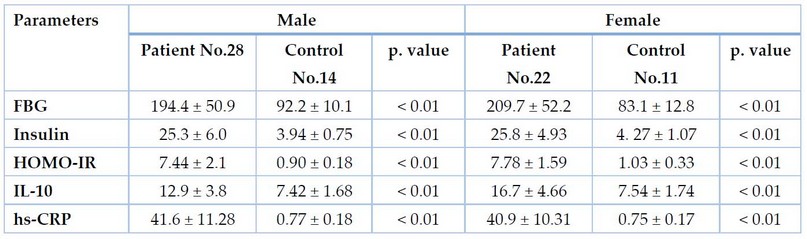
Table 2. Immuno-physiological Parameters Comparison between DP and control groups according to gender
Immuno-physiological Parameters Comparison between DM2 Group according to Disease Severity
According to disease severity, The current results indicated a highly significant increase in DM2 with critical status compared with severity status. In contrast, Hs-CRP did not record significant differences at p. value < 0.05, as shown in Table 3.
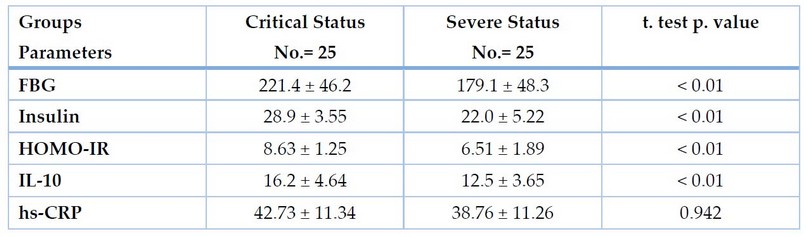
Table 3. Immuno-physiological comparison between DM2 Group according to disease severity
Immuno-physiological Parameters Comparison between DM2 Group according to Age Groups
The current results indicated, according to age groups of patients, a non-significant difference between all studied parameters according to age groups in DM2P at p. value < 0.05. as shown in Table 3-4.
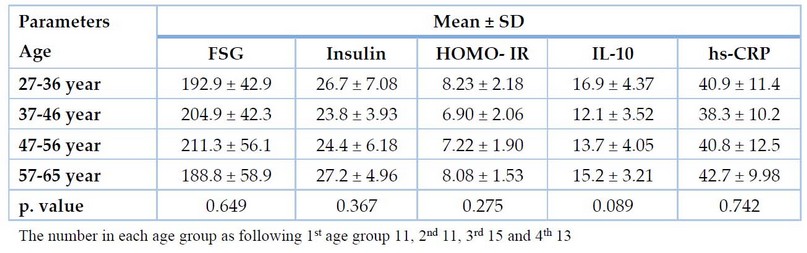
Table 4. Immuno-physiological comparison between DM2 Group according to age groups
DISCUSSION
COVID-19 is a highly infectious disease characterized by a high prevalence of infection and mortality, especially for individuals who have the chronic disease as diabetes, cardiovascular disease, kidney failure and autoimmune disease 12, there the current study focused on patients who also suffer from chronic diabetes milieus. The receptor for severe acute respiratory syndrome coronavirus is the angiotensin-converting enzyme 2 (ACE2) receptor, widely distributed in the kidneys, heart, intestines, etc., and is considered a significant receptor for SARS-CoV-2. COVID-19 is to bind to ACE2 receptors located in the cell membrane of respiratory and pulmonary epithelial cells, causing respiratory infections, as well as those in islets that lead to islet cell infection and increased blood glucose due to insulin metabolism dis-regulation 13.
The current results illustrated that diabetic patients have high levels of blood glucose, insulin and Homo IR. Also, the study recorded non-significant differences between patients according to age groups and gender; the diabetic patients also have levels of proinflammatory Hs-CRP and interleukin-10. In the study of Najim 14, he studied hyperglycemia, hydroxychloroquine, and the COVID‐19 pandemic, and their study illustrated that patients in ICU have higher glucose parameters than both patients in moderate and severe cases. The study of Chakraborty 15 investigated that both Hs-CRP and IL-10 significantly increased in diabetic patients with severe status than in moderate and control groups.
The study of Pakpour 16 showed a highly significant immunological effect on diabetes, and Covid-19 represents a major challenge globally due to the high mortality among the seriously ill. The study of Ajeel 17 showed that Covid-19 patients infected with T2DM were highly significant with the current study. It had adverse outcomes, which may result from deteriorating inflammation, impaired immunity, and worsening liver function compared to non-diabetics. Among the infected COVID-19 patients with T2DM, ICU admission rate, while hospital use of insulin, was a risk to increase invasive ventilation after adjusting for age and blood glucose. Also, the study showed highly significant with 17; this study showed COVID-19 may increase the risk of insulin resistance in patients without pre-existing diabetes. At the same time, the results also indicate that there may be decreases in insulin secretion with SARS-CoV-2 infection, although these decreases could be transient and reversible; thus, it is suggested that parameters regarding insulin sensitivity and pancreatic. The current study also recorded a positive correlation between hyperglycemia and increased insulin resistance with the severity of status and increased morbidity; a study performed by 18, indicated that high intracellular blood sugar leads to increased mitochondrial production of superoxide, which in turn activates multiple pathways through which hyperglycemia can lead to toxic effects on the brain either directly, by causing neuronal dysfunction and death cells, or indirectly, by stimulating micro-vascular and macro-vascular damage.
Diabetic patients with Covid-19 are exposed to hypoxia due to impaired function of the lung, with an increase in blood glucose, and this leads to cells not receiving glucose due to the decreased level of oxygen required by mitochondria, which leads to its remaining in the blood and hyperglycemia and this leads to complications such as brain membrane injures, cardiac muscle injuries kidney failure.
CONCLUSION
The current study concluded that people with diabetes are considered a risk factor for Covid 19 due to the high level of secondary sugar due to infection, and it was also noted that people with diabetes have an immune disorder due to the immune storm caused by the virus.
REFERENCES
1. B. Crespo-Facorro, J. Vázquez-Bourgon, C. A. Sánchez-Hidalgo, N. Garrido-Torres, M. J. Cisneros, C. Prieto, and J. Sainz “Aripiprazole as a Candidate Treatment of COVID-19 Identified Through Genomic Analysis,” Front. Pharmacol., 2021; 12(3), pp. 1–8.
2. A. O. Ferreira, H. C. Polonini, and E. C. F. Dijkers, “Postulated adjuvant therapeutic strategies for COVID-19,” J. Pers. Med. 2020. 10(3), pp. 1–33.
3. S. S. Abdelsalam, H. M. Korashy, A. Zeidan, and A. Agouni, “The role of protein tyrosine phosphatase (PTP)-1B in cardiovascular disease and its interplay with insulin resistance,” Biomolecules, 2019. 9(7), pp. 1–23.
4. M. Jagannathan-Bogdan, E. M. McDonnell, H. Shin, Q. Rehman, H. Hasturk, M. C. Apovian and S. B. Nikolajczyk ., “Elevated Proinflammatory Cytokine Production by a Skewed T Cell Compartment Requires Monocytes and Promotes Inflammation in Type 2 Diabetes,” J. Immunol., 2011. 186(2), pp. 1162–1172.
5. F. Rubino, A. S. Amiel, P. Zimmet, G. Alberti, S. Bornstein, H. R. Eckel, G. Mingrone, B. Boehm, E. M. Cooper, Z. Chai,. S. Del Prato, D. Hopkins, H. W. Herman, K. Khunti, C. Mbanya and E. Renard ., “New-Onset Diabetes in Covid-19,” N. Engl. J. Med., 2020; 383(8), pp. 789–790.
6. L. Zhu., G. Z. She, X. Cheng, J.J. Qin, J. X. Zhang, J. Cai, F. Lei, H. Wang, J. Xie, W. Wang, and H. Li, “Association of Blood Glucose Control and Outcomes in Patients with COVID-19 and Pre-existing Type 2 Diabetes,” Cell Metab., 2020. 31(6), pp. 1068-1077.e3.
7. K. Ramanathan, D. Antognini, A. Combes, M, Paden, B. Zakhary, M. Ogino, G. Maclaren and D. Brodie ., “Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study,” Endocrinology, 2020. 8(1), pp. 19–21.
8. L. Sylow, V. L. Tokarz, E. A. Richter, and A. Klip, “The many actions of insulin in skeletal muscle, the paramount tissue determining glycemia,” Cell Metab., 2021. 33(4), pp. 758–780.
9. B. Li, J. Yang, F. Zhao, L. Zhi, X. Wang, L. Liu, Z. Bi and Y. Zhao., “Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China,” Clin. Res. Cardiol., 2020. 109(5), pp. 531–538.
10. F. Zhou, T. Yu, R. Du, G. Fan, Y. Liu, Z. Liu, J. Xiang, Y. Wang, B. Song, X. Gu, L. Guan, Y. Wei, H. Li, X. Wu, J. Xu, S. Tu, Y. Zhang, H. Chen and B. Cao., “Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study,” Lancet, 2020. 395(10229), pp. 1054–1062.
11. A. Remuzzi and G. Remuzzi, “COVID-19 and Italy: what next?,” in The Lancet, vol. 395, no. 10231, Elsevier Ltd, 2020, pp. 1225–1228.
12. Z. Shahid, R. Kalayanamitra, B. McClafferty, D. Kepko,, D. Ramgobin,, S. C. Aggarwal, R. Chander, R. Vunnam, N. Sahu,, D. Bhatt and K. Jones ., “COVID-19 and Older Adults: What We Know,” J. Am. Geriatr. Soc., 2020. 68(5), pp. 926–929.
13. F. Wu, F. Wu, S. Zhao, B. Yu, M. Y. Chen, G. Z. Song, Y. Hu, W. Z. Tao, H. J. Tian, Y. Y. Pei, L. M. Yuan, L. Y. Zhang, H. F. Liu, Y. Liu, M. Q. Wang, J. J. Zheng, L. Xu, C. E. Holmes and Z. Y. Zhang., “A new coronavirus associated with human respiratory disease in China,” Nature, 2020. 579, no. 7798, pp. 265–269..
14. Najim, Y. S. .; Mohammed, T. T. .; Hussain, F. M. . The Impact Of Varying Azolla Dosages On Male Broilers Diets In Terms Of Economic Feasibility And Physiologic Performance. JLSAR 2022, 3, 42-45.
15. C. Chakraborty, A. R. Sharma, M. Bhattacharya, G. Sharma, G. Agoramoorthy, and S. S. Lee, “Diabetes and COVID-19: A major challenge in pandemic period?,” Eur. Rev. Med. Pharmacol. Sci., 2020. 24(21), pp. 11409–11420.
16. A. H. Pakpour, M. D. Griffiths, K.-C. Chang, Y.-P. Chen, Y.-J. Kuo, and C.-Y. Lin, “Assessing the fear of COVID-19 among different populations: A response to Ransing et al.” no. January, 2020..
17. M. Ajeel, A.; A. Mehdi, L. . Effect Of Eruca Sativa Seeds Powder As Feed Supplementation On Some Physiological Traits Of Male Lambs. Journal of Life Science and Applied Research. 2020, 1, 20-30..
18. Ali, A. F., Mohammed, Th. T. & Al-Bandar, L. K. Effect of adding different levels of Optifeed®, Vêo® Premium and Oleobiotec® to the diets as appetite stimulants in the production and physiological performance of Male broiler under heat stress conditions. Plant Archives, 2019;
Received: May 15 2023/ Accepted: June 10 2023 / Published:15 June 2023
Citation: Okab H F, Yassir H K, Majed M M. Estimation of Immunological and Physiological Parameters in Diabetic Patients with COVID-19. Revis Bionatura 2023;8 (2) 47. http://dx.doi.org/10.21931/RB/2023.08.02.47
