2022.07.02.51
Files > Volume 7 > Vol 7 No 2 2022
1College of Pharmacy/ Tikrit University, Tikrit, Iraq [email protected]
2 College of Medicine, Al-Nahrain University, Baghdad, Iraq
3Al-Yarmouk Teaching Hospital, Ministry of Health, Iraq [email protected]
4Al-Imamein Al-Kadhimein Medical City, Baghdad, Iraq [email protected]
*Corresponding author: Jabbar S. Hassan. [email protected]
Available from: http://dx.doi.org/10.21931/RB/2022.07.02.51
ABSTRACT
Covid 19 in hematological cancer patients can lead to a deterioration in the clinical course and a reduction in life expectancy leading high fatality rate. Vaccines developed against the causative virus may reduce the severity of the disease and a decline in mortality rate. This study aims to determine the impact of vaccination on the severity of COVID-19 illness in patients with hematologic malignancies. A multicenter retrospective observational study was conducted on 60 hospitalized patients admitted to intensive care units (ICUs). All patients were previously diagnosed with leukemia or lymphoma and tested positive for COVID-19 by real-time polymerase chain reaction (RT-PCR). Protocol version 8 was used to determine the patients' results, including improvement to discharge criteria or deterioration to death. The most results in this study; The mean age of the patients was 33.63± 16.5 years (range 6-72 years). Diabetes was the most common comorbid illness (10%). The Oxygen saturation range was (70-95%). Among (60) patients enrolled in this study;29(48.33%) was not received any Covid-19 vaccine while 31(51.67%) were fully vaccinated; concerning patients with positive COVID19; the underlying hematological malignancy was leukemia (63.3%) while patients with lymphoma were (36.7%); after 30-day follow up, depending to the outcome. The number of deaths was 14 cases (23.3%) of patients while the other 46 patients (74.7%) survived and were discharged from the hospital. Our study concludes that vaccinating hematological malignancy patients against Covid19 may provide clinical protection from this illness compared to no vaccination patients
Keywords. COVID-19 disease, Hematological Malignancy, Vaccine, intensive care units
INTRODUCTION
World Health Organization (WHO) in March 2020 stated that Coronavirus disease 19 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was a pandemic 1. Within a year, the mortality rate of this disease increased over the world; some groups of individuals are at high risk of developing severe and life-threatening infections. One of them is patients with hematological disorders due to immunocompromised status as chemotherapy treatments. Covid 19 disease in hematological cancer patients can lead to a deterioration of the clinical result and a reduction in life expectancy leading high fatality rate 2.
Patients with hematological malignancies deal more with the healthcare system, which puts them at a higher risk of contracting COVID-19. Furthermore, preliminary trials in China revealed that severe COVID-19 infection and death were common in all types of cancer patients compared to the general population 3.
Another study in this regard reported that patients suffering from blood malignancy are more susceptible to developing more severe infection and a high death rate of Covid-19 among all cancer patients. This could be because hematological malignancy patients frequently exhibit innate and adaptive immunological abnormalities, which is a critical risk factor for increased mortality in older age when it's associated with cancer disease 4.
After the scientist develops many types of Covid19 vaccines, professional oncology societies declare an urgent need for vaccination in patients with cancer, including hematological malignancies 5.
In people who have been vaccinated, the rate of hospital admissions and death from Covid 19 remained stable. According to Public Health England's latest surveillance report, unvaccinated people have a "significantly higher" risk than vaccinated people 6. Some studies reported that patients with immunocompromise might be less likely to produce a robust immune response to the vaccine, putting them at a higher risk of moderate to severe covid-19 7.
This study was conducted to determine the impact of vaccination on the severity of COVID-19 illness in Hematologic malignancy patients.
MATERIAL AND METHODS
A Multicenter retrospective observational study was conducted on 60 hospitalized patients who were admitted to intensive care units (ICUs). All patients were previously diagnosed with leukemia or lymphoma from January 2021 to the end of December 2021. All patients were tested positive for COVID-19 by real-time polymerase chain reaction (RT-PCR) assay, which was achieved in the hospital-based clinical laboratory.
All patients under investigation in this study were referred by consultation of a hematological specialist and verification of the information in the medical record. Patients with incomplete data, information or presented with non-malignant hematological diseases or solid cancer were excluded from this study.
Demographics, clinical and laboratory data were accumulated from a medical record for all participants; patients who are fully vaccinated have positive COVID-19 laboratory testing and symptoms that appear >14 days after the second dosage; while Individuals who have positive laboratory COVID-19 tests but no record of receiving any type of COVID-19 immunization or first-dose vaccination after symptom start are considered unvaccinated.
Outcomes
To observe the principles of early detection, reporting, quarantine and treatment of COVID-19 patients to increase recovery rates and lower fatality rates. Protocol version 8 was used to determine the patients' results, including improvement to discharge criteria or deterioration to death8. COVID-19 death was defined as the death of COVID19 patients who died as a direct result of coronavirus infection but not due to the pandemic's indirect effects 9.
Statistical Analysis
The quantitative data were expressed as mean ± standard deviation. Binomial data were presented as frequency percentages. Comparisons between quantitative were performed by the parametric Student t-test, while the Chi-square test made the comparison between binomial data. Multivariate analysis was performed with a binary logistic regression test. The odds ratio (OR) and its corresponding 9% confidence interval (CI) were calculated from this test. All data were analyzed with SPSS for Windows, v.25.0; IBM Corp, Armonk, USA.
RESULTS
Demographic Characteristics of the Patients
The mean age of the patients was 33.63± 16.5years (range 6-72 years); about two-thirds of them (60%) were females. Only a small percentage (15%) of the patients were ex/current smokers. Diabetes was the most common comorbid illness (10%). Many patients had more than one comorbidity (Table 1).
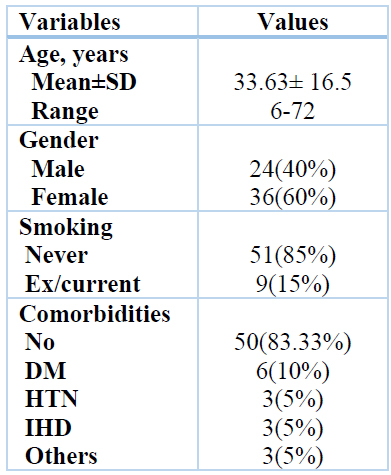
DM: diabetes mellitus, HTN: hypertension, IHD: ischemic heart disease. Other comorbidities include one case hyperthyroidism, heart failure and epilepsy.
Table 1. Patients' characteristics and demographic data (n=60)
Clinical Characteristics of the patients
During the sickness, all patients underwent respiratory support, and the oxygen saturation (SpO2) was measured using pulse oximetry; the saturation range (was 70-95%); among (60) patients enrolled in this study; 29 (48.33%) was not received any COVID-19 vaccine while 31 (51.67%) was fully vaccinated; Headache is the most prominent complaint in 39 (65%) of patients followed by cough in 38 (63.33%) in addition to that fatigue and loss of smell and taste was also reported as frequent symptoms and was 27 (45%) and 22 (36.67%) respectively. The other complaints include three cases of abdominal pain and two cases of vomiting and sore throat were much less frequent symptoms 7 (11.67%) table (2).
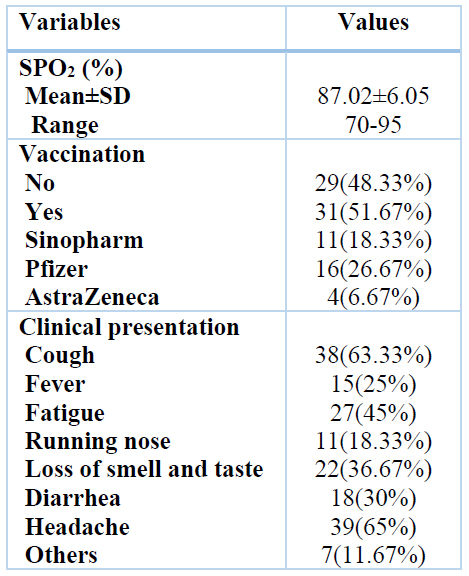
Table 2. Clinical presentation (n=60)
Type of Malignancies
Concerning patients positive for COVID-19, the underlying hematological malignancy was leukemia at 63.3%, while patients with lymphoma were 36.7%. After a 30-day follow-up, depending on the outcome, death was reported in 14 patients (23.3%), while the other 46 patients (74.7%) survived and were discharged from the hospital figure (1) and (2).
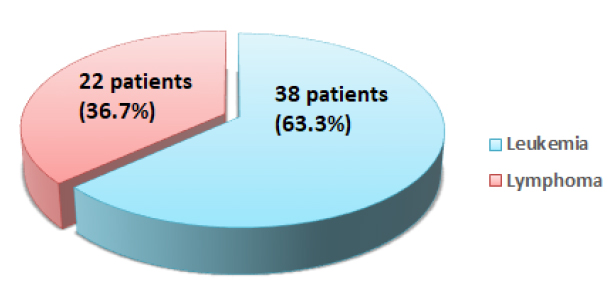
Figure 1. The proportion of leukemia and lymphoma in patients with COVID1-9
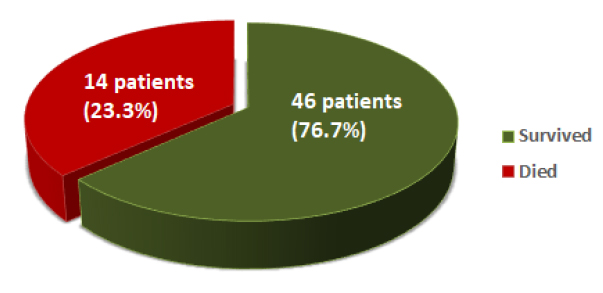
Figure 2. Mortality and Survived Percentage
Association of Clinical Characteristics with a Survival rate
Patients were classified into two groups according to outcomes (survival and dead patients); patients in the survived group reported SPO2% (88.9±4.1%) compared to (81.79±7.56) in dead patients with significance differences (P-value <0.001). Many patients in the survived group underwent fully COVID 19 vaccination 31 (67.39%). On the other hand, no patients in the dead group received such vaccines with a significant difference (P-value <0.001). Among clinical symptoms, non -significant differences were obtained between the two groups. Concerning the type of hematological malignancies, the leukemic patients were more common among survival (33 patients, 71.74%) than deceased patients (5 patients, 35.71%) with a significant difference (Table 3).
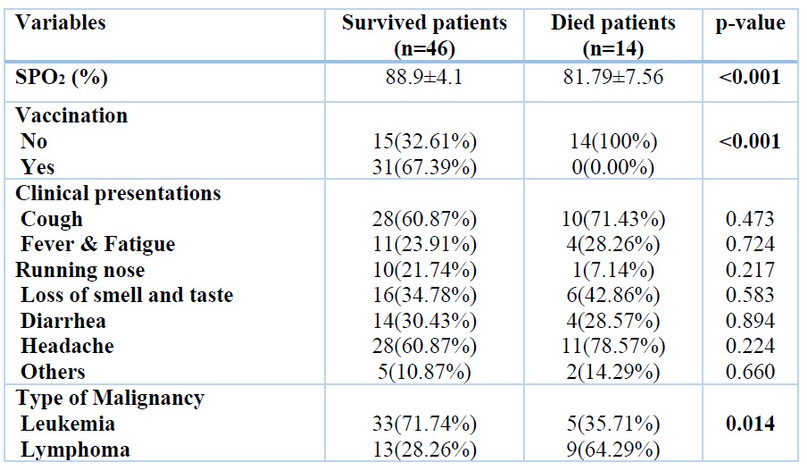
Table 3. Association of clinical characteristics with outcomes
Multivariate Analysis
All variables that demonstrated significant association with the patient's outcome in univariate analyses were entered into multivariate analysis. The results are shown in Table 4. Two variables remained significantly associated with the patients' outcomes. More than half of deceased patients (57.14%) had SPO2 <85% compared with 23.91% of surviving patients who had such percent with a significant difference (OR= 2.62, 95% CI 1.21-3.48 P=0.042). Furthermore, 76.39% of surviving patients were vaccinated versus none of the deceased patients who had a vaccine, with a highly significant difference (OR=15.6, 95% CI 1.75-18.17, P=0.003).
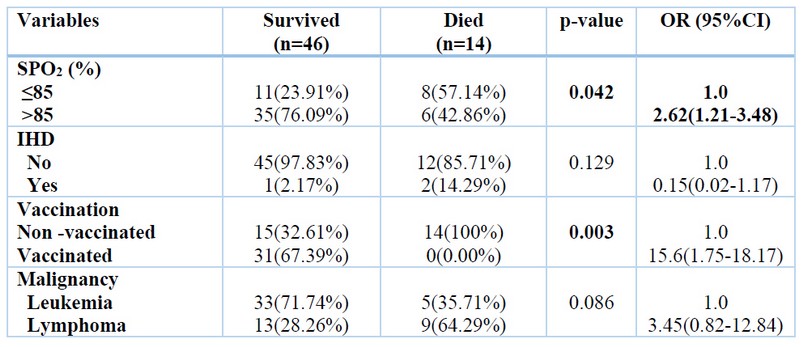
Table 4. Multivariate Analysis
DISCUSSION
The rapid spread of SARS-CoV-2 worldwide has created a unique medical situation for individuals with chronic diseases, including patients with hematological malignancies who are at the most significant risk of severe COVID-19. As a result, incremental vaccines have been a top goal; and highly protective vaccinations are already being distributed. The current study looked at the crucial role of COVID-19 vaccination in the survival of patients with hematological malignancies who were admitted to the hospital.
Among sixty patients with hematological malignancy confirmed to COVID-19 infection in this study, the mean age of the patients suffering from this infection was 33.63± 16.5 with a range of 6-72 years. However, this observation disagreed with many studies that reported severe cases of COVID-19 were more common in older patients 65 years old 10,11.
The difference in this study from other studies can be attributed to the fact that the selection of patients in this study is restricted to people who suffer from hematological diseases, and it is known that blood malignancy affects different ages.
In the current study,60% of patients were female, and (40%) of them were male and male to female (1:1.5). Much literature on gender as a risk of in-hospital mortality provides mixed results. According to a few studies, sex differences may exist in COVID-19 individuals with severe illnesses, with men being more likely than women and recovery is more challenging 12,13.
This result is incompatible with those obtained in the above studies. However, many researchers in Middle Eastern countries, including Iraq, mentioned that hematological cancer affects females more than males 14,15.
The majority of patients in the current study (85%) were nonsmokers, and it was higher than the results obtained by Prats-Uribe et al., Who mentioned that (56.2%) of COVID-19 patients were nonsmoker16; Conversely, it was less than the results reported by Heydari et al. (77.8%) 17.
The explanation for these variations in smokers and nonsmoker COVID-19 patients could be attributed to differences in the socioeconomic and geographical aspects of the studied locations and differences in the study methods. The size of the sample and the distinction in the mode of life factors.
The data reported that most patients had no comorbidities (83.33%) while (16.67%) of the patients had comorbid diseases. Furthermore, diabetes mellitus is the most frequent comorbidity in the current study but less than the finding of other studies conducted in Myanmar 37.8% 18. Singapore 28.3% 19. But it's higher than the finding reported in China, 15.8% 20. This disparity in such results could be explained by differences in the prevalence of chronic diseases by age, gender, and geographic region.
In the current study, headache (65%) and cough (63.33%) are the predominant clinical impression associated with COVID 19 infection, followed by fatigue (45%) then smell and taste (36.67%); this result is inconsistent with prior studies stated that fatigue, sore throat, shortness of breath and rhinorrhea were the most common presenting symptoms of COVID 19 patients 21,22.
In this study, patients were classified into two groups according to outcomes (survival and dead patients); overall results in the current study showed a considerable decline in Oxygen saturation SPO2% in Died (81.79%). Such results are in line with other studies that stated decreasing in SPO2% is closely related to an increased mortality rate in COVID19 patients in which pulmonary infection may affect the oxygenation state, resulting in a decrease in peripheral SpO2, which subsequently leads to acute respiratory distress syndrome (ARDS) and acute hypoxemic respiratory failure 23,24.
In the current study, out of 14 deceased patients, 2 (14.29%) were presented with IHD. Such a finding is lower than the result by Shi et al. 25. Who reported that 19.7% of COVID 19 patients displayed heart disease. In another study conducted in China, the authors displayed that the SARS-CoV-2 infection has a more significant clinical impact in people who have had previous cardiovascular illness 26.
This study reported a higher mortality rate in non-vaccinated patients than surviving. Many studies mentioned that vaccination against COVID-19 is a cornerstone for reversing the COVID-19 pandemic; all vaccines have reduced disease severity and mortality, particularly in immunocompromised individuals 27.
Our data confirm that a more significant number of COVID-19 cases were diagnosed with leukemia 63.3%; most of the patients recorded 33 (71.74%) in a survived group with leukemia, however; 13 (28.26%) of the survived patients presented with lymphoma comparatives for 9 (64.29%) in the dead group. This result contradicts the finding of Xuejun et al., Who found that most patients with COVID-19 had lymphoid malignancies 28. This discrepancy may be due to our regional patient population distribution, which has higher rates of leukemia malignancies. Pagano et al. mentioned that a clear correlation between the type of hematological malignancy and the incidence of COVID-19 had not been described in the literature 29.
Furthermore, COVID-19 and Cancer Consortium (CCC19), the UK Coronavirus Cancer Monitoring Project (UKCCMP), and the American Society of Hematology (ASH) Research Collaborative are all larger cohort and registry studies that will give insight to the present questions about hematological malignancies and COVID-19. However, it is evident that patients with such malignancies are a susceptible group, and further research is needed to comprehend COVID-19's influence on these individuals 30 fully.
CONCLUSION
The current study results suggest that; vaccinating hematological malignancy patients against COVID19 may provide clinical protection from this illness compared to no vaccination, patients which supports national and international public health policy suggestions for the targeting of immunocompromised patients for such vaccination.
Author Contributions
(1) Design and acquisition of data.
(2) Writing the article and revising it critically for important intellectual content analysis and interpretation of results.
(3) & (4): Samples collection from patients and Statistical analysis.
Funding: Self-funding
Institutional Review Board Statement: The ethical aspects of this study have been approved by the ethical council in Medical College, Al- Nahrain University.
Informed Consent Statement: "Informed consent was obtained from all patients involved in this study."
Conflict of interest: The author declares that they have no competing interests.
Acknowledgment: The authors highly appreciate the effort of all staff in Al-Imammian Al-Kadhimein Medical City and the COVID-19 quarantine center in Baghdad during sample collection.
REFERENCES
1- Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Bio Medica: Atenei Parmensis. 2020;91(1):157.
2- Vijenthira A, Gong IY, Fox TA, Booth S, Cook G, Fattizzo B, Martín-Moro F, Razanamahery J, Riches JC, Zwicker J, Patell R. Outcomes of patients with hematologic malignancies and COVID-19: a systematic review and meta-analysis of 3377 patients. Blood. 2020 Dec 17;136(25):2881-92.
3- Liang W, Guan W, Chen R, Wang W, Li J, Xu K, Li C, Ai Q, Lu W, Liang H, Li S. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. The lancet oncology. 2020 Mar 1;21(3):335-7).
4- Dai M, Liu D, Liu M, Zhou F, Li G, Chen Z, et al. Patients with Cancer Appear More Vulnerable to SARS-COV-2: A Multicenter Study During the COVID-19 Outbreak. Cancer Discovery (2020) 10:CD–20-0422. doi: 10.1158/2159-8290.CD-20-0422
5- Ribas A, Sengupta R, Locke T, Zaidi SK, Campbell KM, Carethers JM, Jaffee EM, Wherry EJ, Soria JC, D'Souza G. Priority COVID-19 vaccination for patients with cancer while vaccine supply is limited. Cancer discovery. 2021 Feb 1;11(2):233-6.
6- Iacobucci G. Covid-19: Act now or hospital admissions could soar, experts tell government. BMJ: British Medical Journal (Online). 2021 Sep 16;374.
7- Egan C, Thorpe M, Knight S. Hospital admission for covid-19 and impact of vaccination: analysis of linked data from the National Immunisation Management Service (NIMS) and the Coronavirus Clinical Information Network (CO-CIN).
8- Commission NH. Diagnosis and treatment protocol for novel coronavirus pneumonia (Trial version 8). Chin Med J. 2020. https://doi.org/10.1097/ CM9.0000000000000819)
9- Meo SA, Abukhalaf AA, Alomar AA, AlMutairi FJ, Usmani AM, Klonof DC. Impact of lockdown on COVID-19 prevalence and mortality during 2020 pandemic: observational analysis of 27 countries. Eur J Med Res. 2020;25(1):1–7
10- Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The lancet. 2020 Mar 28;395(10229):1054-62
11- Alamdari NM, Afaghi S, Rahimi FS, Tarki FE, Tavana S, Zali A, Fathi M, Besharat S, Bagheri L, Pourmotahari F, Irvani SS. Mortality risk factors among hospitalized COVID-19 patients in a major referral center in Iran. The Tohoku journal of experimental medicine. 2020;252(1):73-84.
12- United Kingdom. Intensive Care National Audit & Research Centre. Available online: https://www.icnarc.org (accessed on 15 January 2021)
13- Meng, Y.; Wu, P.; Lu, W.; Liu, K.; Ma, K.; Huang, L.; Cai, J.; Zhang, H.; Qin, Y.; Sun, H.; et al. Sex-specific clinical characteristics and prognosis of coronavirus disease-19 infection in Wuhan, China: A retrospective study of 168 severe patients. PLoS Pathog. 2020, 16, e1008520. [CrossRef]
14- Al-Janabi AA, Naseer ZH, Hamody TA. Epidemiological study of cancers in Iraq-Karbala from 2008 to 2015. International Journal of Medical Research & Health Sciences. 2017;6(1):79-86.
15- Kulhánová I, Bray F, Fadhil I, Al-Zahrani AS, El-Basmy A, Anwar WA, Al-Omari A, Shamseddine A, Znaor A, Soerjomataram I. Profile of cancer in the Eastern Mediterranean region: The need for action. Cancer epidemiology. 2017 Apr 1; 47:125-32.
16- Prats-Uribe A, Xie J, Prieto-Alhambra D, Petersen I. Smoking and COVID-19 Infection and Related Mortality: A Prospective Cohort Analysis of UK Biobank Data. Clinical Epidemiology. 2021; 13:357.
17- Heydari G, Arfaeinia H. COVID-19 and smoking: More severity and death–An experience from Iran. Lung India: Official Organ of Indian Chest Society. 2021 Mar;38(Suppl 1):S27.
18- Htun, Y.M., Win, T.T., Aung, A. et al. Initial presenting symptoms, comorbidities and severity of COVID-19 patients during the second wave of epidemic in Myanmar. Trop Med Health 49, 62 (2021). https://doi.org/10.1186/s41182-021-00353-9
19- Puah SH, Young BE, Chia PY, Ho VK, Loh J, Gokhale RS, Tan SY, Sewa DW, Kalimuddin S, Tan CK, Pada SK. Clinical features and predictors of severity in COVID-19 patients with critical illness in Singapore. Scientific reports. 2021 Apr 5;11(1):1-1.
20- Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DS, Clinical characteristics of coronavirus disease 2019 in China. New England journal of medicine. 2020 Apr 30;382(18):1708-20.
21- Pongpirul WA, Wiboonchutikul S, Charoenpong L, Panitantum N, Vachiraphan A, Uttayamakul S, Clinical course and potential predictive factors for pneumonia of adult patients with Coronavirus Disease 2019 (COVID-19): A retrospective observational analysis of 193 confirmed cases in Thailand. PLoS neglected tropical diseases. 2020 Oct 16;14(10):e0008806.
22- Vaughan L, Veruttipong D, Shaw JG, Levy N, Edwards L, Winget M. Relationship of socio-demographics, comorbidities, symptoms and healthcare access with early COVID-19 presentation and disease severity. BMC Infectious Diseases. 2021 Dec;21(1):1-0.
23- Shenoy N, Luchtel R, Gulani P. Considerations for target oxygen saturation in COVID-19 patients: are we under-shooting? BMC medicine. 2020 Dec;18(1):1-6.
24- Lu X, Jiang L, Chen T, Wang Y, Zhang B, Hong Y, Wang J, Yan F. Continuously available ratio of SpO 2/FiO 2 serves as a noninvasive prognostic marker for intensive care patients with COVID-19. Respiratory Research. 2020 Dec;21(1):1-4.
25- Shi, S.; Qin, M.; Shen, B.; Cai, Y.; Liu, T.; Yang, F.; Gong,W.; Liu, X.; Liang, J.; Zhao, Q.; et al. Association of Cardiac Injury with Mortality in Hospitalized Patients With COVID-19 in Wuhan, China. JAMA Cardiol. 2020, 5, 802–810. [CrossRef] [PubMed]
26- Team E. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China, 2020. China CDC weekly. 2020 Feb 21;2(8):113.
27- Egan C, Thorpe M, Knight S. Hospital admission for covid-19 and impact of vaccination: analysis of linked data from the National Immunisation Management Service (NIMS) and the Coronavirus Clinical Information Network (CO-CIN).
28- Xuejun Alice Wang, Adam F. Binder, Usama Gergis and Lindsay Wilde: COVID-19 in Patients with Hematologic Malignancies: A Single Center Retrospective Study Front. Oncol. doi: 10.3389/fonc.2021.740320
29- Pagano L, Salmanton-García J, Marchesi F, Corradini P, Hoenigl M, Klimko N, Koehler P, Pagliuca A, Passamonti F, Verga L, Víšek B. COVID-19 infection in adult patients with hematological malignancies: a European Hematology Association Survey (EPICOVIDEHA). Journal of hematology & oncology. 2021 Dec;14(1):1-5.
30- Desai A, Mohammed TJ, Duma N, et al. COVID-19 and Cancer: A Review of the Registry-Based Pandemic Response. JAMA Oncol. 2021;7(12):1882–1890. doi:10.1001/jamaoncol.2021.4083
Received: 30 January 2022 / Accepted: 9 March 2022 / Published:15 May 2022
Citation. Saleh KS, Hassan J S, Zaidan A, Abdul- Ridha R A. The Impact of Vaccination on Severity of COVID-19 Illness in Hematologic Malignancies Patients. Revis Bionatura 2022;7(2) 51. http://dx.doi.org/10.21931/RB/2022.07.02.51
