2021.06.04.28
Files > Volume 6 > Vol 6 No 4 2021
Schizophrenia and refractory status epilepticus in a male patient with anti-NMDA auto-immune encephalitis: A case report
Available from: http://dx.doi.org/10.21931/RB/2021.06.04.28
ABSTRACT
Encephalitis is the inflammation of the central nervous system cells as a result of activation of immune cells, antibodies, or proteins by a reaction with pathogens or self-body components; when this happens, a malfunction of the immune system is known as this an auto-immune disease. Auto-immune encephalitis characterizes 21% of all encephalitis and manifests with loss of memory and cognition, personality deviations, neurologic deficit, aphasia, seizures, and epilepsy. Treatment is guaranteed using steroids, immunoglobulins, and plasmapheresis, and as a second-line therapy, cyclophosphamide or rituximab is used. In cases related to tumors, surgery is part of the treatment. An unusual case of auto-immune encephalitis is reported.
Keywords: Encephalitis – Auto-immune diseases – Epilepsy – Mental disorders
INTRODUCTION
Encephalitis is the inflammation of the central nervous system cells as a result of activation of immune cells, antibodies, or proteins by a reaction with pathogens or self-body component; when this happens, a malfunction of the immune system is known as this an auto-immune disease 1.
Encephalitis's annual incidence is about 5-8 cases per 100000 inhabitants, and 21% of these cases are related to auto-immune encephalitis 2. Epidemiologic studies report that young patients of age 21 are most frequently affected since auto-immune encephalitis can occur between 2 months and 85 years of age 3. In Ecuador, statistical data about this disease are not available.
Early diagnosis and treatment prevent the diminished quality of life with memory loss, cognition deficits, personality disorders, paresis and paresthesia, aphasia, seizures, and coma 4.
The following case report presents a male patient with a schizophrenia-like disease followed by a refractory status epilepticus (RSE) diagnosed with anti-NMDA auto-immune encephalitis. It is considered an unusual presentation due to male gender and RSE, so it is essential to recognize presentation variants of this disease to accomplish prompt diagnosis and treatment.
CASE REPORT
Twenty-three-year-old male patient with a familiar history of schizophrenia in maternal aunt presented behavioral symptoms, aggressiveness, agitation, visual hallucinations, and generalized seizures without abnormalities in a head computed tomographic (CT) scan, treated with carbamazepine and phenytoin, and no improvement. After a psychiatric assessment, it was resolved to be hospitalized under a diagnosis of schizophrenia.
The patient became febrile, somnolent, agitated, and his Glasgow coma scale (GCS) changed to 12 (O4V3M5). Haloperidol and diazepam were administered to control symptoms. Cerebrospinal fluid (CSF) and blood test turned out inconclusive (Table 1), so bacterial versus viral meningitis was considered, and the patient was started on acyclovir ceftriaxone and azithromycin. Phenytoin and valproic acid were used as anticonvulsive treatments.
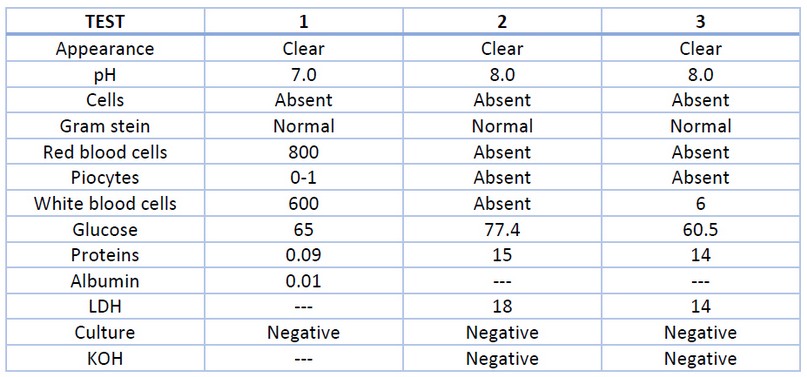
Table 1.- Cerebrospinal fluid test characteristics in the patient.
After eight days of hospitalization, GCS worsened to fluctuate between 11 (O3V2M6) and 7 (O2V2M3), so it was decided to protect the airway and start on mechanical ventilation. Fentanyl and midazolam infusions were indicated. He was transferred to the intensive care unit (ICU) with suspicion of auto-immune encephalitis, and methylprednisolone was initiated (1 gr IV each day for 5 days).
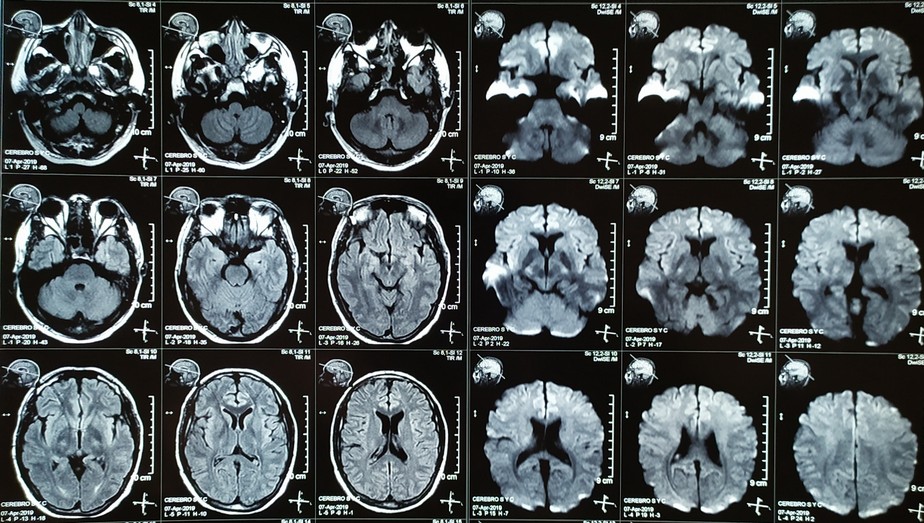
Three days after, the patient presented refractory status epilepticus (RSE), and propofol bolus and infusion were needed to stop it. Levetiracetam was started as the third anticonvulsive drug. A brain magnetic resonance imaging study was performed without abnormalities reported (Figure 1). Blood and CSF tests were carried to rule out herpes simplex brain infection and thyroid and testicular cancers. Nevertheless, the CSF molecular diagnosis lab reported anti-MNDA antibodies, and diagnosis of auto-immune encephalitis was achieved.
Figure 1.- Simple brain MRI with FLAIR (left) and Diffusion (right) sequences without central nervous systems visible alterations.
The patient showed involuntary movements despite sedative infusions, and electroencephalographic (EEG) monitoring was necessary to follow patient evolution. It was negative for persisting status epilepticus.
Plasmapheresis was indicated as the initial treatment, and 5 sessions were carried out according to institutional availability. Sedation was withdrawn while he was on EEG monitoring and GCS improved from 3T (O1V1TM1) to 10T (O4V1TM6) without new seizures. Nevertheless, superior extremities dyskinetic movements continued.
Mechanical ventilation was kept for 15 days due to infectious multi-drug resistant complications (ventilator-associated pneumonia), and tracheostomy and gastrostomy were needed to perform weaning.
ICU length of stay was 23 days, and the patient was discharged to the Neurology department. Hospitalization continued for 37 days more because of healthcare-associated pneumonia. New episodes of agitation and somnolence developed, so a relapse was identified. Second-line drug rituximab was indicated, and a good response was achieved. Agitation control and connection with the environment were accomplished. However, right arm dyskinetic movements persisted.
In the end, discharge and ambulatory follow-up were planned, but the patient didn't return.
DISCUSSION
The case report refers to a young male patient with an initial diagnosis of schizophrenia, who developed a new onset refractory status epilepticus (NORSE), followed by suspicion of auto-immune encephalitis and confirmed by isolation anti-NMDA antibodies in cerebrospinal fluid. He is treated with plasmapheresis as a first approach, showing a slow response and a relapse. Rituximab is chosen as a second-line treatment with complete control of symptoms. Hospitalization of the patient is complicated with healthcare-associated pneumonia for two occasions.
Ecuador doesn't have a database for registry and reports of patients with a diagnosis of auto-immune encephalitis. A UK study reports that auto-immune encephalitis represents 21% of all diagnosed encephalitis; nevertheless, 37% of the encephalitis doesn't achieve an etiology 5. In a Norwegian study, the diagnosis of encephalitis has a known cause in 43% of cases; this is because of the infectious disease focus 6. Numbers point out a difficulty in diagnosing auto-immune encephalitis.
The first description of auto-immune encephalitis was made in 2005 when four young women diagnosed with ovarian teratoma showed psychiatric, neurologic, and respiratory compromise 7. In this regard, our patient was ruled out of possible testicular, thyroid, brain, and lung cancer.
In this case, the diagnosis of auto-immune encephalitis was made by isolation of anti-NMDA antibodies in cerebrospinal fluid. Antibodies against central nervous system cells are classified into 2 groups according to their mechanism of action. Antibodies like Hu-type, Ri-type, anti-fine, Ma2-type, CRMP 5-8-9-10, work against intracellular antigens and are related to paraneoplastic syndromes in lung cancer cases seminomas, and breast cancer. Immune therapy and steroids perform poorly against them, with a bad prognosis. Antibodies against the surface and synaptic proteins like anti-AMPA-GluR3, anti-NMDA-NR1, and anti-NMDA-NR2 can cause encephalic, cerebellar, and epileptic syndromes with a benign evolution and a better response to immune therapy and steroids 8.
Young male patients with auto-immune encephalitis are unusual because anti-NMDA encephalitis is presented with a greater frequency by females in a ratio of 3:1 according to different studies 8,9.
The main symptoms showed by our patient were personality disorders, agitation, and seizures. According to epidemiologic studies, the most frequent sign and symptoms are seizures (88%), personality disorders (69%), fever (56%), headache (50%), and neurologic deficit (50%) (10). The most common neurologic deficits are aphasia (72%), movement disorders (63%), and autonomic dysfunction (47%). Irritability (75%), hallucinations (66%), and psychosis (59%) are the most prevalent psychiatric traces 4,10.
NORSE is not a common feature in auto-immune encephalitis. It is reported that 52% of NORSE cases are cryptogenic, and just 5% are related to anti-NMDA encephalitis 11,12.
Epidemiologic studies have reported cerebrospinal fluid characteristics in auto-immune encephalitis. They have found pleocytosis (>4/ul) in 69% of cases, proteins >0.5 g/l in 44% of cases, and a CSF/serum glucose ratio <0.5 in 27% of cases 10. It was different in our patients.
Viral etiology is the most common cause of encephalitis, so tests for infectious diseases must be performed to rule out them (herpes simplex, varicella-zoster, enterovirus) 10,13. Our patient was negative for herpes simplex. No other test was available to be performed.
Image studies in encephalitis report: head computed tomography (CT), alterations in 17% of cases; brain magnetic resonance imaging (MRI), abnormalities in 25%-46% of cases; and electroencephalographic seizure changes in 81%-88% of cases 10,14. No abnormalities were displayed by head CT scan or brain MRI in the patient in the present report. EEG was not helpful because of NORSE presentation and drugs used for its treatment.
The treatment used in this case were plasmapheresis and rituximab. Case series and expert recommendations state that the first-line treatment for NMDA auto-immune encephalitis is steroids (methylprednisolone 1 g IV per day for 3 to 5 days), immunoglobulin (0.4 g/kg per day for 5 days). As second-line treatments, cyclophosphamide and rituximab are used. In cases related to cancer, surgery is part of the treatment 3,10,12,14,15.
It has been reported that approximately 53-75% of auto-immune encephalitis patients require ICU admission, and 41% precise mechanical ventilation. The hospital length of stay is 89 days as an average 3. In this case report, ICU hospitalization was for 23 days, and the total hospital stay was 60 days.
Our patient follow-up was not possible, so neurologic and functional recovery assessment was not registered. A US multicenter observational study in 577 patients found that early treatment and no-UCI admission was related to good prognosis (OR 0.62, CI 0.50–0.76; p<0.0001; OR 0.12, CI 0.06–0.22; p<0.0001). After the first month of discharge, patients showed, according to the modified Rankin scale (Table 2), a score of 5 in 86% of cases, 4 in 12%, and 3 in 1%. After the second year, 78% of patients achieved a 0-2, and 6% died 3,16.
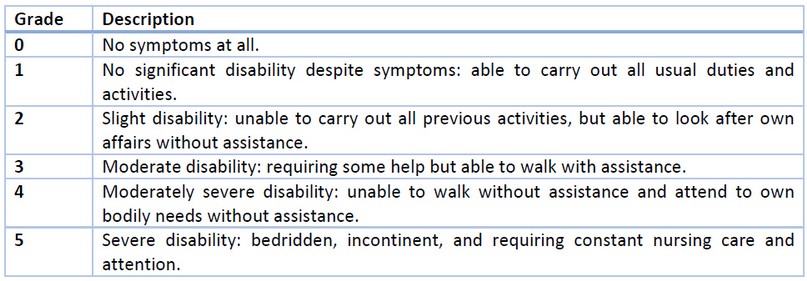
Table 2. Modified Rankin Scale 17.
Limitations found in our case report were that it contains just one case attended in different health institutions, so difficulties were obtaining detailed psychiatric notes. NORSE as part of the patient's symptoms, didn't allow neurologic exploration and EEG record to characterize auto-immune encephalitis because of the need for sedation. And the patient was lost for follow-up.
Strengths, in this case, were early suspicion of auto-immune encephalitis after lack of response in treatment with antibiotics. The possibility of complete plasmapheresis therapy and the availability of rituximab for treatment is not standard therapy used in Ecuador. And the opportunity of confirming the diagnosis with isolation of anti-NMDA antibody because this test is not routinely accessible in the country.
CONCLUSIONS
Anti-NMDA auto-immune encephalitis is a low prevalence disease worldwide, so national reports and follow-up strategies have been created, so etiology, clinical picture, and early diagnosis and treatment are possible. This is not available in low and middle-income countries like Ecuador, so it is necessary to be familiar with the presentation and evolution of these cases to offer an opportunity for recovery. Diagnosis starts in a patient with psychiatric and neurologic symptoms, followed by isolation of antibodies in CSF. First-line treatments are IV immunoglobulins and plasmapheresis. Cyclophosphamide and rituximab are second-line drugs. Functionality recovery is slow and achieved by the second year of discharge. Good prognosis factors are early treatment and no-UCI admission.
REFERENCES
1. Guasp M, Dalmau J. Encefalitis por anticuerpos contra el receptor de NMDA. Med Clínica. 2017;9.
2. Parra JPC, Urra CR, Derio CD. Encefalitis autoinmunes: criterios diagnósticos y pautas terapéuticas. Rev Med Chile. :11.
3. Titulaer MJ, McCracken L, Gabilondo I, Armangué T, Glaser C, Iizuka T, et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol. 2013 Feb;12(2):157–65.
4. Landa E, Alvites M, Fortes J, Pérez M. Psicosis y encefalitis NMDA: reporte de un caso y revisión de la literatura. Rev Clínica Médica Fam. 2014 Sep 8;8(1):4.
5. Granerod J, Ambrose HE, Davies NW, Clewley JP, Walsh AL, Morgan D, et al. Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis. 2010 Dec;10(12):835–44.
6. Quist-Paulsen E, Kran A-MB, Dunlop O, Wilson J, Ormaasen V. Infectious encephalitis: A description of a Norwegian cohort. Scand J Infect Dis. 2013 Mar;45(3):179–85.
7. Vitaliani R, Mason W, Ances B, Zwerdling T, Jiang Z, Dalmau J. Paraneoplastic encephalitis, psychiatric symptoms, and hypoventilation in ovarian teratoma. Ann Neurol. 2005 Oct;58(4):594–604.
8. Torricelli RE. ENCEFALITIS AUTOINMUNES. RECEPTOR ANTI-NMDA Y NUEVOS INMUNOFENOTIPOS. 2019;6.
9. Salazar Reinoso F, Saltos Mata F, Cevallos Plúas J, Romero Santana G. Encefalitis Autoinmune Anti-Receptor NMDA Reporte de Caso Clínico y Revisión de Literatura. Rev Ecuat Neurol. 2020;29(1):165–70.
10. Gable MS, Sheriff H, Dalmau J, Tilley DH, Glaser CA. The Frequency of Autoimmune N-Methyl-D-Aspartate Receptor Encephalitis Surpasses That of Individual Viral Etiologies in Young Individuals Enrolled in the California Encephalitis Project. Clin Infect Dis. 2012 1 April;54(7):899–904.
11. Gaspard N. New-onset refractory status epilepticus. 2015;(5):10.
12. Khoo CS, Zulkifli NH, Rahman SSA. An unusual case of refractory status epilepticus in a young lady: anti-NMDA receptor encephalitis. Clin Med. 2017 Oct;17(5):436–8.
13. Panariello A, Bassetti R, Radice A, Rossotti R, Puoti M, Corradin M, et al. Anti-NMDA receptor encephalitis in a psychiatric Covid-19 patient: A case report. Brain Behav Immun. 2020 Jul;87:179–81.
14. Yang L, Jiang Q, Guan H, Bo H. Nursing care in anti-N-methyl-D-aspartate receptor encephalitis: A case series. Medicine (Baltimore). 2019 Nov;98(46):e17856.
15. Sonneville R, Venkatesan A, Honnorat J. Understanding auto-immune encephalitis in the ICU. Intensive Care Med. 2019 Dec;45(12):1795–8.
16. Kayser MS, Dalmau J. Anti-NMDA receptor encephalitis, autoimmunity, and psychosis. Schizophr Res. 2016 Sep;176(1):36–40.
17. van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJA, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. :4.
Received: 5 April 2021
Accepted: 7 July 2021
Pablo Andrés Llerena-Rengel1, Luis Felipe Villamarín-Granja1, Jorge Luis Vélez-Páez1,2.
1. Universidad Central del Ecuador-Instituto Superior de Posgrado, Quito-Ecuador.
2. Hospital Pablo Arturo Suárez-Unidad de Terapia Intensiva-Centro de Investigación Clínica, Quito-Ecuador.
Autor de correspondencia: Pablo Andrés Llerena-Rengel
Universidad Central del Ecuador-Instituto Superior de Posgrado, Quito-Ecuador
ORCID: https://orcid.org/0000-0003-4446-3042
Luis Felipe Villamarín-Granja
Universidad Central del Ecuador-Instituto Superior de Posgrado, Quito-Ecuador
Jorge Luis Vélez-Páez
Universidad Central del Ecuador-Instituto Superior de Posgrado, Quito-Ecuador
Hospital Pablo Arturo Suárez-Unidad de Terapia Intensiva-Centro de Investigación Clínica, Quito-Ecuador.
ORCID: https://orcid.org/0000-0002-6956-4475