2023.08.03.52
Files > Volume 8 > Vol 8 No 3 2023
Diagnostic utility of high-sensitive troponin T in patients with acute coronary syndrome
Osvaldo Valdés Dupeyrón1  , Maribel Quintero Arcentales1
, Maribel Quintero Arcentales1 , Lidia Espinales-Casanova2
, Lidia Espinales-Casanova2 , Caleb I. Chilán Santana2
, Caleb I. Chilán Santana2 , Ivon Howland Alvarez2
, Ivon Howland Alvarez2 , Alejandro Villar Inclan3
, Alejandro Villar Inclan3 , Javier González Robles2
, Javier González Robles2 , Natacha Lois Mendoza2
, Natacha Lois Mendoza2 , Juan Carlos Suarez Fernández2
, Juan Carlos Suarez Fernández2 , Andrea Patricia Chancay Mendoza2
, Andrea Patricia Chancay Mendoza2 , Jhon Henry Calle Poveda2
, Jhon Henry Calle Poveda2 , Grover Michael Manrique Choez2
, Grover Michael Manrique Choez2 , Walther Zhukov Paz y Miño Intriago1
, Walther Zhukov Paz y Miño Intriago1 , José Miguel Rubio Cala4
, José Miguel Rubio Cala4 , Lorena Garcia Lois2
, Lorena Garcia Lois2 , Rider Quintana Souza5
, Rider Quintana Souza5 , Yarisley Barrueto Blanco5
, Yarisley Barrueto Blanco5
1 Department of Surgery, Verdi Cevallos General Hospital, Portoviejo, Manabí, Ecuador
2 Graduate Department and health science. Technical University of Manabí, Ecuador.
3 Department of cardiovascular Surgery Hospicor. Manta. Manabí. Ecuador
4 Ásmerp, Metrodial Portoviejo, Portoviejo, Manabí, Ecuador.
5 Department of Surgery, Hospital Rodriguez Zambrano, Manta, Manabí, Ecuador
* Correspondence: Osvaldo Valdés Dupeyrón, Email: osvaldovaldesdupeyron @gmail.com
Available from: http://dx.doi.org/10.21931/RB/2023.08.03.52
ABSTRACT
Cardiovascular diseases are the first cause of death in the world. Early detection of coronary pathologies contributes to the prevention of acute coronary events. High-sensitive troponin T is a valuable biomarker for diagnosing and assessing these patients. A retrospective cross-sectional study was performed from January 2018 to December 2020 at Hospicor-Manta. We included 571 patients who attended the Intensive Care Unit and had at least one high-sensitive troponin T determination with symptoms in the first 6 hours. Analyzing from the upper reference limit (99th percentile, allows understanding and interpreting data from the values below which a certain percentage is found for cardiac troponins. Elderly male patients tended to suffer acute coronary syndrome (p<0.05). The most frequent comorbidities were: arterial hypertension, dyslipidemia and diabetes (p< 0.05). There was evidence of the correlation between high-sensitive troponin T values and electrocardiographic signs of acute coronary syndrome (p<0.05). There was a moderate correlation between high-sensitive troponin T analysis and acute coronary syndrome (p< 0.05).
Keywords: Cardiovascular diseases, acute coronary syndrome, high-sensitive troponin T.
INTRODUCTION
Cardiovascular diseases (CVD) are the leading cause of death worldwide and in most Latin American countries. CVDs are estimated to cause 1.9 million deaths per year. 1 However, many of these diseases can be prevented by using healthy diets, regular physical exercise, and avoiding tobacco use, among other measures.
Myocardial infarction and cerebrovascular disease are part of the so-called non-communicable diseases. Around 4.45 million people die each year from these entities, and a third of these deaths occur before the age of 70. 2
Early detection of coronary disease in the subclinical stage through laboratory analysis helps prevent acute coronary events such as unstable angina (UA), acute myocardial infarction (AMI), and death of coronary origin.3,4
Troponin I and troponin T (TnI and TnT) are muscle-thin filament proteins that are part of a complex in skeletal muscle. Both TnI and TnT exist in skeletal and cardiac forms. Cardiac isoforms are extremely heart-specific and are increasingly used as specific markers of myocardial damage. The more injury to the heart, the higher the blood troponin value will be.5
Ultrasensitive cardiac troponin (hs-cTn) assays are superior to conventional cardiac troponin (cTn) studies for the early diagnosis of AMI. Current guidelines recommend using cut-off values for cTn corresponding to the 99th percentile in healthy controls and a rising and falling pattern. Hs-CTn should be measured on admission and repeated 3–6 hours later because some chronic diseases show high but stable cTn concentrations; dynamic changes become a critical part of diagnosing AMI. However, it is essential to distinguish the differences associated with AMI from the dynamic changes associated with laboratory imprecision or normal chronobiological variation.6
Acute coronary syndromes (ACS) include a broad spectrum of clinical presentations, ranging from chest pain to cardiogenic shock due to prolonged ischemia or mechanical complications. They also encompass electrocardiographic presentations such as ST-segment elevation myocardial infarction (STEMI) or non-ST-segment elevation ACS (NSTE-ACS).7
Regardless of the presence of typical signs and symptoms of myocardial ischemia and suggestive electrocardiographic (ECG) abnormalities, measurement of cTn, either cTnI or cTnT, has become the gold standard to make a specific clinical decision, particularly for the diagnosis of NSTEMI.8,9
In Ecuador, data from the National Institute of Statistics and Censuses (NISC) of 2018 indicated that ischemic heart disease is the leading cause of death in the general population, with more than 3,000 deaths per year, both in men and women. The incidence of STEMI despite new ischemic event detection technologies is increasing.10
Cardiovascular pathologies generate a significant clinical, social, and economic impact in industrialized and developing countries. In our health center, the number of patients with ACS has been increasing in recent years; for this reason, we have proposed to determine the usefulness of high-sensitive troponin T (hs-TnT) in the diagnosis of acute coronary syndrome in patients treated during 2018-2020 in Hospicor -Manta.
MATERIALS AND METHODS
A retrospective cross-sectional study was conducted to determine the importance of hs-TnT in diagnosing patients with acute coronary syndrome from January 2018 to December 2020 at Hospicor-Manta. We included 1438 patients who met the following criteria: admitted to the Hospicor-Manta Intensive Care Unit and with at least one hs-TnT determination within 4 to 6 hours of symptom onset or admission. Sociodemographic variables were analyzed: age, sex, and cardiovascular risk factors: hypertension, dyslipidemia, smoking, diabetes mellitus, and obesity. All patients underwent an initial clinical evaluation, where clinical data, 12-lead electrocardiogram, electrocardiographic monitoring, hs-TnT levels between 4 to 6 hours, and a second measurement within the first 24 hours were recorded. All information was stored in an EXCEL database. Samples in hs-TnT analysis were obtained basally at 4-6 hours from the onset of pain or admission and within 24 hours with a total of (N=189) for 2018, (N=216) for 2019, and (N=166) for 2020, giving a total of 571 cases to be studied, analyzing from the upper reference limit (99th percentile, which allowed understanding and interpretation of data, from the values below which a certain percentage is found). Qualitative variables were expressed as percentages and analyzed using the chi-square test. Quantitative variables were defined as means with their standard deviation, diagnosed with the T-test or non-parametric as appropriate, and by paired sample analysis, where age was analyzed using a numerical interval scale in which both the order and the exact differences between the values were represented, calculating a range of 10 years to determine the predisposing values in terms of the 99th percentile, which divides a series of data ordered from lowest to highest in one hundred equal parts.
Hs-TnT levels were measured using the Wilcoxon test (Mann-Whitney) for comparison between two subgroups, such as those with ACS and those without ACS without ST-segment elevation. In the analysis of comorbidities, 571 patients were taken, with a standard deviation that analyzed the information on the mean dispersion to the variable ACS. In addition, the confidence interval was determined, which indicated that within the given range, the true value of a parameter with 99% certainty was found as recommended cut-off values for the diagnosis of ACS are the upper reference limit (ULR); that is, the 99th percentile, the same that is important to determine the relationship that may exist between the causes that predispose to the increase in ACS. Hs-TnT utilization strategies were evaluated and obtained by a COR curve for hs-TnT. Differences with a probability error of less than 5% were considered significant, where sensitivity, specificity, positive predictive value, and negative value about hs-TnT were recognized. The data were analyzed using SPSS 18.0 software from the documentary collection of patients in the study years.
RESULTS
A population of 571 patients with elevated hs-TnT levels attended the Hospicor-Manta Intensive Care Unit from 2018 to 2020 was considered.
Table 1 analyzed age using a numerical scale and hs-TnT levels, using the Wilcoxon test (Mann-Whitney) for comparison between two subgroups: determination of patients with ACS and without ACS without ST-segment elevation, said probability values less than 0.05 (p<0.05).
There was a prevalence of male sex represented by hs-TnT levels with a p99 value of 71.5 with 11.1-194.3, and with ACS of 38.4%, giving a p-value of 0.03, indicating that the result is clinically essential.
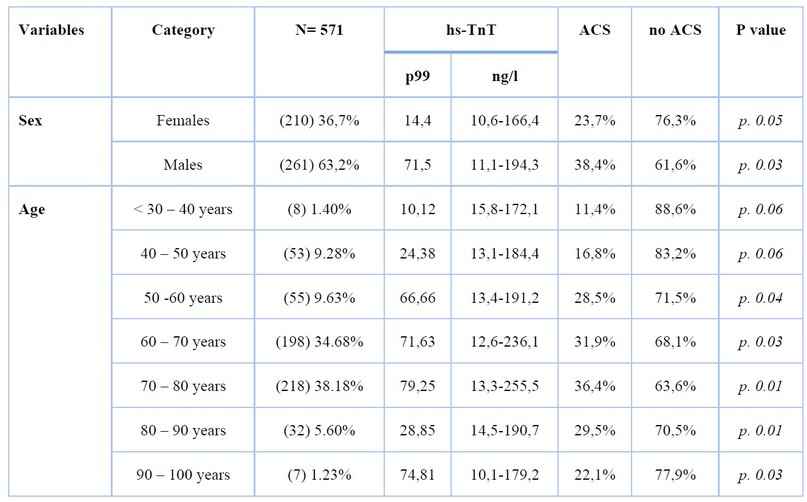
Table 1. Sociodemographic factors related to high-sensitive troponin T - Acute coronary syndrome
Analyzing the age ranges, it can be established that high hs-TnT levels are more prevalent in patients aged 60 to 70 years with hs-TnT values of 12.6-236.1 ng/l and 31.9% of cases with ACS (p. 0.03). Age groups between 70 to 80 years presented hs-TnT levels of 13.3-255.5 ng/l with a total of 36.4% of patients with ACS. Likewise, patients aged 80 to 90 years showed hs-TnT levels of 14.5-190.7 ng/l, with 29.5% of patients with ACS determined with a p-value of 0.01, resulting in clinically significant.
Table 2 shows that diabetes accounted for 64.6% (369) with a confidence interval of 12,184-15,823 calculated using the 99th percentile, with a p-value of 0.03, followed by arterial hypertension with 59.6% (340) with a CI of 12,242-14,043 and a p-value of 0.02. These results corroborate that the presence of associated diseases constitutes a considerable risk factor in the appearance of ACS, with the consequent elevation of troponins.
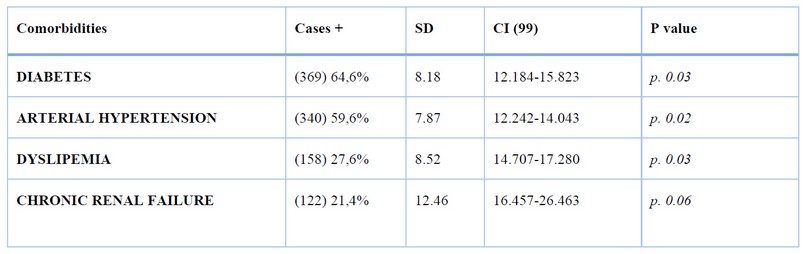
Table 2. Causative factors/comorbidity
Figure 1 shows the association between the levels of involvement of the pathologies represented on ACS using a ROC curve. The sensitivity of 99L was calculated at 64.6% (CI 12.184-26.463) as the cut-off point for the diabetes result. The specificity was 21.4% (CI 16.457-26.463) based on minimum values for the chronic renal failure cut-off point, between which the cut-off points for arterial hypertension and dyslipidemia were established.
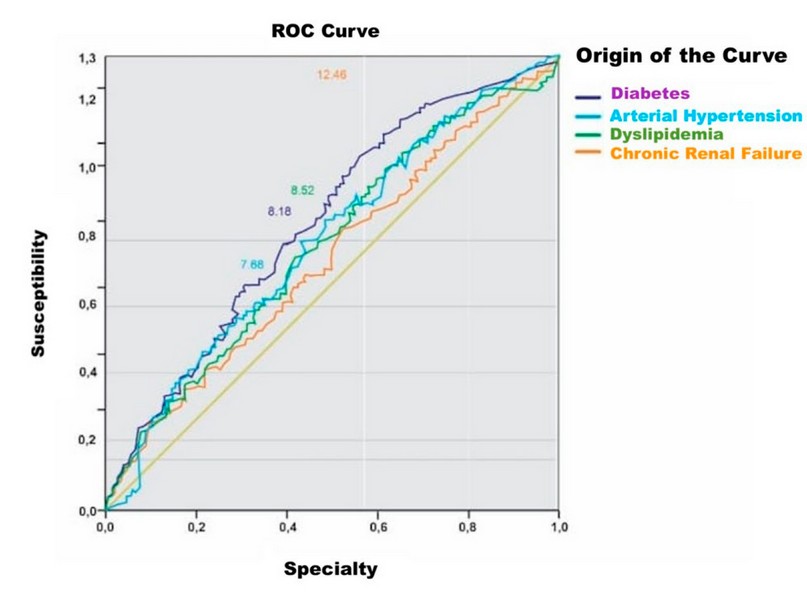
Figure 1. Association between levels of involvement of comorbidities represented on ACS
The groups with risk factors analyzed through the Wilcoxon test showed highly statistically significant differences (p<0.003). This expressed that the hs-TnT values of each group with risk factors were significantly higher for the diagnosis of acute coronary syndrome. In addition, it can be observed that diabetes mellitus, arterial hypertension, and dyslipidemia have the highest incidence according to the susceptibility analyzed within the graph.
Table 3 showed hs-TnT values >0.004ng/ml in 78.3% of patients with electrocardiographic signs of ACS, while cases with hs-TnT concentration <0.004ng/ml represented 21.7% with ACS. The percentage of electrocardiogram results can determine the total f / % value. This does not predict a stable analysis because troponin levels can be unstable when the ACS determination is performed in the first hours of symptom onset. However, a p-value of 0.05 is presented for tests with Tntus >0.004ng/ml. This means that hs-TnT values can detect ACS at an earlier stage than traditional tests, which may lead to early treatment. It is important to note that ultrasensitive troponins should be complemented with the clinical picture and other studies to confirm the diagnosis of ACS.
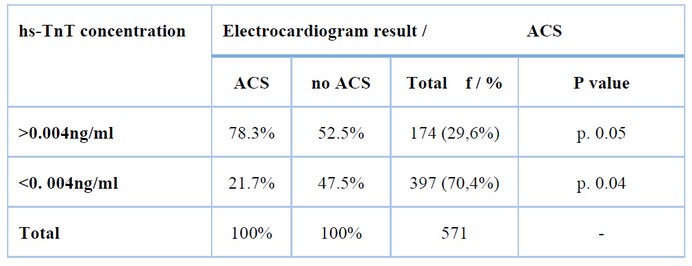
Table 3. Electrocardiogram result according to his-TnT / ACS concentration
Table 4 shows correlational variables according to Pearson's R that allow us to analyze the incidence of the hs-TnT study on the determination of patients with ACS. A moderate correlation was demonstrated, being moderately significant when knowing that using the hs-TnT analysis, it is possible to establish the existence of ACS, applying the mean analyses that predispose sociodemographic values causative around comorbidities. This result allows instituting an upper limit of 0.595 for his-TnT, within a TnTus value of 50 ng/L, which is an adequate cut-off point to evidence coronary problems, where 0.489 is estimated as a confidence interval to determine the existence of the
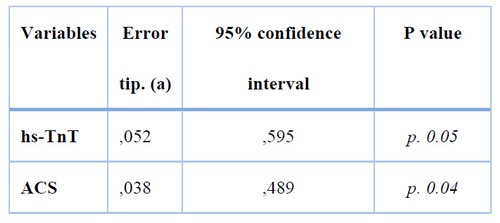
Table 4. Correlation of variables hs-TnT / ACS
The correlation between ultrasensitive troponin levels and ACS is strong, with higher troponin levels indicating a higher probability of ACS by presenting a p.value of 0.05, focusing on a moderate correlation; however, it is essential to keep in mind that a positive troponin test alone does not confirm the diagnosis of ACS.
DISCUSSION
In the analysis of the sociodemographic characterization of patients with acute coronary syndrome and hs-TnT elevation, there was a predominance of males in our study and most of the series reviewed.11-18 However, Dominguez et al. 19 found a slight difference in favor of females, despite including patients with non-ischemic troponin elevation, without taking into account the clinical signs of ACS and only using hs-TnT values as a predictor of mortality. Regarding age, there was a similarity between the present study and the literature consulted, where there was a proportional increase between years of life and troponin elevation in coronary pathologies. 11-19
Comorbidities increase the probability of suffering or dying from cardiovascular disease in those who present them. Since the beginning of the present century, major independent risk factors have been incorporated, which have a stronger association with CVD and are very frequent in the population. Let us take into account the most frequent comorbidities in our patients. We can observe that they are all included in this group, which makes this population more vulnerable to ACS and elevated hs-TnT.20
Diabetes is an independent risk factor for coronary atherosclerosis. There is a relationship between hyperglycemia and ACS prognosis, with increased glycemia being a strong predictor of adverse events in patients admitted for ACS. 21,22
Liu et al. studied 498 patients with non-ST-segment elevation ACS divided into three groups according to glycemia values at admission: group A: glycemia less than 7.8 mmol/L, group B: glycemia between 7.8 and 11.0 mmol/L and group C glycemia ≥ 11.1 mmol/L; they found higher rates of heart failure, malignant arrhythmias and death in groups B and C compared to group A with statistically significant results (p<0.05). This relationship was similar when group B was compared with group C, with a higher incidence of the effects above in group C (p<0.05).23
Other series corroborate the relationship between associated diseases and ACS; the study by Sprocket and Diaztagle evidenced a high incidence of hypertensive and previously cardiac patients with recurrent angina and infarction.24 Likewise, a recent study published in the Malaysian Journal of Medical Sciences found elevated troponin levels in hypertensives and diabetics who suffered coronary syndromes.25
Modifications of troponin values have also been demonstrated in patients with CKD on dialysis. 26-28 However, a study published by Baron et al. observed troponin elevation in only 3% and 6% during pre-dialysis and post-dialysis, respectively, which demonstrated a low incidence of abnormal troponins in patients with CKD on dialysis, with non-significant differences. 29 Similarly, a study published in the Spanish Journal of Cardiology found a low incidence of abnormal troponins in patients with CKD. These results demonstrate the importance of interpreting troponin elevation as a risk condition without considering its increase due to its causative disease. 14
cTn has been used for years as the primary study in diagnosing coronary syndromes. With the incorporation of highly sensitive biomarkers, our interpretation of the results has changed considerably. These ultrasensitive tests allow early detection of infarcts, even identifying microinfarcts within the first 2 hours of symptom onset. 30 In the Fourth Universal Definition of Myocardial Infarction, high-sensitivity troponin measurements are recommended over less sensitive ones since they provide greater diagnostic accuracy at an identical low cost. 31
A study published in the Spanish Journal of Cardiology demonstrated cardiac injury by high-sensitivity troponin values in 34.6% of patients with severe COVID-19. Mortality and mechanical ventilation were higher in patients with cardiac injury than in patients without cardiac injury (39.1% vs. 9.1%).32
Similar results were described by an article in the New England Journal of Medicine, where TnTus tests were positive in 114 patients, considering an accurate early detection of myocardial cell injury in ACS; furthermore, negative test results were associated with low risk and allowed the rapid and safe discharge of patients with an episode of acute chest pain from the emergency room.33 However, in the study by Jaffe et al., it was shown that most current immunoassays for measuring hs-TnT lacked the recommended analytical sensitivity to determine the ULR accurately; that is, the 99th percentile reference value, which is the cut-off value recommended by existing guidelines for diagnosing ACS.34
A multicenter study involving several hospitals in Australia and New Zealand with a population of 4371 patients with suspected ACS found no differences between groups in angiography or revascularization rates. All analyses showed a low incidence of in-hospital events, including recurrent heart failure in patients for whom high-sensitivity troponins were used (GEE odds ratio, 0.75; 95 % CI, 0.60-0.94; P = 0.014); IPW analysis showed an absolute reduction of 2.3 % in these events with the use of the high-sensitivity assay (P = 0.018).35
A similar result was shown in a study published in the Argentine Journal of Cardiology, where it was concluded that clinical variables and ultrasensitive troponin values were not consistent in predicting hospital events in patients with ACS. In addition, they considered it unnecessary to use them to guide therapeutic strategies. 13
In the present study, a moderate correlation was observed, being moderately significant when knowing that utilizing the analysis of hs-TnT value, it is possible to see the existence of ACS, applying the mean analyses that predispose sociodemographic values, causative around comorbidities managing to establish an upper limit of 0.595 for hs-TnT, within a hs-TnT value of 50 ng/L seems to be an adequate cut-off point that predisposes to evidence coronary problems.
CONCLUSIONS
There was a predominance of male patients aged 70-80; the most frequent comorbidities were hypertension and diabetes. There was a statistically significant correlation between ultrasensitive troponin levels and electrocardiographic findings of ACS. A moderate correlation was significant when we found that the analysis of hs-TnT predisposes to ACS despite the levels of hs-TnT instability according to the cut-off point.
Author Contributions: Conceptualization, Osvaldo Valdés Dupeyrón. and Maribel M. Quintero Arcéntales; methodology, Lidia Espinales-Casanova.; software, Caleb I. Chilán Santana.; validation, Osvaldo Valdés Dupeyrón, Maribel M. Quintero Arcéntales. and Lidia Espinales-Casanova.; formal analysis, Ivon Howland Alvarez.; investigation, Alejandro Villar Inclan.; resources, Javier González Robles and Yarisley Barrueto Blanco; data curation, Natacha Lois Mendoza.; writing—original draft preparation, Juan Carlos Suarez Fernández.; writing—review and editing, Andrea Patricia Chancay Mendoza.; visualization, Jhon Henry Calle Poveda.; supervision, Michael Manrique Choez and Rider Quintana Souza; project administration, Walther Zhukov Paz y Miño Intriago and Lorena Garcia Lois; funding acquisition, José Miguel Rubio Cala. All authors have read and agreed to the published version of the manuscript.
Funding: This research received no external funding.
Institutional Review Board Statement: This article was prepared following the Declaration of Helsinki and approved by the institutional ethics committee through official letter No: UTM II 2018-011-OF of January 25/2018, and in compliance with article No. : 14 and 36 of the committee regulations (approved on October 24 October 24, 2021).
Informed Consent Statement: Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest: The authors declare no conflict of interest.
REFERENCES
1. Sánchez-Galarza, A., Delfino-Blanco, C., Rosa-Rodríguez, Y., & Torres-Pagán, L. (2019). Percepción de Salud General y Calidad de Vida de Puertorriqueños/as con Enfermedades Cardiovasculares. Salud & Sociedad, 9(3), 294-305. https://doi.org/10.22199/S07187475.2018.0003.00007
2. Huerta Patricio, Naranjo Ana María, Martínez Darío. Correlación entre Estudios Electrocardiográficos y Cinecoronariográficos en Enfermedades Coronarias. Int. J. Morphol. [Internet]. 2018 Dic [citado 2022 Nov 13]; 36(4): 1514-1518. Disponible en: http://www.scielo.cl/scielo.php?script=sci_arttext&pid=S0717-95022018000401514&lng=es. http://dx.doi.org/10.4067/S0717-95022018000401514.
3. Lazaro VL. 2014 PHA Clinical Practice Guidelines for the Diagnosis and Management of Patients with Coronary Heart Disease. ASEAN Heart J. 2016 March 23March 23; 24:3. doi: 10.7603/s40602-016-0003-6.
4. González Soriano LS, Lozano Espinosa DA, Bornachera Pinto DA. Caracterización de pacientes con dislipidemia en un hospital regional de colombia. RESPYN Rev Salud Pública y Nutr. 2020;19(4). DOI: https://doi.org/10.29105/respyn19.4-4
5. Domingues C, Ferreira MJV, Ferreira JM, Marinho AV, Alves PM, Ferreira C, Fonseca I, Gonçalves L. Prognostic Value of Isolated Elevated Troponin I Levels in Patients without Acute Coronary Syndrome Admitted to the Emergency Department. Arq Bras Cardiol. 2021 May;116(5):928-937. English, Portuguese. doi: 10.36660/abc.20190356. PMID: 34008817; PMCID: PMC8121477.
6. Moreno JS, Lépori AJ, Novoa P, De Elias R, Guglielmone R, Bono JO. Troponina T ultrasensible y CA125 como marcadores pronósticos en pacientes con enfermedad renal terminal en hemodiálisis. Rev Fac Cien Med Univ Nac Cordoba [Internet]. 27 de febrero de 2016 [citado 14 de noviembre de 2022];73(1). Disponible en: https://revistas.unc.edu.ar/index.php/med/article/view/13383
7. Cader FA, Banerjee S, Gulati M. Sex Differences in Acute Coronary Syndromes: A Global Perspective. J Cardiovasc Dev Dis. 2022 Jul 27;9(8):239. doi: 10.3390/jcdd9080239. PMID: 36005403; PMCID: PMC9409655.
8. Bazzino Óscar. Tercera definición universal de infarto de miocardio: Implicancias en la práctica clínica. Rev.Urug.Cardiol. [Internet]. 2013 Dic [citado 2022 Nov 13]; 28(3): 403-411. Disponible en: http://www.scielo.edu.uy/scielo.php?script=sci_arttext&pid=S1688-04202013000300014&lng=es.
9. Roffi M, Patrono C, Collet J, Mueller P, Valgimigli M, Andre-otti F. Guía ESC 2015 para el manejo de síndromes coronarios agudos en pacientes que presentan sin elevación persistente del segmento ST: Grupo de trabajo para el manejo de síndromes coronarios agudos en pacientes que presentan sin elevación persistente del segme. Eur Hear J [Internet]. 2016; 36:267–315. Available from: https://doi.org/10.1093/eurheartj/ehv320.
10. Ibáñez B. Guía ESC 2017 sobre el tratamiento del infarto agudo de miocardio en pacientes con elevación del segmento ST. Rev Esp Cardiol [Internet]. 2017 [cited 2022 Mar 11];70(12):1–61. Available from: https://www.revespcardiol.org/es-pdf-S0300893217306693
11. Velilla Moliner J, Gros Bañeres B, Povar Marco J, Santaló Bel M, Ordoñez Llanos J, Martín Martín A, et al. Rendimiento diagnóstico de la troponina de alta sensibilidad en el síndrome coronario agudo sin elevación del segmento ST. Med Intensiva. 2020 Mar 1;44(2):88–95.
12. Calvo-Fernández A, Izquierdo A, Subirana I, Farré N, Vila J, Durán X, et al. Markers of myocardial injury in the prediction of short-term COVID-19 prognosis. Rev Española Cardiol (English Ed. 2021;74(7).
13. Mauro V, Rafaelli A, Castillo Costa YB, Charask A, Fairman E, Zapata Mel LE, et al. Síndromes coronarios agudos sin elevación del segmento ST y troponina ultrasensible. ¿Es el final de la estrategia conservadora? Rev. argent. cardiol. [Internet]. 2018 Oct [citado 2022 Oct 30]; 86(5): 45-54. Disponible en: http://www.scielo.org.ar/scielo.php?script=sci_arttext&pid=S1850-37482018000500045&lng=es.
14. De Castro RN, Boqué C. Troponina elevada en pacientes sin síndrome coronario agudo Troponin Elevation in Patients Without Acute Coronary Syndrome. Rev Esp Cardiol. 2017;68(8).
15. Barón AM, García AA, Juan Guardela ML, Rodríguez MP, González C, Alarcón Robles P, et al. Comportamiento de los niveles de troponina I de alta sensibilidad en pacientes con enfermedad renal crónica estadio 5 en hemodiálisis. Acta Médica Colomb. 2017;42(4).
16. Silva E, Baltar VT, Pereira MP, Minuzzo L, Timerman A, Avezum Á. Artículo Original Comparación entre Troponina I Cardíaca y CK-MB masa en Síndrome Coronario Agudo Sin Supradesnivel de ST. Arq Bras Cardiol. 2018;96(3).
17. Lewandrowski KB. Special topics: Cardiac markers in myocarditis. Cardiac transplant rejection and conditions other than acute coronary syndrome. Vol. 34, Clinics in Laboratory Medicine. 2016.
18. Liu M, Shehu M, Herrold E, Cohen H. Prognostic value of initial elevation in cardiac troponin I level in critically ill patients without acute coronary syndrome. Crit Care Nurse. 2018;35(2).
19. Domingues C, Ferreira MJV, Ferreira JM, Marinho AV, Alves PM, Ferreira C, et al. Prognostic value of isolated elevated troponin I levels in patients without acute coronary syndrome admitted to the emergency department. Arq Bras Cardiol. 2021;116(5).
20. Bejarano JM, Cuixart CB. Factores de riesgo cardiovascular y atención primaria: evaluación e intervención [Cardiovascular risk factors and Primary Care: evaluation and intervention]. Aten Primaria. 2011 Dec;43(12):668-77. Spanish. doi: 10.1016/j.aprim.2011.10.002. Epub 2011 Nov 17. PMID: 22099938; PMCID: PMC7025141.
21. Ding XS, Wu SS, Chen H., Zhao XQ, Li HW Los niveles altos de glucosa al ingreso predicen un peor resultado clínico a corto plazo en pacientes no diabéticos con infarto agudo de miocardio: un estudio observacional retrospectivo. Trastornos cardiovasculares BMC. 2019; 19 (1): pág. 163. doi: 10.1186/s12872-019-1140-1.
22. Cui CY, Zhou MG, Cheng LC, et al. La hiperglucemia al ingreso como predictor independiente del pronóstico a largo plazo en pacientes con infarto agudo de miocardio sin diabetes: un estudio retrospectivo. Revista de Investigación de la Diabetes. 2021; 12 (7):1244–1251. doi: 10.1111/jdi.13468.
23. Liu W, Li Z, Xing S, Xu Y. Effect of Admission Hyperglycemia on Short-Term Prognosis of Patients with Non-ST Elevation Acute Coronary Syndrome without Diabetes Mellitus. J Diabetes Res. 2021 Dec 6; 2021:1321289. doi: 10.1155/2021/1321289. PMID: 34912898; PMCID: PMC8668326.
24. Sprockel J, Diaztagle J. Precisión diagnóstica de un modelo de redes bayesianas en los síndromes agudos. Rev la Univ Ind Santander Salud. 2019;47(2).
25. Zamri WNAWM, Shafii N, Ismail TST, Zakaria AZ, Yaacob NM, Soh NAAC. Elevation of highly sensitive cardiac troponin t among end-stage renal disease patients without acute coronary syndrome. Malaysian J Med Sci. 2021;28(5).
26. Iannaccone M, Gili S, De Filippo O, D’Amico S, Gagliardi M, Bertaina M, et al. Diagnostic accuracy of functional, imaging and biochemical tests for patients presenting with chest pain to the emergency department: A systematic review and meta-analysis. Eur Hear J Acute Cardiovasc Care. 2019;8(5).
27. Rodrigo Orozco B. Enfermedad cardiovascular (ECV) en la enfermedad renal crónica (ERC). Revista Médica Clínica Las Condes. 2015; 26(2): 142-155. https://doi.org/10.1016/j.rmclc.2015.04.003.
28. Liebetrau C, Elsässer A, Nef H, Möllmann H. Management of acute coronary syndrome. Kardiologe. 2018;12(5).
29. Barón, A. M., García, A. A., Juan Guardela, M. L., Rodríguez, M. P., González, C., Alarcón Robles, P., & Betancur, M. C. (2017). Comportamiento de los niveles de troponina I de alta sensibilidad en pacientes con enfermedad renal crónica estadio 5 en hemodiálisis. Acta Médica Colombiana, 42(4), 210-214. https://doi.org/10.36104/amc.2017.1107
30. Chaulin AM. The Importance of Cardiac Troponin Metabolism in the Laboratory Diagnosis of Myocardial Infarction (Comprehensive Review). Biomed Res Int. 2022 March 30March 30; 2022:6454467. doi: 10.1155/2022/6454467. PMID: 35402607; PMCID: PMC8986381.
31. Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD; Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction (2018). J Am Coll Cardiol. 2018 Oct 30;72(18):2231-2264. doi: 10.1016/j.jacc.2018.08.1038. Epub 2018 August 25August 25. PMID: 30153967.
32. Calvo-Fernández A, Izquierdo A, Subirana I, Farré N, Vila J, Durán X, et al. Markers of myocardial injury in the prediction of short-term COVID-19 prognosis. Rev Española Cardiol (English Ed. 2021;74(7).
33. Hamm CW, Goldmann BU, Heeschen C, Kreymann G, Berger J, Meinertz T. Emergency room triage of patients with acute chest pain by means of rapid testing for cardiac troponin T or troponin I. N Engl J Med. 1997 December 4December 4;337(23):1648-53. doi: 10.1056/NEJM199712043372302. PMID: 9385123.
34. Jaffe AS, Ordonez-Llanos J. Troponina cardiaca ultrasensible: de la teoría a la práctica clínica. Rev Española Cardiol. 2019;66(9).doi: 10.1016/j.recesp.2013.04.021
35. Cullen L, French JK, Briffa TG, Redfern J, Hammett CJ, Brieger DB, Parsonage WA, Lefkovits J, Ellis C, Astley C, Howell TE, Elliott JM, Chew DP. Availability of highly sensitive troponin assays and acute coronary syndrome care: insights from the SNAPSHOT registry. Med J Aust. 2015 January 19 January 19;202(1):36-9. doi: 10.5694/mja13.00275.
Received: 25 June 2023/ Accepted: 26 August 2023 / Published:15 September 2023
Citation: Valdés Dupeyrón O, Quintero Arcentales M, Espinales-Casanova L, Chilán Santana C I, Howland Alvarez I, Villar Inclan A, González Robles J, Lois Mendoza N, Suarez Fernández JC, Chancay Mendoza A P, Calle Poveda J H, Manrique Choez G M, Paz y Miño Intriago W Z, Rubio Cala J M, Garcia Lois L, Quintana Souza R, Barrueto Blanco Y, Diagnostic utility of high-sensitive troponin T in patients with acute coronary syndrome.Revis Bionatura 2023;8 (3) 52. http://dx.doi.org/10.21931/RB/2023.08.03.52
