2022.07.03.41
Files > Volume 7 > Vol 7 No 3 2022
1 College of medicine/ Mustansiriyah University, Iraq,
2 Iraqi Center for cancer and medical genetics research/ Mustansiriyah University, Iraq,
3 Al-Mussaib technical college/ Al-FuratAl-Awsat Technical University, Iraq. [email protected],
4 Department of Biology, College of Science, University of Baghdad, Baghdad- Iraq,
* Correspondence authors email: [email protected], [email protected],
Available from: http://dx.doi.org/10.21931/RB/2022.07.03.41
ABSTRACT
Chronic myeloid leukemia (CML), is one of the myeloproliferative disorders with a characteristic cytogenetic abnormality resulting in the BCR-ABL fusion gene. Imatinib Mesylate is an effective agent for treating patients in all stages of CML. According to the annual Iraqi cancer registry 2019, the total number of chronic myeloproliferative disorders was 338. The percentage and incidence rates were 0.94% and 0.86%, respectively, with a higher incidence rate in males than females (1.12 in males and 0.60 in females). In this registry, no details about CML, so this study aimed to estimate the number of CML patients who attended the national center of hematology from 2005 until 2020 and investigate their epidemiological and clinic-pathological data. All data were obtained from the National Center of Hematology /Baghdad. Data regarding annual admission, number of deaths, and information about age, regions, and sex, were collected from patient cards. Interview and history taking from the patient and reviewing their clinical features at diagnosis were performed, and then statistical analysis was achieved. Two hundred sixteen patients were registered as CML; among them, 163 are still alive, while 53 died. The mean age at diagnosis was 40.39 ±14.30, with a male-to-female ratio of 1:1.16. The pediatrics age group comprises 3.7% of total cases and 1.8 % and 9.4% in the alive and dead groups, respectively. The percentages of death were higher in the pediatric age group, 62,5%( 5 /8), followed by the patient group who were ≥60 years, 42.1%(8/19), while it was the least in adults < 60 years, 21.1% (40/189). In conclusion, the studied patients with CML were younger than the globally reported ages at diagnosis, with predominant female patients. Females had better survival, while children and the elderly were the worse. Most patients were symptomatic at diagnosis; however, a good outcome is achieved when treated with IM.
Keywords: CML, Imatinib, leukemia,
INTRODUCTION
Chronic myeloid leukemia (CML) is one of the myeloproliferative disorders in which the granulocyte proliferates and can differentiate but not achieve full maturation. Philadelphia (Ph) chromosome is a characteristic cytogenetic abnormality resulting in BCR-ABL fusion protein, constitutive tyrosine kinase activity and promotes the proliferation of leukemia cells via multiple mechanisms1. An effective agent for the treatment of patients in all stages of CML is Imatinib Mesylate (IM), which is a selective inhibitor of ABL and its derivative BCR-ABL. According to worldwide cancer data by the American Institute for Cancer Research, the global incidence of CML ranges from 0.7 per 100,000 to 1.5 per 100,000 persons. The lowest incidence is in Sweden therapy, considered the first-line treatment for newly diagnosed CML 2,3 and China, and the highest in Switzerland and the United States.4 CML is an age-related disease that commonly affects the elderly (6 years old) in western countries and 50 years in Africa and Asia.5 Less than 10 percent of all cases occur in subjects between 1 and 20 years old, and CML represents approximately 3 % of all childhood leukemias. Multiple occurrences of CML in families are rare. No concordance of the disease between identical twins has been found. There is no evidence of a familial predisposition to CML.6 The global age-standardized incidence rate is 0.52 /100000 in males and 0.36 in females.7 According to the annual Iraqi cancer registry 2019, the total number of chronic myeloproliferative disorders was 338. The percentage and incidence rates were 0.94% and 0.86%, respectively, with a higher incidence rate in males than females ( 1.12 in males and 0.60 in females).8 In this registry no details about CML, so in this study, all the CML patients on IM therapy since 2005 were reviewed, and the available data were included and also estimating the number of CML patients who attended the national center of hematology from the year 2005 to 2020 and investigated the epidemiological and clinicopathological data of them.
MATERIALS AND METHODS
The scientific committee approved the study of the Iraqi Center of Cancer and Medical Genetic Researches with the agreement and help of the National Center of Hematology.
A consultant hematology team diagnosed the patients according to the clinical and laboratory findings, such as the history and clinical examination, followed by laboratory tests including complete blood count, blood film, cytogenetic and molecular study and other biochemical investigations. All the patients were in chronic phase CML and treated with IM. All data were derived from the National Center of Hematology /Baghdad. Data regarding annual admission, number of deaths, and information about age, regions, and sex, were collected from patient cards. Interview and history taking from the patient and reviewing their clinical features at diagnosis were performed, and then statistical analysis was done.
RESULTS AND DISCUSSION
From 2005 until 2020, (216) patients were registered as CML; among them, 163 are still alive, while 53 died. The annual number of patients registered from 2005 to 2020 is shown in figure (1)and table (1), in which a higher number of patients was during the years 2005 and 2016 (18,17 cases, respectively). Death of 11,4,7,and2 patients were registered during the years 2005, 2006, 2007, and 2008 respectively, while no death during the following eleven years from 2009 to 2019 and only two death during the year 2020. The improved survival over the years is highly attributed to the better management and treatment of CML by (IM).
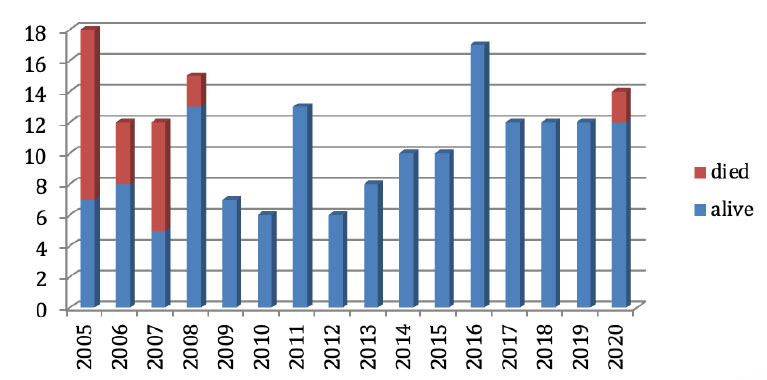
Figure 1. The annual number of patients registered from 2005 to 2020
As shown in table 1, the mean age at diagnosis was 40.39 ±14.30 ranging from 3 to 77 years, with a median age of 39. In many other studies, comparable mean ages were reported, such as 43.4,42, 43.3,48, 52,46, and 55. 9-15 In the alive group, the mean age was 43.09 ±13.09 ranging from 14-77 years with a median age of 38; in the dead group, the mean age was 37.90 ±14.20 from 3-75 with a median age of 37 years. Significantly lower mean age among the dead group, with the presence of 5 death out of 8 patients in pediatrics age group 3,12,15,16, and17 years. The pediatric age group comprises 3.7% of total cases and 1.8 % and 9.4% in the alive and dead groups, respectively. The percentages of death were higher in the pediatric age group, 62,5% (5 /8), followed by the patient's group who were ≥60 years, 42.1%(8/19), while it was the least in adults < 60 years, 21.1% (40/189). Chronic myelogenous leukemia in pediatrics is rare and comprises 2-3% of all leukemias of childhood and less than 10 % of CML. It has an aggressive clinical presentation than adults, 6,16 on the other extreme CML in the elderly also had poor survival, and advanced age is considered an independent prognostic factor. There are no biological or genetic changes that are related to aging, but age-related co-morbidity, immune defects, and bone marrow stromal changes may cause a more aggressive disease.17Chronic myeloid leukemia can affect all age groups, 18-20; however, in this study, the majority of cases were adults below the age of 60 years. This distribution is similar to that mentioned in other Iraqi studies 9 and lower than other western studies. 20-22 Young patients, regardless of prognostic factors, are generally well.23-25 There is no proven evidence that different biological or genetic factors are implicated, but this could be due to ethnic and demographic variations. A slightly higher number of patients were female, with a male-to-female ratio of 1:1.16 in total patients and 1:1.76 in alive patients, but with a reverse ratio of 3.41:1 in the dead group, where 77.3% of death cases were male.
Globally, CML's incidence and death cases increased slightly in males while decreasing in females.7 But in this study, there was a better survival of females, which may be due to better general longevity, early disease diagnosis, or favorable risk factors.

Table 1. Age and sex of CML patients, including alive and dead groups.
The appearance of clinical signs and symptoms related to the disease was reported in 95% of cases. The main presenting symptom was fatigue and weakness in 80% of cases, and the main presenting sign was splenomegaly in 85% of cases. Other signs and symptoms include fever in 72%, bone pain in 65%, abdominal pain and night sweating in 52% of cases. Only 5 % are accidentally diagnosed while they investigate other medical problems. As shown in figure .2

Figure 2. The main presenting signs and symptoms.
All the presenting signs and symptoms indicated a hypermetabolic state and delayed diagnosis. At the same time, only 5% were asymptomatic .these findings were controversial to western data, in which 40% of cases were asymptomatic.11This discrepancy is attributed to better health care services and early detection of disease via routine check-ups in developed countries.
CONCLUSIONS
The studied patients with CML were younger than the globally reported ages at diagnosis with predominant female patients. Females had better survival, while children and the elderly were the worse. Most patients were symptomatic at diagnosis; however, a good outcome is achieved when treated with IM. Further study to understand the epidemiology of CML and the causes of discrepancies, improve health care, and encourage routine check-ups for early detection of disease, particularly in the young.
Funding: Nil.
Acknowledgments The authors would like to thank Mustansiriyah University /Faculty of medicine, particularly the Department of Pathology and Forensic Medicine, Iraqi Center Of Cancer and Medical Genetics Researches and National center Of Hematology.
Conflicts of Interest: There are no conflicts of interest
REFERENCES
1. Bain BJ. Leukaemia diagnosis. John Wiley & Sons; 2017.ISBN 9781119210542.
2. Shanmuganathan N, Hiwase DK, Ross DM. Treatment of chronic myeloid leukemia: assessing risk, monitoring response, and optimizing outcome. Leukemia & Lymphoma. 2017; 58(12):2799-810.
3. Chauhan R, Sazawal S, Pati HP. Laboratory monitoring of chronic myeloid leukemia in patients on tyrosine kinase inhibitors. Indian Journal of Hematology and Blood Transfusion. 2018; 34(2):197-203.
4. Huang X, Cortes J, Kantarjian H. Estimations of the increasing prevalence and plateau prevalence of chronic myeloid leukemia in the era of tyrosine kinase inhibitor therapy. Cancer. 2012; 118(12):3123-3127.
5. Mendizabal AM, Younes N, Levine PH. Geographic and income variations in age at diagnosis and incidence of chronic myeloid leukemia. International journal of hematology. 2016;103(1):70-80.
6. Nguyen LT, Guo M, Naugler C, Rashid-Kolvear F. Incidence of chronic myeloid leukemia in Calgary, Alberta, Canada. BMC Research Notes. 2018;11(1):1-5.
7. Ning L, Hu C, Lu P, Que Y, Zhu X, Li D. Trends in disease burden of chronic myeloid leukemia at the global, regional, and national levels: a population-based epidemiologic study. Experimental hematology & oncology. 2020; 9(1):1-4.
8. Alwan NA, Tawfeeq FN, Mallah N. Demographic and clinical profiles of female patients diagnosed with breast cancer in Iraq. Journal of Contemporary Medical Sciences. 2019; 5(1):14-19.
9. Alagele MH, Alwash MM, Ahmed AA. Vascular Endothelial Growth Factor Receptor 2 (VEGFR2) Gene Polymorphism And Treatment Outcome Following Imatinib Therapy In Iraqi Patients With Chronic Myeloid Leukemia. European Journal of Molecular & Clinical Medicine. 2020;7(2):4847-4857.
10. Mjali A, Al-Shammari HH, Abbas NT, Azeez ZD, Abbas SK. Leukemia epidemiology in Karbala province of Iraq. Asian Pacific Journal of Cancer Care. 2019; 4(4):135-139.
11. Sih BT, Alqasim AM, Ajil AH. The effect of gamma ray on total leukocytes, lymphocytes and neutrophils on blood samples of smokers compared to non-smoker donors. Iraqi Journal of Hematology. 2017; 6(1):1-5.
12. Awidi A, Abbasi S, Alrabi K, Kheirallah KA. Generic imatinib therapy among Jordanians: an observational assessment of efficacy and safety in routine clinical practice. Clinical Lymphoma Myeloma and Leukemia. 2017 Dec 1;17(12):e55-61..
13. Algahtani FH, Alqahtany FS. Evaluation and characterisation of Chronic myeloid leukemia and various treatments in Saudi Arabia: A retrospective study. Journal of Infection and Public Health. 2020; 13(2):295-298.
14. Godoy CR, Levy D, Giampaoli V, Chamone DA, Bydlowski SP, Pereira J. Circulating endothelial cells are increased in chronic myeloid leukemia blast crisis. Brazilian Journal of Medical and Biological Research. 2015; 48:509-514.
15. Kim DH, Xu W, Kamel-Reid S, Liu X, Jung CW, Kim S, Lipton JH. Clinical relevance of vascular endothelial growth factor (VEGFA) and VEGF receptor (VEGFR2) gene polymorphism on the treatment outcome following imatinib therapy. Annals of oncology. 2010; 21(6):1179-1188.
16. Hijiya N, Schultz KR, Metzler M, Millot F, Suttorp M. Pediatric chronic myeloid leukemia is a unique disease that requires a different approach. Blood, The Journal of the American Society of Hematology. 2016; 127(4):392-399.
17. Balducci L, Dolan D. Chronic Myelogenous Leukemia (CML) in the elderly. Mediterranean Journal of Hematology and Infectious Diseases. (2014),6(1):e2014037.
18. Pushpam D, Bakhshi S. Paediatric chronic myeloid leukaemia: Is it really a different disease?. The Indian Journal of Medical Research. 2019;149(5):600.
19. Jbireal JM, Azab AE, Alzahani S, Elshareef M. Haematological and cytogenetic changes in CML patients treated with imatinib mesylate in Western Libya. Hematol Transfus Int J. 2019;7(3):50-57.
20. Kalmanti L, Saussele S, Lauseker M, Proetel U, Müller MC, Hanfstein B, Schreiber A, Fabarius A, Pfirrmann M, Schnittger S, Dengler J. Younger patients with chronic myeloid leukemia do well in spite of poor prognostic indicators: results from the randomized CML study IV. Annals of hematology. 2014;93(1):71-80.
21. Fadhel AA, Yousif AK. Correlation of glycated hemoglobin (Hba1c) and serum uric acid in type-2 diabetic patients. Indian Journal of Public Health. 2019;10(5):105.
22. Hochhaus A, Larson RA, Guilhot F, Radich JP, Branford S, Hughes TP, Baccarani M, Deininger MW, Cervantes F, Fujihara S, Ortmann CE. Long-term outcomes of imatinib treatment for chronic myeloid leukemia. New England Journal of Medicine. 2017 9;376(10):917-927.
23. Holmes L, Hossain J, Desvignes-Kendrick M, Opara F. Sex variability in pediatric leukemia survival: Large cohort evidence. International Scholarly Research Notices. 2012;2012.
24. Ahmed AA, Khaleel KJ, Fadhel AA. Potential effect of Imatinib on some sex hormones for male patients of Chronic Myelogenous Leukemia in Baghdad province. Bionatura 2021 ,6(4):2193–2195.
25. Berger U, Maywald O, Pfirrmann M, Lahaye T, Hochhaus A, Reiter A, Hasford J, Heimpel H, Hossfeld DK, Kolb HJ, Löffler H. Gender aspects in chronic myeloid leukemia: long-term results from randomized studies. Leukemia. 2005; 19(6):984-989.
Received: 15January 2022 / Accepted: 20 July 2022 / Published:15 August 2022
Citation: Anwer Ahmed A, Khaleel K J, Abbas Fadhel A, Laftaah Al-Rubaii BA. Chronic Myeloid Leukemia: A retrospective study of clinical and pathological features. Revis Bionatura 2022;7(3) 41. http://dx.doi.org/10.21931/RB/2022.07.03.41
