2023.08.03.28
Files > Volume 8 > Vol 8 No 3 2023
Efficacy of an educational program based on health belief model to enhancing weight control behaviors among employees in University of Mosul: a randomized controlled trial
1. College of Nursing / University of Mosul /IRAQ
2. College of Nursing / University of Baghdad/IRAQ
3. Nursing of CH, College of Nursing / University of Mosul/ IRAQ
Available from: http://dx.doi.org/10.21931/RB/2023.08.03.28
ABSTRACT
Weight management is complex for most individuals, as indicated by the high numbers of obesity worldwide. Obesity has increased dramatically over the past decades. The study aims to determine the efficacy of an educational program based on the health belief model to improve weight control behaviors among overweight and obese employees at the University of Mosul. The study design is genuinely experimental, using the randomized controlled trial approach to enhance weight control behaviors among employees at the University of Mosul from January 10, 2021, to March 15, 2022. A probability simple random sample of 576 employees from faculties of different specializations was selected. The sample was chosen from a homogeneous group of 280 employees. Random selection and random assignment are used to create the experimental (40) and control group (40). The study results showed that in the pre-test, there was no significant difference between the experimental group and the control group in employee behaviors related to weight to control at a P-value (0.378). It showed an improvement in the behaviors of the study group toward weight control at (0.000) in the first and second post-tests. Also, the body mass index improved after three months for the experimental group at a P-value of 0.01. The researchers concluded that the intervention through the health beliefs model positively affected many health behaviors that affect weight maintenance.
Keywords: Efficacy, Health Belief Model, Weight, Behaviors.
INTRODUCTION
Weight management is complex for most individuals, as indicated by the high numbers of obesity worldwide. Obesity has increased dramatically over the past decades. Unfortunately, this epidemic is not limited to adults but also to children globally. Developing a weight management plan is essential for everyone. Body Mass Index (BMI), a simple screening technique dependent on weight and height, is frequently related to a person's body fat percentage. Adults with a BMI of 25 to 29.9 are termed overweight, while those with a BMI of 30 or more are classified as obese. Whereas a BMI of over 30 is not the only sign of obesity, it is a straightforward, low-cost diagnostic that offers healthcare professionals information about a patient's general health. All the patients and third-party insurance providers save money by maintaining a healthy weight4,5, 8,9,10. People cannot take preventive and curative steps toward obesity unless they have knowledge and motivation and believe that they are exposed to severe life-threatening diseases due to obesity., according to the Health Belief Model (HBM). Individuals must also feel that a weight-control intervention is desirable and that there are minimal obstacles to its implementation11,12. The study aims to determine the efficacy of an educational program based on the health belief model to improve weight control behaviors among overweight and obese employees at the University of Mosul.
MATERIALS AND METHODS
The proper experimental design using the randomized controlled trial approach is conducted to determine the efficacy of an educational program based on the health belief model to enhance weight control behaviors among employees in the University of Mosul from January 10, 2021, to March 15, 2022. A probability simple random sample of 576 employees from faculties of different specializations was selected. The sample was selected from a homogeneous group of 280 employees. Random selection and random assignment are used to create the experimental (40) and control group (40). An intervention program has been developed, in line with the findings of the assessment needs of employees related to weight control, on the Health Beliefs Model in enhancing employee's behavior about bodyweight control. The program consists of four main sessions. The study tool is (Behavioral Strategies for weight management in overweight adults) This questionnaire consists of 5 parts, including Physical activity (6 items), Dietary impulse control (7 items), Social support (4 items), Advanced dietary planning (5 items), and weight loss planning and monitoring (5 items). Responses to these items range from (1) Never to (2) Sometimes, and (3) Always with a higher score indicating higher agreement with the behaviors. Data is analyzed using the "Statistical Package for Social Science" (SPSS) software for Windows (Version 24)13,14,15.
RESULTS AND DISCUSSION
According to the results, the mean age and standard deviation for the study and the control groups were (41.17 ± 0.82) and (38.82 ± 0.87), respectively. The majority of the participants in the study group are 60% males. Most of them were married (85%), while the control group (67.5%) males and (80%) were married. The results within the same table showed that the majority of employees are engaged in office work that does not require physical activity, (87.5%) of the study group and (85%) of the control group, and the majority of them have a bachelor's degree, (75%) of the experiment group, (67.5%) of the control group. The study's findings were comparable to many studies showing that overweight and obesity affect middle-aged adults. A study in India showed that the average age of 47 is the majority who try to control their weight to avoid diseases16,17. The other survey in Iraq by 18 demonstrates that overweight obesity may increase in the middle age of 40. Adults have a relatively low level of physical activity, which tends to decline as they age. The lack of physical activity and unhealthy food is one of the most important causes of weight gain, as the level of adult physical activity is very low and tends to decline with age 8. The pre-test results showed that most of the study participants for both groups were obese stage 1 BMI (30-34.9), (57.5%) of the study group, and 52.5% of the control group. The average weight of the two groups is 33.60, with a standard deviation of 3.93, and there was no significant difference in weight between the two groups, according to the results. In another survey by the World Health Organization in Iraq, 26% of Iraqi men and 38% of Iraqi women aged 25-65 years were obese19. The study results from interpretation show that the participants were homogeneous within themselves because one of the prerequisites of (randomized controlled trials (RCTs) is pool homogeneity, and RCTs are preparing the best way to determine the efficacy to resolve a specific problem through the implementation of (HBM), so the results of both groups (control and study) appeared homogeneous. Adult weight reduction programs have been proven to help people reduce weight and, more importantly, improve their health.
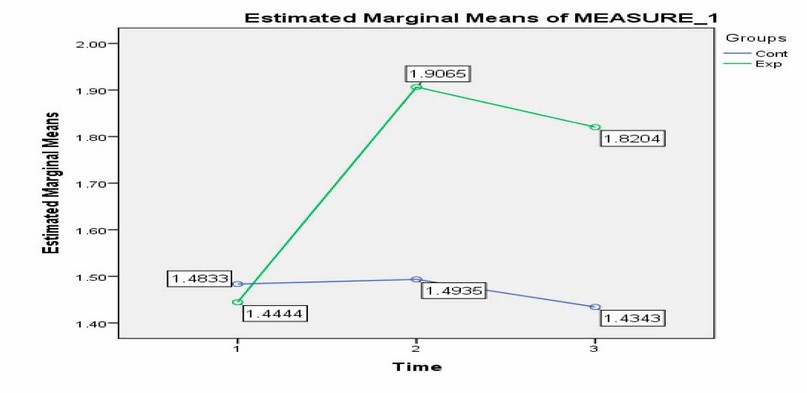
Figure 1. Changes in behaviors related to weight control among employees in the University of Mosul for the study and control groups throughout the three times.
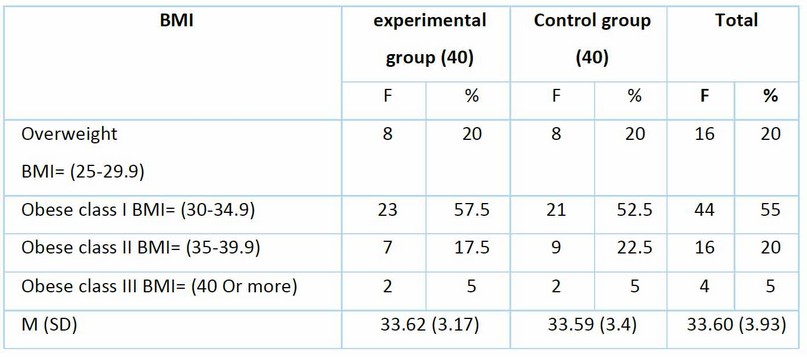
Table 1. Body mass index and homogeneity between control and experimental groups
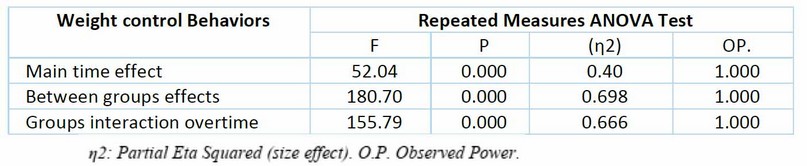
Table 2. Repeated measures ANOVA tests for changing the health behaviors related to weight control among employees.
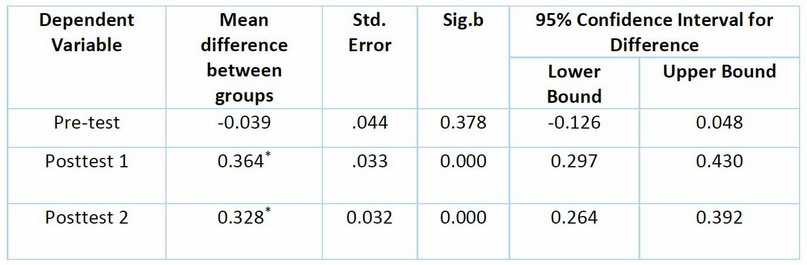
Table 3. Binary comparisons between the experimental and control groups over time.
Table 4. Efficacy of health beliefs intervention in controlling body weight for the experimental and control groups.
Diet, exercise, and behavior change instruction are the most well-known weight loss methods; as such, studies like the one conducted by 20 among overweight and moderately obese participants, a weight loss program focused on behavior modification or intervention improved health-related quality of life21`.The Behavioral Risk Factor Surveillance System reported an increase in the rates of overweight and obesity among adults under 30 years old with low educational levels. The increase results from a combination of factors, including food behaviors and the constant eating of fast food in restaurants. They were eating light snacks between main meals, excessive intake of fatty foods, low physical activity, watching television and video games, and finally, unhealthy sleep behaviors. Then, two months later, both groups were given a post-test 2 to determine the efficacy of the education program. The primary goal of this stage was to determine whether the educational program was effective in helping study group participants maintain a healthy weight. According to the studies, there was an increase in the value of (Physical activity, dietary impulse control, dietary planning, monitoring weight, and family and friend Support) over time. The result showed no significant difference in the mean of employees' behaviors before the study intervention and control groups. However, the difference was significant after the intervention at a P-value (0.05), indicating that health education positively affected changing participants' weight control behaviors. After completing the intervention, a post-test-2 calculated the BMI for both groups. The study outcomes revealed a significant difference between the study group's baseline test and post-test 2 of body mass index. This means that the intervention has had a positive impact on the BMI. However, there were no statistically significant differences in BMI for employees in the control group between pre-test and post-test 2. Several previous studies have shown that the health belief model can change behaviors related to weight control, including a study conducted on adolescents in Iran, which showed an improvement in body mass index after 3 months of the program. A previous experiment conducted by 26 revealed significant differences between the groups after three months of follow-up in waist circumference, weight loss, BMI, resting heart rate, blood pressure, physical activity, sweetened beverage consumption, and dietary beliefs.
CONCLUSION
The researchers concluded that the intervention through the health beliefs model positively affected many health behaviors that affect weight maintenance, including physical activity, controlling food impulses, dietary planning, monitoring body weight, and supporting family and friends to control weight. All of these behaviors led to a clear improvement in weight control of the study group approximately three months after the start of the intervention.
Funding
This research received no external funding.
Informed Consent Statement:
Not applicable
Acknowledgment
All thanks and appreciation to the staff working at the University of Mosul, as well as the University, for helping us obtain the research sample
Conflicts of Interest
The author declares that there is no conflict of interest in this study.
REFERENCES
1. Odysseos C, Avraamidou M. Weight management for athletes: Important things to be considered. Arab Journal of Nutrition and Exercise (AJNE). 2016:155-70.
2.Naji AB, Ahmed MM, Younis NM. Adherence to the Preventive Measures Against COVID-19 teachers at the University of Mosul. In J Med Tox Leg Med 2021;24(3&4).pp:273_277.
3. Al-Ghurairi SA, Younis NM, Ahmed MM. Prevalence of weight gain among students of Mosul University, Iraq, during quarantine 2020. Rawal Medical Journal. 2022 Jul;47(3).
4. Fleary SA, Ettienne R. Inherited or behavior? What causal beliefs about obesity are associated with weight perceptions and decisions to lose weight in a US sample?. International Scholarly Research Notices. 2014;2014.
5. Houston KA. A systematic review of literature on the effectiveness of behavioral weight loss programs to achieve weight reduction. J Obes Weight Loss Ther. 2012;3(156):2.
6. Ibrahim RM, Idrees NH, Younis NM. Epidemiology of leukemia among children in Nineveh Province, Iraq. Rawal Medical Journal. 2023 Mar 3;48(1):137-.
7. Taher AK, Younis NM. Effect of a trans theoretical model in improving behaviors of health care workers related to electronic hookah in Mosul, Iraq. Rawal Medical Journal. 2023 Mar 3;48(1):228-.
8. Tang W, Aggarwal A, Moudon AV, Drewnowski A. Self-reported and measured weights and heights among adults in Seattle and King County. BMC obesity. 2016 Dec;3:1-8.
9. Ahmed MM, Younis NM, Dhahir NM, Hussain KN. Acceptance of Covid-19 vaccine among nursing students of Mosul University, Iraq. Rawal Medical Journal. 2022 Apr;47(2):254-.
10. Muwfaq Younis N. Efficacy of Health Beliefs Model-Based Intervention in Changing Substance Use Beliefs among Mosul University Students: A Randomized Controlled Trial. Revis Bionatura 2022; 7 (2) 35.
11. Louis JP. Exploring Constructs of the Health Belief Model as Predictors To Haitian Men's Intention To Screen for Prostate Cancer. Urologic Nursing. 2019 Mar 1;39(2).
12. MacDonald, T. M. Factors that Influence Overweight and Obese Mens Participation in Healthy Eating, Exercise, and Weight Management Programs.2012.pp: 148.
13. Mohammad FH, Noori LK, Younis NM. Assessment of nutritional habits among Mosul University Students regarding breakfast. Rawal Medical Journal. 2023 Mar 3;48(1):96-.
14. Nasir MY, Rian MI, Nada HI. Prevalence of snake bite among children in Nineveh Governorate/Iraq: A retrospective study. International Journal of Medical Toxicology & Legal Medicine. 2022;25(3and4):166-9.
15. Karki S, Pradhan M, Rai A. Warts among Patients Visiting the Outpatient Department of Dermatology in a Tertiary Care Centre: A Descriptive Cross-sectional Study. Journal of the Nepal Medical Association. 2022 Sep 1;60(253).
16. Karki S, Pradhan M, Rai A. Warts among Patients Visiting the Outpatient Department of Dermatology in a Tertiary Care Centre: A Descriptive Cross-sectional Study. Journal of the Nepal Medical Association. 2022 Sep 1;60(253).
17. Mansour AA, Al-Maliky AA, Salih M. Population overweight and obesity trends of eight years in Basrah, Iraq. Epidemiol. 2012;2(1):110.
18. Pengpid S, Peltzer K. Overweight and obesity among adults in Iraq: Prevalence and correlates from a national survey in 2015. International journal of environmental research and public health. 2021 Apr 15;18(8):4198.
19. Younis NM, Ahmed MM, Abdulsalam RR. Assessing the quality of life in palliative care. International Journal of Medical Toxicology & Legal Medicine. 2021;24(3and4):115-8.
20. Rezapour B, Mostafavi F, Khalkhali H. "Theory Based Health Education: Application of Health Belief Model for Iranian Obese and Overweight Students about Physical Activity" in Urmia, Iran. International Journal of Preventive Medicine. 2016;7.
21. Semlitsch T, Stigler FL, Jeitler K, Horvath K, Siebenhofer A. Management of overweight and obesity in primary care—A systematic overview of international evidence‐based guidelines. Obesity Reviews. 2019 Sep;20(9):1218-30.
22. Abbas AS, Younis NM. Efficacy of Pender's Health Promotion-based Model on Intervention for Enhancing University of Mosul Hypertensive Employees' Eating Behaviors: A randomized Controlled Trial. Revis Bionatura. 2022;7(3):35.
23. Soliman NM, Elsayied HA, Shouli MM. Application of health belief model among youth at high risk for obesity in West Bank (Palestine). American Journal of Nursing Science. 2018;7(3-1):86-96.
24. Adea MK, Lefta RM, Younis NM. Impact of psychosocial aspect parameters on psoriasis patients' quality of life at an outpatient clinic in Al-Dewania City, Iraq. Rawal Medical Journal. 2022 Dec 11;47(4):892-.
25. Melo-Betancourt LG, Castaño-Marín JC, Narváez-Solarte W. Atividade física, sobrepeso e obesidade nos motoristas do transporte público em Manizales, Colômbia. Hacia la Promoción de la Salud. 2021 Jan;26(1):132-47.
26. Ahmed MM, Younis NM, Abdulsalam RR. Assessment of changes in sleep habits in elementary students during covid_19 lockdown. International Journal of Medical Toxicology & Legal Medicine. 2022;25(1and2):76-80.
27. Yerro L. How effective is an adult weight loss program on medication and exercise regimens. California State University, Long Beach; 2015.
28. Mukhlif HH, Younis NM. Evaluation of the association between internet addiction and fatigue among undergraduate students at universities in Mosul city, Iraq: A cross-sectional study. Rawal Medical Journal. 2022 Dec 11;47(4):829-.
Received: 28 May 2023/ Accepted: 15 July 2023 / Published:15 September 2023
Citation: Ahmed M M, Naji A B, Younis N M. Efficacy of an educational program based on health belief model to enhancing weight control behaviors among employees in the University of Mosul: a randomized controlled trial. Revis Bionatura 2023;8 (3) 28. http://dx.doi.org/10.21931/RB/2023.08.03.28
