2022.07.02.13
Files > Volume 7 > Vol 7 No 2 2022
The Effects of Sex Hormones and some Respiratory Diseases on the Severity of Corona Virus Infection
Masar J. Jari1, Ghanim A. Abbas2 and Meraim A. Kazaal3*
1 Nursing techniques department, Technical Institute of Al-Diwaniyah, AL-Furat AL Awsat Technical University, Iraq. [email protected]
2 Nursing techniques department, Technical Institute of Al-Diwaniyah, AL-Furat AL Awsat Technical University, Iraq. [email protected].
* Nursing techniques department, Technical Institute of Al-Diwaniyah, AL-Furat AL Awsat Technical University, Iraq . *Correspondence: e-mail: [email protected]
Available from: http://dx.doi.org/10.21931/RB/2022.07.02.13
ABSTRACT
Sex hormones and chronic respiratory diseases play a role in the pathogenesis and the management of Covid-19 infection. Present research tries to shed light on the role of sex hormones, bronchial asthma and lung cancer on the severity of Covid-19 infection and the resulting mortality rate. This study included a follow-up of the health status of 85 patients infected with Covid-19, and all the patients previously diagnosed had hereditary respiratory diseases (bronchial asthma (64) and lung cancer (21)). The serum level of progesterone and testosterone and the stages of lung cancer development were measured in the laboratories of Diwaniyah Teaching Hospital. After conducting medical examinations, computed tomography and x-rays, the severity of Covid-19 infection was classified according to the WHO to moderate, severe and critical infection. The current results showed that most of the hospitalized cases were males (65%) with a death rate (18%), so bronchial asthma was associated with the death rate in males (70% of dead males), followed by postmenopausal (POM) women (66.7% of the dead woman), while pre-menopausal (PRM) women had the highest cure rate (100%). The results of the study showed that the rise in the mean of progesterone in PRM (13.55 ng/ml) was associated with moderate symptoms of Covid-19, while the increased testosterone in males and POM (1018 ng/dL and 67.3 ng/dL, respectively) was associated with an increase in the severity of the infection. In conclusion, asthma and high testosterone directly affected the increase in the severity of Covid-19 and the high mortality rate among the Corona sufferers. While advanced lung cancer had a clear role in that, at the same time, progesterone appeared as a protective factor in young women.
Keywords: Covid-19, bronchial asthma, lung cancer, testosterone, progesterone
INTRODUCTION
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was recognized as the reason for the Covid-19 sickness (Coronavirus) flare-up in Wuhan, China, on 9 January, 2020 1,8,18. Since the World Wellbeing Association proclaimed Coronavirus a pandemic, the quantity of cases has expanded at a dramatic rate. To 2020, there have been 19,369,210 confirmed cases around the world with more than 732,499 deaths 2,3. The novel coronavirus disease 2019 shows a wide range of clinical outcomes as severity and fatality rates. Older populations and health-compromised groups may be at higher risk of getting very sick with Covid-19. Specifically, persons with respiratory diseases, such as lung cancer and bronchial asthma, and individuals in active cancer treatments may be susceptible to a more serious form of the infection 4,5. Accessible information affirm that patients with innate respiratory illnesses as hypersensitivity and malignancy are potentially bound to be tainted by SARS-CoV-2 and, all the more critically, absolutely inclined to foster extreme difficulties characterized here as confirmation in an emergency unit 5, the requirement for mechanical ventilation (MV) or demise because of Coronavirus. As of late, a few investigations have proposed conceivable non-hurtful impacts of asthma on the clinical results of Coronavirus yet a review concentrate by Zhao et al., assessed the danger factors among 548 Coronavirus inpatients in Wuhan and announced that there were not many patients with asthma and the danger was steady with severe Coronavirus cases 6,7.
On the other hand, Disease patients and malignancy survivors address a weak populace for Coronavirus. Generally, the pervasiveness of Coronavirus in malignancy patients is assessed at 6% and is higher than in the non-disease populace. Besides, malignancy patients have more awful results from Coronavirus, upheld by past reports from China 8,9,10 , Italy 11, and all the more as of late New York 12. Hazard of solemn occasions characterized as admission to the ICU, the requirement for MV or demise is accounted for up to 39% of patients with the disease, and death rate could be just about as high as 30% 9.
Patients with the cellular breakdown in the lungs and hematological malignancies appear to be at the most elevated danger of death from SARS-CoV-2 infection.6 as opposed to hematologic malignancies, significantly immunosuppressive treatment isn’t regular in the cellular breakdown in the lungs 13. Sex hormones and associated comorbidities can play a role in the pathogenesis and the management of Covid-19 infection. Sex hormones, such as estradiol, progesterone, and testosterone, might concern the age-dependent and sex-specific severity of Covid-19. According to several studies, men have higher Covid-19-related morbidity and mortality rates than women 14, 15. The severity of Covid-19 is associated with various comorbidities. However, not adequate studies have yet demonstrated the potential risk of respiratory failure and mortality in Covid-19 patients with pre-existing asthma or lung cancer; therefore, the current study aimed to detect the role of inherent bronchial asthma and lung cancer in the severity of Covid-19 infection and the resulting mortality rate. Additionally, this article investigates the possible master/calming impacts of progesterone and testosterone during Coronavirus disease, with specific consideration regarding the expected restorative job of chemical substitution treatment in people with Coronavirus.
MATERIALS AND METHODS
The current study included a follow-up of the health status of 85 hospitalized cases infected with Coronavirus in Al- Diwaniyah Teaching Hospital during the period from 6/8/2020 to 5/2/2021. In addition, the present study was in agreement with the ethics of Al- Diwaniyah Teaching Hospital and verbal informed consent were obtained from all participants. The patients’ ages ranged from 18-65 years, and the inclusion criteria as all patients were positive for Covid-19, the patients had the respiratory disease (bronchial asthma or lung cancer) and were not smokers, patients had a positive family history of bronchial asthma or lung cancer, age range from 18-65 year and determined the menstruation of females.
Hormone level measurement: after blood collection, centrifuging preform for serum preparation. serum concentration of progesterone and testosterone measured by routine protocol of hormone assay analyzer in chemistry lab.
Diagnosis of respiratory disorders: the present study included only Covid-19 infected patients who have bronchial asthma or lung cancer. Identification of Covid-19 infection detected by enzyme-linked immunosorbent assay and real-time polymerase chain reaction in a virology lab. After conducting medical examinations, computed tomography and x-rays, the severity of Covid-19 infection was classified according to the World Healthcare Organization (WHO) as moderate, severe and critical infection 16. Asthmatics were previously diagnosed with chronic inherent respiratory disorder by respiratory disease specialists. Moreover, Lung cancer patients are pre-diagnosed and receive treatment, and the stages of cancer are known to some of them, while this has been determined for others in the Histopathology lab according to American Cancer Society 17.
Statistical analysis: Statistical Package for Social Sciences version 20 (SSPS20) computer software and Microsoft Dominate 2010 were dependent on measurable Investigation and just outcomes that had a P esteem <0.05 were considered statically huge 25,35.
RESULTS
The current study aims to monitor the health status of MERS-CoV patients with bronchial asthma or lung cancer as a model for chronic respiratory diseases that could play a role in infection severity, response rate to treatment, or death. Patients’ ages ranged from 18-65 years; younger patients were excluded, while we did not reach older patients during the current study period. In addition, the results showed that more males than females stayed in the hospital (55 and 30, respectively) with a mean age ± standard deviation of 38.20±3.68 years and 34.13 ± 5.61 years for males and females, respectively, as in table (1) so no significant differences were found when comparing the average ages of both sexes (P= 0.471). The studied samples showed that Covid-19 infected elderly people increase the rate of their stay in the intensive care unit, especially in males when the highest percentage of infected males and females appeared within the age group of 47-65 years (45% and 40% respectively) followed by the age group from 31-46 years (31% and 37% respectively) However, there were no statistical differences in the distribution of females and males according to the mentioned age groups (P>0.05) as explained in the table (1).
On the other hand, females were divided into two groups according to the menstruation to determine the extent of the impact of hormonal changes on the severity of infection. The percentage of pre-menopause (PRM) women appeared to be 60%, and post-menopause (POM) by 40% of the total number of women (figure 1).
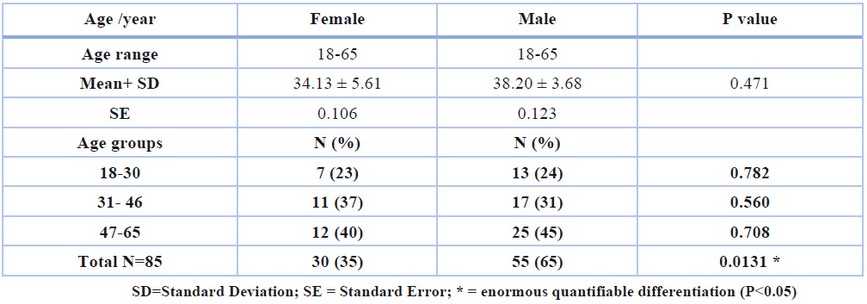
Table 1. Distribution of Covid-19 patients with bronchial asthma or lung cancer over gender and age
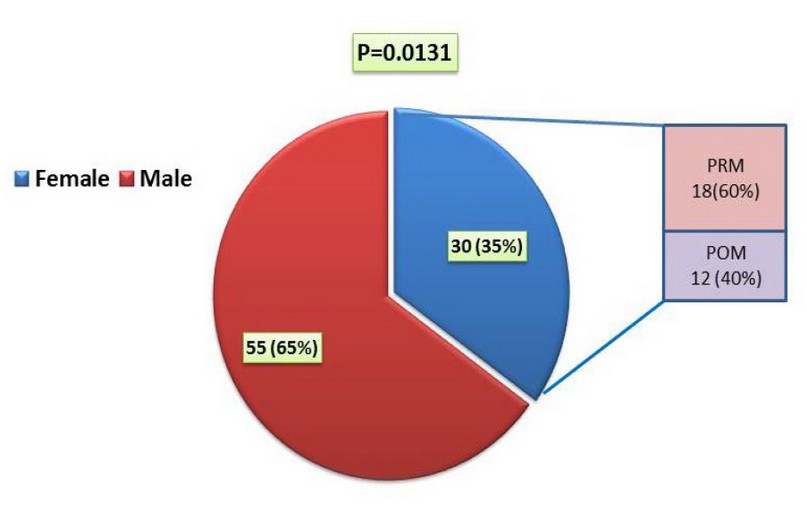
Figure 1. Distribution of Covid-19 infected according to gender. PRM=Pre menopause, POM=Post menopause
The current study included knowledge of the relationship between the effect of bronchial asthma and lung cancer on the severity of infection with the Coronavirus, as 64 Covid-19 patients (75%) had bronchial asthma of these, 42%, 36% and 22% have severe, moderate and critical infection respectively as in table 2 and figure 2. On the other hand, the percentage of Covid-19 patients and those with lung cancer accounted for 25% (21 patients), and a large percentage of them suffered from severe infection (43%), and 33% had a moderate infection, while 24% have an acute infection.
The mortality rate during the present survey was 10 males (7 asthmatics and 3 have lung cancer), and 3 women (2 asthmatics and 1 lung cancer) are dead, while all the young women recovered (Table 3). Moreover, the results in figure (3) also showed that the severity of the infection increases with the progression of cancer, as 75% of cancer patients in the IV stage were distressed from critical Covid-19 infection, and this was reflected in the death of 2 males and 1 female infected with Covid-19 in this cancer stage so 50% of patient in III cancer stage have severed Covid-19 infection. However, the number of deaths among males (18%) was more than that of females (10%), and the death rate mainly appeared among POM women and older males within the age group of 47-65 years ( 25% and 28% for POM woman and males respectively) as shown in the table (4).
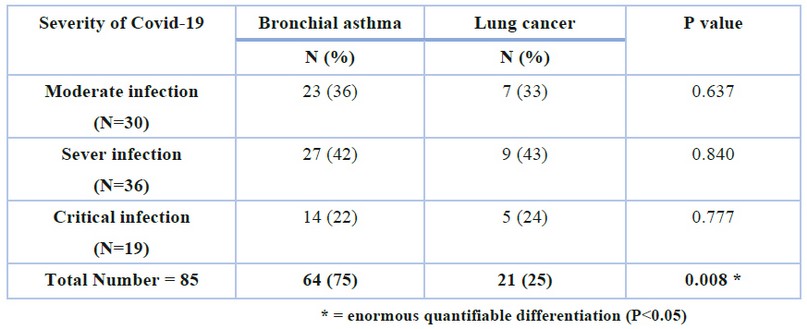
Table 2. The effect of bronchial asthma and lung cancer on the severity of Covid-19 infection
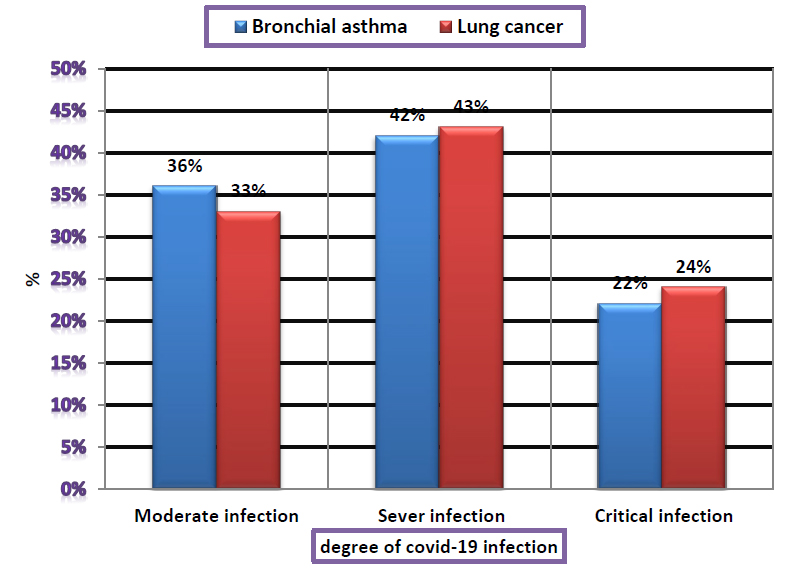
Figure 2. Frequency of Covid-19 infection among asthmatic and lung cancer patients
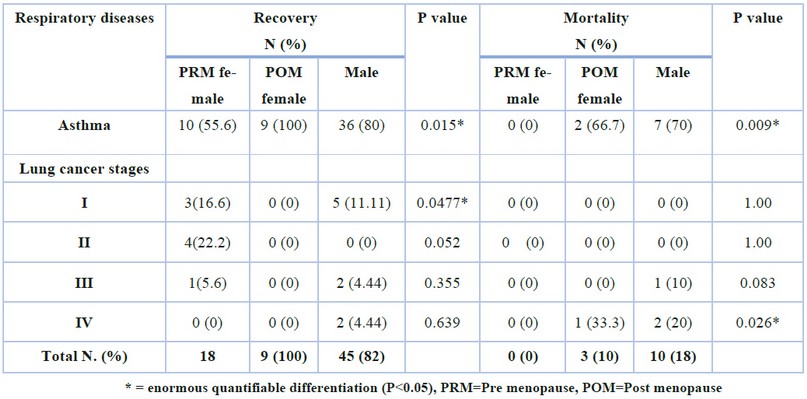
Table 3. The effect of bronchial asthma and lung cancer on the mortality and recovery rate among patients with Covid-19
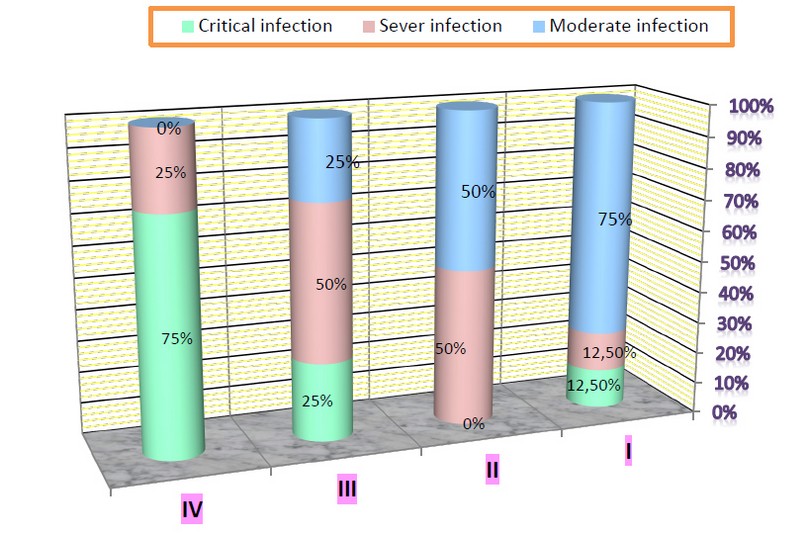
Figure 3. Distribution of lung cancer stages according to severity of Covid-19 infection
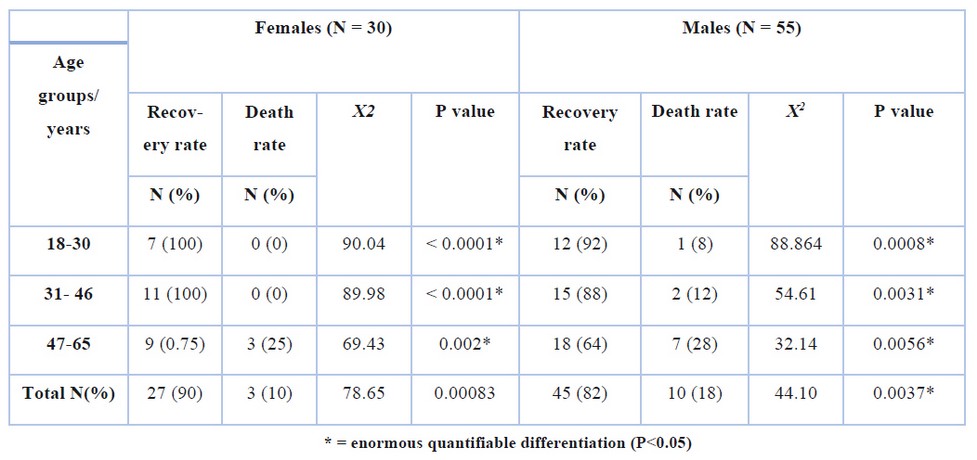
Table 4. The effect of patients ’age on the rates of cure and mortality
Table (5) showed the effect of gender and maturity on the severity of Covid-19, as a straightforward percentage of males and POM women suffered from severe infection (42% and 58%, respectively), while most PRM women have a moderate infection (61%). While high rates of acute infections were 27%, 25% and 6% for males, POM and PRM women, respectively, this was accompanied by significant differences in the moderate and severe infections among the studied groups (P<0.05).
The current results also showed an expansion in the Coronavirus severity and symptoms with an increase in the male hormone testosterone, especially in males and POM women, compared to PRM women, where the mean testosterone in the Covid-19 infection was 871 ng/dL, 22.0 ng/dL and 20.5 ng/dL for males, POM and PRM women respectively (P=0.041). On the other hand, in severe infections was 995 ng/dL, 36.7 ng/dL and 27.72 ng/dL for males, POM and PRM women, respectively (P=0.048), while the serum means of testosterone in acute infections was 1018 ng/dL, 67.3 ng/dL and 50.16 ng/dL for males, POM and PRM women respectively (P=0.039)as shown in table (6). While the effects were different in the case of progesterone hormone in females, whose high concentration in the blood was accompanied by moderate symptoms and signs of Coronavirus in females (especially PRM women) as shown in table (7) when the mean progesterone in the moderate Covid-19 infection was 0.03ng/ml, 0.037ng/ml and 13.55ng/ml for males, POM and PRM women respectively (P=0.036). Moreover, in severe infections was 0.015ng/ml, 0.022ng/ml and 10.14 ng/ml for males, POM and PRM women respectively (P=0.022), while the serum mean of progesterone in critical infections was 0.012ng/ml, 0.021ng/ml and 8.36ng/ml for males, POM and PRM women respectively (P=0.009)
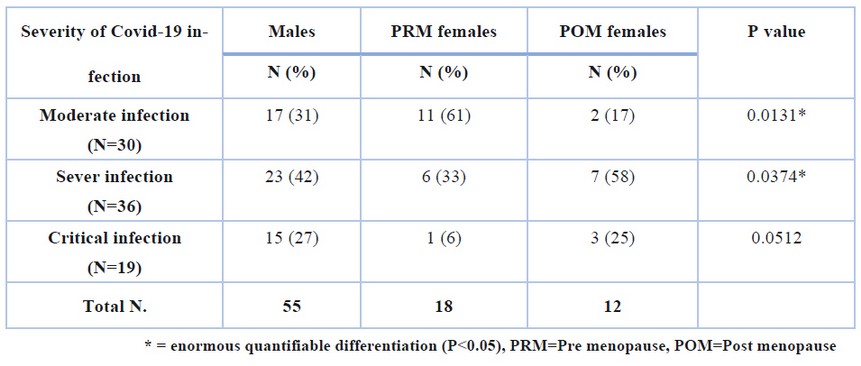
Table 5. The effect of gender and menstruation on the severity of Covid-19 infection
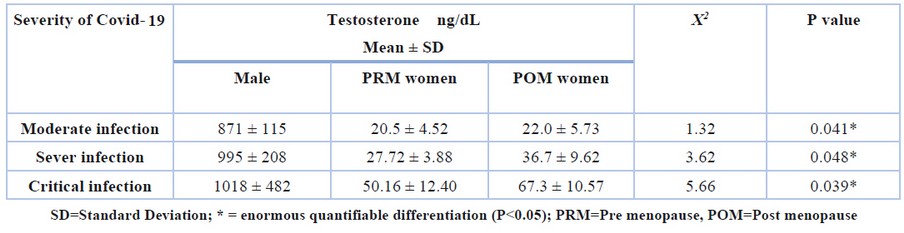
Table 6. Mean serum testosterone level according to Severity of Covid-19 among patients with respiratory disorders
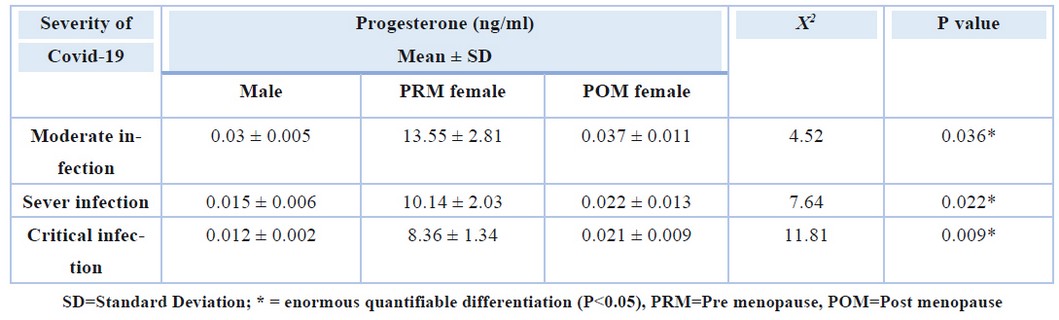
Table 7. Mean of serum Progesterone level according to Severity of Covid-19 among patients with respiratory disorders
DISCUSSION
The growing statistics support the notion that gender and older age are associated with a significantly higher risk of severe health deterioration and death from covid-19 18,19,20. The current study showed that the severity of infection with the Coronavirus is more among the males and POM females than in PRM females, and the severity of the infection and the number of deaths increases with age, and this result is similar to many previous studies of different countries. Of the 1591 patients admitted to ICU in the Lombardy region, Italy, 82% were male 21. Another Canadian study analyzed over 200,000 residents tested for SARS-CoV-2; although only 36% of individuals tested were males, compared with women, they showed higher rates of laboratory-confirmed infection (13.5% vs. 9.8%), hospitalization (15.6% vs. 10.4%), ICU admission (4.1% vs. 1.7%), and death (8.7% vs. 7.6%) 22. Several other reasons have also been suggested to elucidate the gender disparity in Covid-19, like the differential habit of smoking and drinking, sociological, psychological factors, and therefore the differential profile of comorbidities among sexes 23. In contrast to our study, studies conducted in South Korea showed that Covid-19 was the foremost prevalent in women within the 20-39 years age bracket. This finding was also observed in another study using data reported to the Korea Centers for Disease Control and Prevention 24,25.
Our study showed that the most common hereditary respiratory disease among people with Coronavirus is bronchial asthma (75%), and its coincidence with the Covid-19 increased the severity of infection and incidence of death. Two studies about asthmatic patients with Covid-19 in South Korea using insurance Review and Assessment database were recently published. The first study by Yang et al. analyzed the entire cohort who underwent Covid-19 testing and reported that non-allergic asthma patients showed a greater risk of susceptibility to Covid-19 infection and severe clinical outcomes of Covid-19, like ICU admission, application of mechanical ventilation, or death 26. The second study of Choi et al. also reported higher mortality in asthmatic patients than in non-asthmatic patients among Covid-19 patients 27,49.
Present data in same line with several previous studies that recorded cancer patients, mainly lung cancers, experience disproportionately severe illness and deaths from Covid-19 28,29. Lung cancer is characterized by a clinical scenario of increased risk of pulmonary complications, acute lung injury, and high incidence of Covid-19 infection due to pathophysiological, clinical and treatment-related risk factors. So, in the current study, the death rate for lung cancer patients with Coronavirus was 19% (4/21), and most of them had advanced stages (IV or III stages) of cancer. In contrast, in other studies, the mortality rates in patients with cancer have been recorded between 25%-30% 30,31, which has mentioned a high interaction between causes frequently associated with lung cancer, including smoking-related lung damage or disorder, major cardiovascular and respiratory diseases, and elderly age which is associated with increased severity of SARS-CoV-2 infection 31,32. Another study from Memorial Sloan Kettering Cancer Center was done on a cohort of 423 cancer patients with Covid-19 (including 8% lung cancer patients) and detected that 20% had severe respiratory disorders (involving 9% with mechanical ventilation) 12% died during 30 days. Furthermore, the researchers determined that given immuno-therapy was correlated with more risk of health problems. Newly published data from current work and previous research showed that stage IV non-small cell lung cancer patients are at greater risk of health complications and death if infected with SARS-CoV-2 33,34.
In the existing study, changes in the level of sex hormones in the blood were linked to changes in the severity of infection. According to the current study, high progesterone may have a role in the recovery of all PRM women. At the same time, the decline of this hormone and the rise of the hormone testosterone may play a role in the severity of Covid-19 and death among men and women after menopause. In previous mice models, female hormones had a protective effect on mortality related to SARS-CoV infection 15. McCoy et al. suggested that androgens, which may play an essential role in SARS-CoV-2 entry into the host cell, were implicated in Covid-19 mortality 34. A study in Korea showed that male sex was not an independent risk factor for mortality, and there was no significant association between hormone therapy use and the clinical outcomes of peri- and postmenopausal women. Cattrini et al Showed that high testosterone levels could upregulate transmembrane serine protease 2, facilitating the entry of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) into host cells via angiotensin-converting enzyme 2 (ACE2)35. Information from patients with prostate disease treated with androgen-hardship treatment appears to affirm this theory.
Androgens, for the most part, smother the provocative reactions by diminishing the action of the fringe blood mononuclear cells, just as the arrival of incendiary components and cytokines, for example, interleukin-1β, interleukin-2, cancer rot factor-α, inducible nitric oxide synthase, and nitric oxide 36,37,38. They can likewise advance the creation of suppressive cytokines, for example, interleukin-10 and the changing development factor-β through the androgen receptor flagging 38,39,40. Furthermore, androgens are remembered for the thymic involution after adolescence 41; thymic involution decreases the fare of lymphocytes towards the fringe and lessens the capacity of fringe immune system microorganisms and the collection of white blood cells receptors. It isn’t shocking that high testosterone levels have been related to a helpless infection-killing movement after flu inoculation 42. These immunosuppressive impacts of androgens may advance SARS-CoV-2 contamination; however, they may likewise hinder the cytokine storm that describes the most extreme instances of Coronavirus.
An Italian review of 31 male patients conceded to ICU found that lower testosterone plasma levels anticipated more terrible results, supporting a good job of androgens during SARS-CoV-2 contamination 43. A German review revealed that fundamentally sick male patients with Coronavirus experienced serious testosterone, and dihydrotestosterone lacks 44. Another Chinese review showed that the proportion of testosterone to luteinizing hormones was altogether diminished in patients with Coronavirus 45. This information supports the thought that decreased testosterone level in prior or conceivably infection instigated hypogonadism may be related to unfavorable anticipation in Coronavirus 46. In outline, it remains hazy right now whether androgens may be great or horrible during SARS-CoV2 disease 35.
As recently revealed, estrogens were observed to be urgent to shield female mice from SARS-CoV disease 47. The perception that ladies with Coronavirus show better results than men and that postmenopausal ladies are those at a greater danger of extreme Coronavirus is steady with the likelihood that progesterone advances mitigating reactions and can support the slanting of CD4+ White blood cell from TH1-type towards TH2-type reactions 14,48. It has been suggested that an insusceptible framework inclined to a TH2-type reaction, for example, in patients with asthma, may ensure against serious Coronavirus 49. Likewise, progesterone includes an insufficient glucocorticoid and mineralocorticoid action. Considering that steroidal treatment is valuable and is utilized in clinical practice for a couple of cases of serious Coronavirus 50, the enactment of the steroid receptor by progesterone may add to relieve extreme insusceptible reactions 51,52.
CONCLUSIONS
The current study supported the results of previous studies on the increase in the severity of Covid-19 infection with age, especially among males and postmenopausal women who show high testosterone levels accompanied by an increase in disease symptoms, while a therapeutic role for progesterone has also appeared in reducing the risk of the Covid-19 in PRM women. The current study also showed that Covid-19 poses a challenge for people who suffer from respiratory diseases related to the family, as the proportion of hereditary bronchial asthma increases among males and has played a clear role in raising the death rate of Covid-19 patients. On the other hand, the advanced stages of lung cancer were similar to that. Moreover, We hope that there will be subsequent studies on a greater number of participants for a more extended period to clarify the effect of sex hormones on the extent of individuals’ susceptibility to infection with the Coronavirus, in addition to studying the effect of these hormones as a successful treatment to reduce the risk of infection. Also we recommend, through the current study, patients with bronchial asthma and lung cancer to take all health precautions to avoid the occurrence of Covid-19 infection.
Author Contributions:
Meraim A. Kazaal: Conceptualization, Methodology, Software, Data curation, Writing- Original draft preparation, Investigation. Ghanim A. Abbas: Supervision. Masar J. Jari: Visualization, Validation, Writing- Reviewing and Editing . All authors have read and agreed to the published version of the manuscript
Funding: This research received no external funding
Institutional Review Board Statement:
Ethical Clearance: The ethical research committee at scientific research by ethical approval of both environment and health and higher education and scientific research ministries in Iraq. CONFLICT OF INTEREST the authors declare that they have no conflict of interest. Informed Consent Statement: Informed consent was obtained from all subjects involved in the study.
Acknowledgments: we extend our thanks and gratitude to all Covid-19 patients who cooperated with us to collect samples and conduct tests. We also thank the medical and nursing staff at Al-Diwaniyah General Hospital for their assistance in completing the current study.
Conflicts of Interest: The authors declare no conflict of interest.
REFERENCES
1. Organization, W. H. Coronavirus disease (COVID-19) Situation report. 2020. https ://www.who.int/docs/defau lt-sourc e/coron aviru se/situa tion-repor ts/20200 811-covid -19-sitre p-204.pdf?sfvrs n=1f438 3dd_2.
2. Impact of comorbid asthma on severity of coronavirus disease (COVID‑19). Scientific Reports | (2020) 10:21805 | https://doi.org/10.1038/s41598-020-77791-8.
3. Garg, S.; Kim, L.; Whitaker, M.; et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 – COVID-NET. MMWR Morb Mortal Wkly Rep. 2020, 69: 458–464.
4. Butler, M.W.; O’Reilly, A.; Dunican, E.M.; et al. Prevalence of comorbid asthma in COVID-19 patients. J Allergy Clin Immunol 2020, 146: 334–335.
5. Zhou F., Yu T., Ronghui Du, et al. (2020).Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet, 395:1054–1062.
6. Matsuyama, S.,; Kawase, M.; Nao, N.; et al. The inhaled corticosteroid ciclesonide blocks coronavirus RNA replication by targeting viral NSP15. bioRxiv 2020, 106:1-10.
7. Li, X.; Xu, S.; Yu M.; et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J. Allergy Clin. Immunol. 2020,146(1):110-118.
8. Liang, W.; Guan W.; Chen, R.; et al.Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncology2020, 21:335–7.
9. Xu, Z.; Shi, L.; Wang, Y. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020, 8:420–422.
10. Dai, M.; Liu, D.; Liu, M.; et al. Patients with cancer appear more vulnerable to SARS-COV-2: a multi-center study during the COVID-19 outbreak. Cancer Discovery2020, 10:783–91.
11. Fratino, L.; Procopio, G.; Di Maio, M.; et al. Coronavirus: Older Persons With Cancer in Italy in the COVID-19 Pandemic. Front Oncol.2020, 10:648.
12. Miyashita, H.; Mikami, T.; Chopra, N.; et al. Do patients with cancer have a poorer prognosis of COVID-19? An experience in New York City. Ann Oncol. 2020, 31:1088–89.
13. Passaro, A.; Bestvina, C.; Velez, M.V.; et al. Severity of COVID-19 in patients with lung cancer: evidence and challenges. J Immunother Cancer. 2021; 9(3): e002266.
14. Channappanavar, R.; Fett, C.; Mack, M.; et al..Sex-based differences in susceptibility to severe acute respiratory syndrome coronavirus infection. J Immunol 2017, 198:4046–4053.
15. McCoy, J.; Wambier, C.G.; Vano-Galvan, S.; et al. Racial variations in COVID-19 deaths may be due to androgen receptor genetic variants associated with prostate cancer and androgenetic alopecia. Are anti-androgens a potential treatment for COVID-19? J Cosmet Dermatol.2020, 19:1542–1543.
16. WHO. Clinical Management of Covid-19—Interim Guidance. Available online: https://www.who.int/Publications/i/item/clinical-management-of-covid-19 (accessed on 29 June 2020)
17. Cancer Staging. American Cancer Society website. https://www.cancer.org/treatment/understanding-your-diagnosis/staging. Revised 18 June, 2020. Accessed 12 February, 2021.
18. Richardson, S.; Hirsch, J.S.; Narasimhan, M.; et al. Presenting Characteristics, Comorbidities, and Outcomes among 5700 Patients Hospitalized with COVID-19 in the New York City Area. JAMA.2020, 323: 2052-2059
19. Onder, G.; Rezza, G.; Brusaferro, S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA.2020, 323(18):1775-1776.
20. Guan W.J.; Ni, Z.Y.; Hu, Y.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Eng. J. Med.2020, 382:1708–1720.
21. Grasselli, G.; Zangrillo, A.; Zanella, A.; et al. Baseline Characteristics and Outcomes of 1591 Patients Infected with SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA.2020, 323 (16): 1574-1581.
22. Stall, N.M.; Wu, W.; Lapointe-Shaw, L.; et al. Sex- and age-specific di_erences in COVID-19 testing, cases and outcomes: A population-wide study in Ontario, Canada. J. Am. Geriatr. Soc.2020, 68(10):2188-2191.
23. Wenham, C.; Smith, J.; Morgan R. COVID-19: The gendered impacts of the outbreak. Lancet 2020, 395:846–848.
24. Kim, L.; Kim, J.A.; Kim S. A guide for the utilization of health insurance review and assessment service national patient samples. Epidemiol Health 2014, 36:e2014008.
25. Dudley, J.P.; Lee, N.T. Disparities in age-specific morbidity and mortality from SARS-CoV-2 in China and the Republic of Korea. Clin Infect Dis.2020, 71:863–865.
26. Yang, J. M.; Koh H.Y.; Moon S.Y.; et al. Allergic disorders and susceptibility to and severity of COVID-19: A nationwide cohort study. J. Allergy Clin. Immunol.2020, 146(4):790-798
27. Choi, Y. J.; Park, J.; Lee, H. S.; et al. Effect of asthma and asthma medication on the prognosis of patients with COVID-19. Eur. Respir. J.2020, https ://doi.org/10.1183/13993 003.02226 -2020.
28. Palmieri, C.; Turtle, L.; Docherty, A.; et al.1670O prospective data of first 1,797 hospitalised patients with cancer and COVID-19 derived from the COVID-19 clinical information network and international severe acute respiratory and emerging infections Consortium, who coronavirus clinical characterisation Consortium. Ann Oncol.2020, 31:S992–S973.
29. Kuderer, N.M.; Choueiri, T.K.; Shah, D.P.; et al. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet 2020, 395:1907–18.
30. Zhang, L.; Zhu, F.; Xie, L.; et al.. Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann Oncol.2020, 31(7):894-901.
31. Saini, K.S.; Tagliamento, M.; Lambertini, M.; et al. mortality in patients with cancer and coronavirus disease 2019: a systematic review and pooled analysis of 52 studies. Eur J Cancer.2020,139:43 -50.
32. Luo, J.; Rizvi, H.; Preeshagul, I.R.; et al. COVID-19 in patients with lung cancer. Ann Oncol.2020, S0923-7534(20)39894-X.
33. Oh W.K. COVID-19 infection in cancer patients: early observations and unanswered questions. Ann Oncol. 2020;31(7):838–839.
34. Calles, A.; Aparicio, M.I.; Alva, M.; et al. Outcomes of COVID-19 in Patients With Lung Cancer Treated in a Tertiary Hospital in Madrid. Front Oncol. 2020, 16,10:1777.
35. Cattrini, C.; Bersanelli, M.; Latocca, M.; et al. Sex Hormones and Hormone Therapy during COVID-19 Pandemic: Implications for Patients with Cancer, Cancers 2020, 12(2325): 1-13
36. Klein, S.L.; Flanagan K.L. Sex differences in immune responses. Nat. Rev. Immunol.2016, 16: 626–638.
37. Musabak, U.; Bolu, E.; Ozata, M.; et al. Gonadotropin treatment restores in vitro interleukin-1beta and tumour necrosis factor-alpha production by stimulated peripheral blood mononuclear cells frompatients with idiopathic hypogonadotropic hypogonadism. Clin. Exp. Immunol.2003, 132:265–270.
38. D’Agostino, P.; Milano, S.; Barbera, C.; et al. Sex hormones modulate inflammatory mediators produced by macrophages. Ann. N. Y. Acad. Sci.1999, 876:426–429.
39. McKay, L.I.; Cidlowski, J.A. Molecular control of immune/inflammatory responses: Interactions between nuclear factor-kappa B and steroid receptor-signaling pathways. Endocr. Rev.1999, 20:435–459.
40. Liva, S.M.; Voskuhl R.R. Testosterone acts directly on CD4+ T lymphocytes to increase IL-10 production. J. Immunol.2001, 167, 2060–2067.
41. Trigunaite, A.; Dimo, J.; Jørgensen T.N. Suppressive effect of androgens on the immune system. Cell. Immunol.2015, 294:87–94.
42. Furman, D.; Hejblum, B.P.; Simon, N.; et al. Systems analysis of sex differences reveals an immunosuppressive role for testosterone in the response to influenza vaccination. Proc. Natl. Acad. Sci. USA.2014, 111, 869–874.
43. Rastrelli, G.; Di Stasi, V.; Inglese F.; et al. Low testosterone levels predict clinical adverse outcomes in SARS-CoV-2 pneumonia patients. Andrology 2020, 9(1):88-98.
44. Schroeder, M.; Tuku, B.; Jarczak, D.; et al. The majority of male patients with COVID-19 present low testosterone levels on admission to Intensive Care in Hamburg, Germany: A retrospective cohort study. medRxiv 2020, doi: https://doi.org/10. 1101/2020.05.07.20073817
45. Ma, L.; Xie, W.; Li, D.; et al. Effect of SARS-CoV-2 infection upon male gonadal function: A single center-based study. medRxiv.2020, doi: https://doi.org/10.1101/ 2020.03.21.20037267
46. Dutta, S.; Sengupta P. SARS-CoV-2 and Male Infertility: Possible Multifaceted Pathology. Reprod. Sci.2020, 2-4.
47. Stelzig, K.E.; Canepa-Escaro, F.; Schiliro, M.; et al.. Estrogen regulates the expression of SARS-CoV-2 receptor ACE2 in di_erentiated airway epithelial cells. Am. J. Physiol. Lung Cell. Mol. Physiol.2020, Published Online:04 JUN 2020https://doi.org/10.1152/ajplung.00153.2020.
48. Piccinni, M..P.; Giudizi, M.G.; Biagiotti, R.; et al. Progesterone favors the development of human T helper cells producing Th2-type cytokines and promotes both IL-4 production and membrane CD30 expression in established Th1 cell clones. J. Immunol.1955, 155: 128–133.
49. Liu, S.; Zhi, Y.; Ying, S. COVID-19 and Asthma: Reflection during the Pandemic. Clin. Rev. Allergy Immunol.2020, 59(1):78-88.
50. Alhazzani, W.; Møller , M.H.; Arabi, Y.M. Surviving Sepsis Campaign: Guidelines on the Management of Critically Ill Adults with Coronavirus Disease 2019 (COVID-19). Crit. Care Med.2020, 46:854–887.
51. Von Langen, J.; Fritzemeier, K.H.; Diekmann, S.;Hillisch A. Molecular basis of the interaction specificity between the human glucocorticoid receptor and its endogenous steroid ligand cortisol. Chembiochem 2005, 6: 1110–1118.
52. Gordon, D.E.; Jang, G.M.;Bouhaddou, M., et al. A SARS-CoV-2 protein interaction map reveals targets for drug repurposing. Nature 2020, 583: 459–468.
Received: 28 November 2021 / Accepted: 8 December 2021 / Published:15 May 2022
Citation: Masar, J. J,.; Ghanim, A. A.; and Meraim, A. K.; The Effects of Sex Hormones and some Respiratory Diseases on The Severity of Corona Virus Infection. Revis Bionatura 2022;7(2) 13. http://dx.doi.org/10.21931/RB/2022.07.02.13
