2020.05.02.12
Files > Volume 5 > Vol 5 No 2 2020
REVISION/REVIEW
The epidemiological plateau of Corona virus in Gulf countries: a descriptive statistics study
Raghad S. Mouhamad1, Khlood Abedalelah Al-Khafaji 1 Risala H. Allami2, Michael Alabboud3, Maha Hameed Abdulla2, Mohammed M. Jafaar1
Available from: http://dx.doi.org/10.21931/RB/2020.05.02.12
ABSTRACT
The novel SARS-CoV-2 belongs to the beta coronaviruses and causes a severe pandemic disease named as COVID-19. In late December 2019. WHO situation reports on 11 March 2020, declared that COVID-19 a pandemic due to its global spread. All Arab countries have reported COVID-19 cases. The confirmed cases of COVID-19 pandemic in Arab gulf countries were reported in the United Arab Emirates, Iraq, Bahrain, Oman, Qatar, Kuwait, and Saudi Arabia, respectively. The fatality case rates in Gulf Countries are less than 1% in Oman, UAE, Kuwait, Bahrain, and Saudi Arabia, yet it hits 7.5% in Iraq. In this manuscript, we try to interpret the pandemic statistically in gulf countries, especially in Iraq. Additionally, the distribution of COVID-19 confirmed cases based on ABO blood groups were investigated. Epidemiological analyses revealed that a decreased risk of infection was attributed to blood group O compared to non-O blood groups, whereas people with the A and A.B. blood groups showed the highest risk for COVID-19 infection. Besides, high risk for diabetes, cardiovascular disease, blood clotting, and interleukin secretion was also related to blood groups in different orders. Accordingly, patients with a specific blood group that are associate with the above diseases should be under strict medical surveillance when infected with COVID-19 to reduce complications and severity. This study provides further confirmation for the previously reported correlation between the ABO blood groups and the susceptibility to COVID-19 infection.
keywords. COVID-19, Blood type, Gulf countries, Epedemic statistics
INTRODUCTION
One of the B- coronavirus was responsible for the last outbreak of pneumonia cases, which recognized in December 2019 in Wuhan, initially the virus named by World Health Organization to a 2019- novel coronavirus (2019-nCoV). Officially WHO called the disease as COVID-19 while the new virus named SARS-CoV-2 by Coronavirus study group. Chinese researchers isolated the virus responsible for COV-19 on 7 January, 2020, and came out to the genome sequence of SARS-CoV-2 1,2,3; it is enveloped non- segmented positive-sense RNA virus with 96.2% identity to a bat CoVRaTG13, whereas it shares 79.5% identity to SARS-CoV. Genome sequence analysis suggests that bat is the natural host of virus origin, and it might transmit to humans via unknown hosts. SARS-CoV-2 could use angiotensin-converting enzyme (ACE2) as a receptor that encoded on lung alveolar epithelial cells and enterocytes of the intestine 4,5,6 just the same for SARS-CoV 7,8,9.
Rapid Spreading of COVID-19 across the world led WHO declaring it a pandemic on 11 March, 2020. As an emerging acute respiratory infectious disease, the virus responsible for COVID-19 secreted out of respiratory tract, spread for distance by small droplets through coughing and sneezing beside direct contact among persons for a low infective dose. 10, 11 The epidemiological investigation suggests that the incubation period is almost 1-14 days, mostly 3-7 days; the virus is contagious during the latency period and high transmissible, especially for the elderly and people with serious diseases. Patients with COV-19 presented common symptoms such as fever, malaise, and dry coughs. However, not everyone who was infected shows the symptoms of the disease. The blood groups and their related antigens might be associate with the immune response against COVID-19.
Additionally, ABO antigens may increase the susceptibility to viral infection12, 13. Blood groups were distributed among the human population and varied across populations and geographical regions. The four blood groups were known for their critical role in blood transfusion. Humans received incompatible blood, powerful naturally-occurring anti-A or anti-B antibodies could cause a blood transfusion reaction, as well as many other diseases, are related to blood groups such as diabetes, cardiovascular disease, viral infections, and interleukin production. Many other criteria other than the virus strain itself may have an influence such as season and temperature, sex and age of patients, blood group, sanitation, and alienating strategies as well as the early discovery of infection by COV-19. Early diagnosed infected persons limited the rate of virus transmission to others, controlling the outbreak and decreased the rate fatality of COVID-19 disease.
The statistical situation for the pandemic
Traditional first confirmed infection in Gulf countries
The Neighboring countries belong to Gulf take their containment measures after the first confirmed case of infection to lessen and prevent the incidence of infections with COVID-19; the origin of first diagnosed COVID-19 will present in the table (1) for Gulf countries. Data presented by WHO for confirmed cases of COVID-19 regarding Arab Gulf countries revealed that Iraq came at the third number of cases at 5-March, keeping forth position till 8 April. While Iraq had the fifth and sixth positions in total confirmed cases at mid of April and 19 April, respectively, the infection situation also, revealed that the total number of confirmed cases at 19 April was bellowed other countries that recorded the first case at the end of February 2020 such as Qatar, Kuwait, and United Arab Emirate. On 28 April- 2020, Iraq became the last position among Gulf countries.
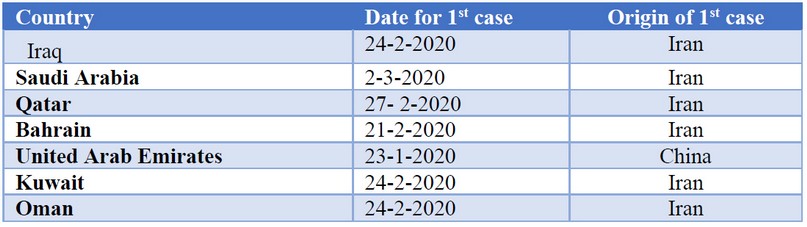
Table 1. The origin of the first confirmed case of COVID-19 at Arab Gulf region
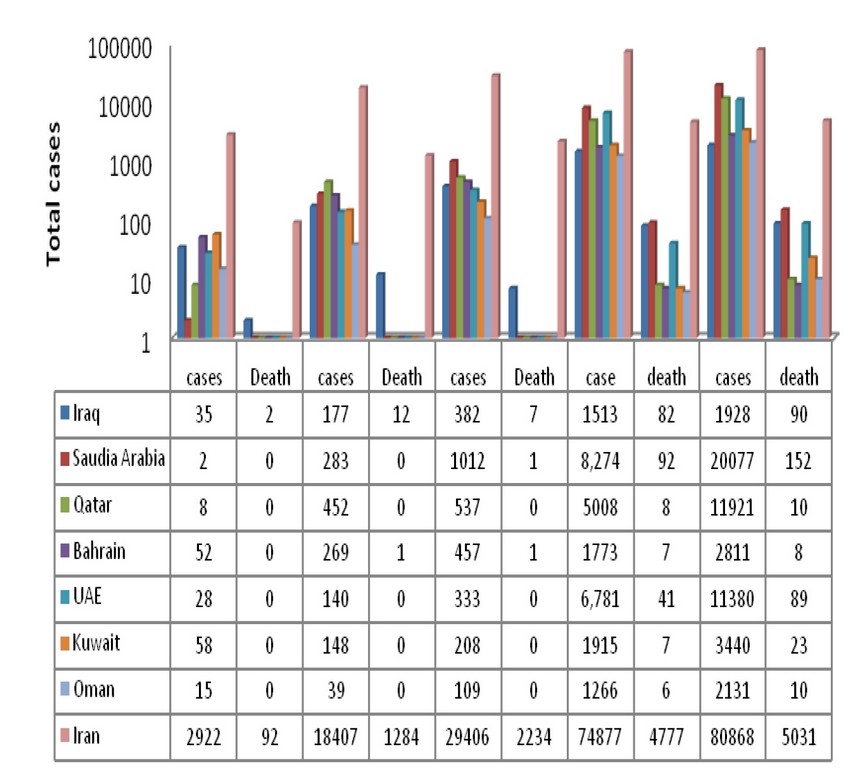
Figure 1. Confirmed cases and Deaths of COVID-19 in Gulf Countries for March- April.
Confirmed cases of COVID-19
COVID-19 regular prevalence data were obtained from the official website between 19 March- April 2020. The charts have been designed to describe the infections in the Gulf area; total cases were analyzed for confirmed infection and deaths in Iraq, Kuwait, Saudi Arabia, UAE, Qatar, and Oman with the first case of infection and its origin. On the other hand, early confirmed the first case in Saudi Arabia began may be the reason for its higher count of cases, as illustrated in figure (1). Many reasons may be attributed to the relatively low incidence of confirmed COVID-19 in the Iraqi population, high temperature (reached to 30-32 in April), prevention of socials aggregation such as Friday prey, religious occasions, closed schools, and Universities. Iraqi hygiene practices were outstanding in streets and houses; they almost wear gloves and masks, wash their hands with soap, shopping with care avoiding aggregation. Other factors may influence infection, such blood group, in which blood group O is more abundant in the Iraqi population; researchers found that individuals with blood group O are more resistant to infections, including SARS and COVID-19. Also, vaccination strategies for the Iraqi population that taken on during past decades; vaccination of BCG and Measles may induce immune responses against COVID-19 infection.
Data collection
COVID-2019 regular prevalence data were obtained from the official website of 14 between 20 January and 18 April 2020. The charts have been extended to a collection of 18 governorates. Figures indicate a growing tendency against the disease network in the total incidence of COVID-2019. There was a persistent rise in the number of reported cases between one-day cases and cases the previous day. The frequency of newly reported cases of COVID-2019 and descriptive statics is evaluated in a detailed review of the results. Also, the pie chart shows the proportion of Iraq confirmed cases who acquired COVID-19 overseas by region, including a category for acquired at traveling, which represents the cases acquired while traveling on visits to religious shrines trips.
The traditional infectious disease prediction model
In February 2020, it was first reported that the ongoing global pandemic was transmitted to Iraq, the first recorded cases of COVID-19 infections were identified in Najaf on 22 February 2020. In Iraq, illness is stigmatized, and many Iraqis are worried not to pursue medical treatment and get screened, which may contribute to inadequate numbers of cases. Quarantine has a certain stigma. Although 0.20 percent of the population of the KRG was checked, just 0.05 percent of the rest of the world was evaluated, and the possible disparity in overall positive statistics in the area and the rest of the nation was then illustrated. The first case was reported on 1 March of COVID-19 infection in Iraqi Kurdistan. The first fatality of the epidemic in Iraq is 3 March. It had been confirmed in the district of Sulaymaniyah.
The number of cases has risen to 67 on 4 March. The following day in Babil and Maysan, two new deaths were recorded. On 14 March, two patients died, on 18 March a death count rose to 12, and 10 new cases were identified, out of 105. Fifty new cases were reported on 24 March. The Ministry of Health has reported that there has been a minimum of 75 recoveries and 27 fatalities. On 25 March, the number of recoveries went up to 89, and 30 new cases were reported. The first case identified in the town of Ishaqi was the Saladin Governorate, thus verifying the virus for the first time in all 18 Iraqi provinces. On 5 April, there is a regular increase of 83 new cases in the number of confirmed cases and, thus, a total of 961, with 279 reported cases. On the same day, five new deaths were also confirmed. Both Baghdad, which saw a rise of 27 and Erbil, the capital of the KRG, which saw an increase of 18 cases, was due to the large increase in the incidents. The cases of Erbil is linked to a prohibited funeral meeting held on 21 and 23 March, which will continue to increase with inquiries and checks. On 15 April, a total of 15 new cases, the lowest in a single day since 21 March, were recorded.
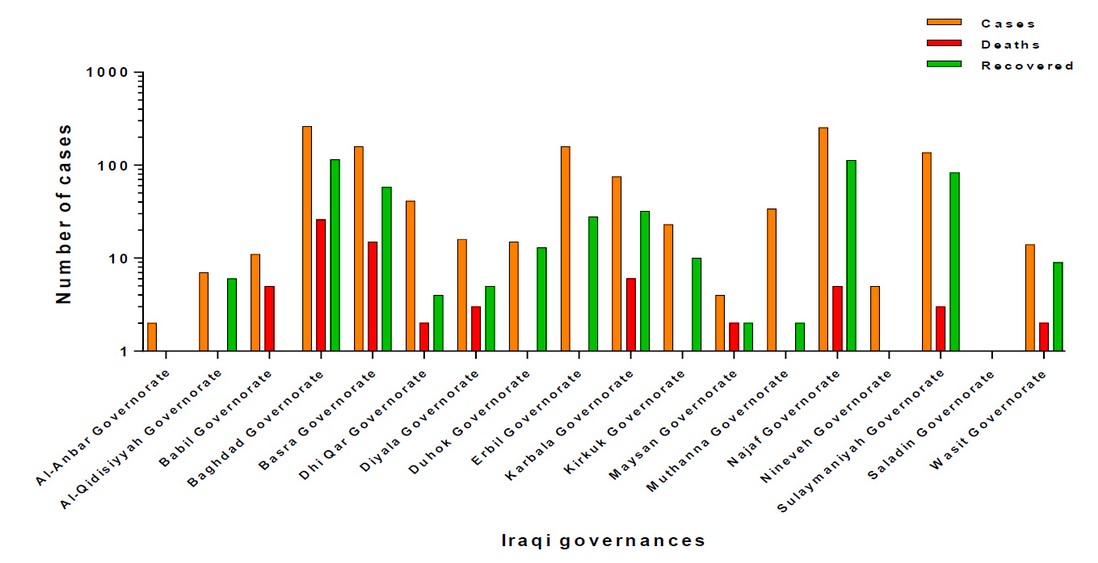
Figure2. Prevalence graph of confirmed cases of COVID-19 in Iraq.
Figure 2, showed that among all areas of Iraq, the number of portable infections, which we find is the largest in Baghdad city 22%, and then Najaf by 21%, while Erbil and Basra share by 13%, and Suleimaniya has risen by 11% and Karbala by 6%. As for the other southern Governorates, it was 3-1% in contrast to the Central Governorates and Kurdistan. Everybody had zero levels of Anbar, Nineveh, Salahuddin, and Maysan. Such percentages are due to the religious visits to central and southern governorates and trade crossings in Iraqi Kurdistan provinces that have been listed above.
In Baghdad’s highest mortality rate, the rate of recovery expressed in the number of cases, accompanied by Najaf’s 23 percent, and Suleimaniya 17 percent, whereas Dohuk also accounted for the lowest mortality level, which was 3 percent, in Kurdistan; That could be attributed to the injured’s age, safety or other causes that we may address later. In Karbala, the 7 percent, and the level for in the regions with maximum rates. The Governorates of Anbar, Saladin, Babil Maysan, and Nineveh had zero recovery rates it’s the same infection case. (figure 3).
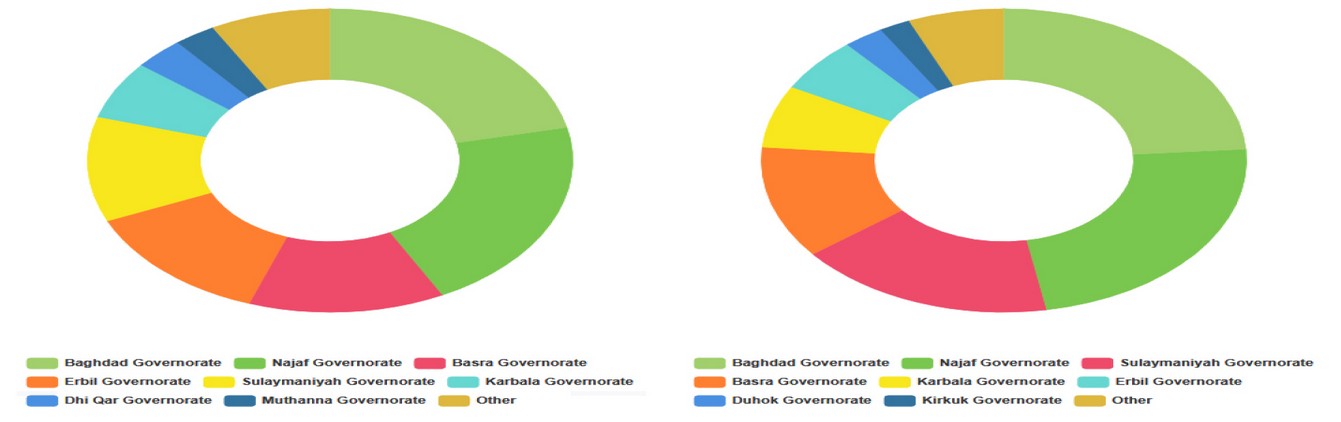
Figure 3. Dounut chart displays the proportion of reported Iraqi COVID-19 confirmed cases, deaths, and recoveries sofar.
Descriptive statistics of COVID-19 epidemic plateau in Gulf countries
The process of statistical analysis of a sample of data and use it to conclude its population includes the use of descriptive static for COVID- 19 in Gulf countries (table 2). We can test and start investigating causal relationships within infection data and country information with inferential statistics. We pursue useful information or models for data mining, especially in those which can be used to predict the epidemic development of COVID-19.
Descriptive statistics were reported for total Bahrain confirmed cases (M=233.77, SD=406.37, min=0, mix= 1744) and the confirmed cases of Iran with difference in area and population (M=1487.03, SD=24062.33, min.=0, max.=79494) and Iraq with others’ countries (M=241.31, SD=433.38, min=0, max=1482). The shortened COVID development cases in Oman comprised 8 Golf countries of a small public people (M=72.02, SD=229.97, min=0, mix= 1069) also and Kuwait the confirmed cases have intermediate descriptive statistics’ (M=187.06, SD=373.85, min=0, mix= 1658). The means for Saudi Arabia were highly infectious in few months (SD=1955.04, M=1678.42, min.=1, max.=7142) for others of Golf countries have foreigners and expatriates more than 2% (Qatar and UEA), so the max of cases was ≤ 4500 and meant ≤ 450.
Skewness is the peakedness or flatness in COVID-19 cases that can be predicated the country statement in epidemic growth or stability. Statistics of the asymmetry of vector distribution was strongly distorted in all Gulf countries. Oman > UEA > Qatar > Kuwait > Bahrain > Iraq > Iran>Saudi Arabia became extremely biased countries. The degree of skewness determines how symmetrical the distribution of a variable is. The variance tests the component distribution accuracy. Nevertheless, we think that in every Gulf country, organizing is a grant that can be linked to the similarity of infection types, food, and living habits. Skewness in coved confirmed cases was represented in kurtosis. Kurtosis is the calculation of outliers found in the distribution, the values for asymmetry and kurtosis of ±2 are considered appropriate, but most Gulf countries were disrupted by regular kurtosis means, Oman > UEA > Qatar > Kuwait > Bahrain > Iraq > Iran>Saudi Arabia.
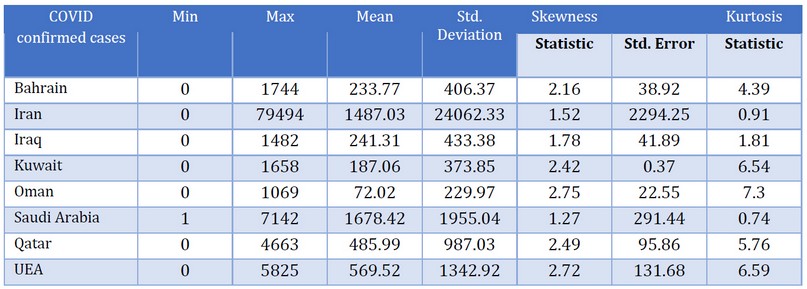
Table 2. Descriptive Statistics for COVID-19 in Gulf countries.
The current case fatality rate (CFR) of COVID-19
CFR is the ratio between confirmed cases and deaths, the figure 4. the number of confirmed COVID-19 events, and the total number of fatalities is seen in contrast. In every individual illness, there is no specific CFR statistic. The CFR differs from location to position and typically shifts with time. There are significant differences between the CFRs in Gulf countries, which are less than 1% in Oman, UEA, Kuwait, Bahrain, and Saudi Arabia, hitting 7.5% in Iraq and 8% in Iran. The Gulf Countries vary in material capacities in the medical knowledge, and other professional capabilities of trained administrators and Iraq is the competence of health personnel, who in recent years, have assisted emergencies.
However, it does not imply a fair assessment of the real likelihood that someone would die of COVID-19. Many cases are asymptomatic versus symptomatic, or whether the same test criteria apply to countries. The actual mortality rate remains uncertain without more and more systematic monitoring and reporting standards. To consider and direct decisions taking the CFR variations. CFR will assist us in recognizing the disease’s nature and what to do with it since CFR is a very weak metric for a small sample size mortality event. As time goes by, the CFR continues to slip.
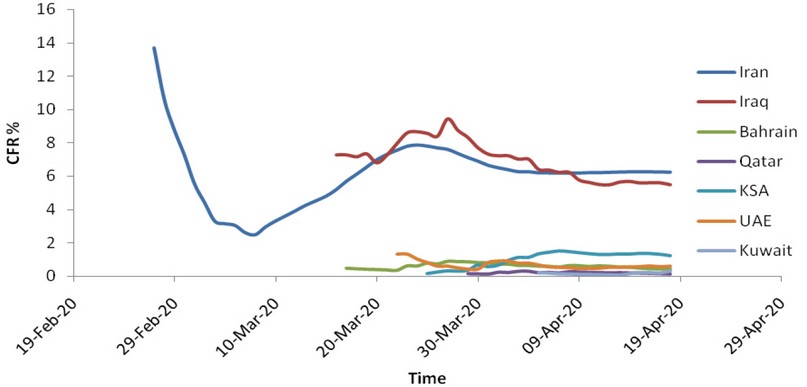
Figure 4. The case fatality rate of the ongoing COVID- 19 pandemics in Gulf countries.
Relationship between ABO blood group and COVID-19.
When comparing total cases of COVID - 19 in Gulf countries with the origin of their first case as Iran, which reached to 92542 at 28-April 2020, this may contribute to other factors such as blood group and their associated diseases such as diabetes, hypertension, and cardiovascular diseases. Blood group O is more abundant in Iraqi, Kuwait, Oman, Saudi Arabia, and UAE population; researchers found that individuals with blood group O are more resistant to infections, including SARS and COVID-19 while, blood group A may need more attention to prevent infection 12. This assumption may differ due to antigens of blood group A on different cells that can act as binding adhesion receptors, which allows COVID-19 to adhere and enter the cells via the ACE2 receptor. On the other hand, anti-A and anti-B antibodies that circulate in blood group O persons may be part of the first natural defense mechanism against viral infection.
The blood groups consist of two antigens, A and B antigens; they are produced by the ABO gene and are autosomal codominant. The group O phenotype is an autosomal –recessive phenotype due to the homozygous inheritance of two null ABO alleles; group O also express the H antigen, the biosynthetic precursor to A and B antigens. In addition to red blood cells, ABH antigens are widely expressed in many other tissues and secretions, such as intestinal mucosa, kidney, heart endothelium, and other organs. For such reason, the virus, which displays many glycosylated regions, could adhere to another organ such as intestinal mucosa. One of the most attractive areas of research is to find whether blood type and their natural antibodies could reduce the spread or severity of the infection.
On the other hand, many types of research were focused on the role of blood group in infection incidence of many pathogenic bacterial species as Enterotoxigenic Escherichia coli, Vibrio cholerae, Pseudomonas aeruginosa, as well as many viruses as norovirus, Norwalk virus13, and Hepatitis B virus14. The most accepted theory is that antigens of blood group on different cells can act as binding receptors that allow bacteria and viruses to attach and enter the cells 15. On the other hand, anti-A and anti-B antibodies may be part of the body’s natural defense that takes place to prevent infection or limit it.
The original severe acute respiratory syndrome outbreak caused by SARS-CoV in winter of 2002 to 2003 which infected 8000 persons worldwide, with a fatality rate of 10%; SARS-CoV is an enveloped RNA virus which adheres to host cells via viral adhesion glycoprotein the spike protein 210-230 kDa with 23 potential N- glycosylation sites 15. The analysis of glycan structure showed a wide range of structures, including complex N- glycans with 2 to 4 antennae capable of supporting ABH epitopes. The primary host target cells of SARS-CoV are respiratory and gastrointestinal mucosa, so its likely most human isolates express ABH antigens on the S protein and host envelope GSLs; expressing A antigen can be blocked by monoclonal anti-A and human anti-A16. Recent pandemic COVID-19 is similar in structure to SARS-CoV regarding its spike protein, which is called NSP15; scientists from the U.S. found 89% identity to NSP15 for both viruses. However, spike protein for SARS-CoV-2 is 10-20 times more likely to attach to human cells, which explain its rapid spread throughout the world.
According to epidemiological study as well as in vitro study, Guillon et al. 16 hypothesized that group O persons are more resistant to SARS-CoV due to ABO antibodies and could decrease the rate of infection throughout the population. The same pattern of distribution of blood group 17 O, A, B, AB occurring in the order O > A > B > A.B. were reported in the studies from neighboring countries; Saudi Arabia 18, Kuwait 19, Iran 20. Although, protection from infection may be influenced by the ABO antibodies titer, secretor status, and the incidence of group O in population. High titer of anti-A (1:256) gave effective blocking to infection, while the lower titer was ineffective 15. Other factors may affect, such as the environment of the population as industrialized countries tend to be less in ABO- antibodies titer. A non-secretor phenotype would also nullify viral neutralization since viral transmitted from a non-secretor lacks ABH expression. The result of Zhao and others 21 a significantly increased risk of blood group A for SARS-CoV-2 in comparison to group O. The differences in significant antigens present on the surface of red blood cells and other epithelial cells have significant clinical importance. These antigens have proved the association between ABO blood group and several serious diseases 22; besides infections, the most important is, cardiovascular disorders, diabetes and IL-6, and IL-10, IL-18, which may affect the infection with recent pandemic SARS-CoV-2 (table3 ).
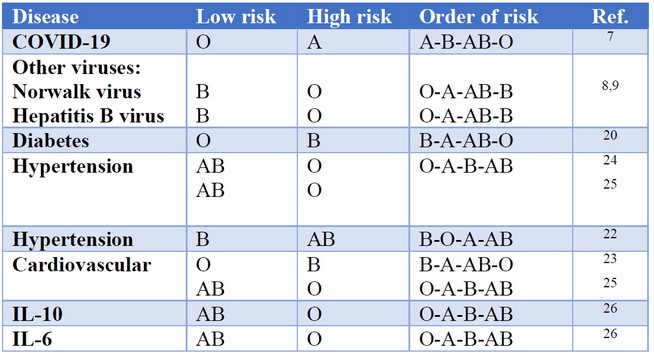
Table 3. Relationship between ABO group risk factors and diseases.
Many researchers ensured the involvement of ABO blood group and diabetes; it was found that blood type O had a lower risk of type 2 diabetes mellitus 23. Another work found that the B group was more prevalent in diabetic patients 24,25.
Hypertension has a significant impact on the health of communities in the whole world; it suspected to link to the ABO blood group via genetic determine at conception and remain fixed for life. Hence, its frequency distribution follows a known pattern governed by gene transmission from generation to generation and varies with the race and geographical distribution of the human being 26. There are reports of increased cardiovascular (CV) risks in different blood groups (non-O group), and an increase in B.P. is considered as a common CV risk 27.
A study that came from Iraq suggested that blood group O is at risk of hypertension and total cholesterol, followed by group A, B, then AB 28. Coronary Artery Diseases in Iranian Patients is more prevalent in blood group O comparing with another group 29. Other estimation of hypertension gave the percentage as follows B (8.7%) followed by group O (7.6%) group A (3.7%) and group AB (1.9%). Inflammation interleukins are also associated with ABO blood group; ABO antigens O and A2 are associated with increased IL-10 levels and decreased VWF level, and that the ABO antigens also influence the levels of sTF in Patients to have Artery coronal syndrome which is associated with disease outcomes in ACS patients 30.
Since the emergence of COVID-19 many types of research were conducted to determine specific comorbidities associated with increased risk of infection and worse outcomes with the development of increased severity of lung injury and mortality, the most common comorbidities in one report were hypertension (30%), diabetes (19%), and coronary heart disease (8%). Diabetes has emerged as an essential risk factor for severe illness and death from COVID-1931. Diabetes was present in 19% of COVID-19 cases in Wuhan, China, and non-survivors were significantly more likely to have diabetes than survivors (31% vs. 14%, P= 0.0051). While another study found that 27% of patients achieving the primary endpoint of intensive care unit (ICU) admission, mechanical ventilation, or death, compared with 6.1% if none of these complications occurred. Also, Bruce Bode et al. 32 in the USA diagnosed that diabetes and uncontrolled hyperglycemia frequently occurred among COVID-19 patients who had a particularly high mortality rate reached to 28.8% in diabetes patients who infected withCOVID-19.
A Chinese study dealing with immune markers in severe cases of COVID-19 found that baseline of IL-6 was significantly increased in patients with severe type, which is ensured by the maximal body temperature during hospitalization and C.T. findings. Baseline IL-6 was also significantly linked to the increase of baseline level of other immune markers, the CRP, lactate dehydrogenase (LDH), ferritin, and D- Dimer 33. The increase of baseline IL-6 level suggests that it may positively correlate with the cytokine storm syndrome of COVID-19. An early study by Jaques 34 demonstrated that a surface viral protein from the SARS virus directly stimulated the production of tumor necrosis factor (TNF)- and interleukin.
Recent pandemic SARS-CoV-2 is similar in structure to SARS-CoV regarding its spike protein, which is called NSP15; scientists from the U.S. found 89% identity to NSP15 for both viruses. However, spike protein for SARS-CoV-2 is 10-20 times more likely to attach to human cells, which explain its rapid spread throughout the world. Proteome analysis derived from online NCBI databases showed existing the following:
- A polyprotein orf1a 7096 amino acid long (QHD43415.1)
- A surface glycoprotein “Spike” (1273 aa - QHD43416.1)
- ORF3a or structural protein E (273 aa - QHD43417.1)
- An envelope protein (ep – 75 aa - QHD43418.1)
- A membrane glycoprotein (MGP – 222 aa - D43419.1)
- ORF6 (61 aa - QHD43420.1)
- ORF7a (121 aa - QHD43421.1)
- ORF8 (121 aa - QHD43422.1)
- A Nucleo capsid phosphoprotein (419 aa - QHD43423.2)
- ORF10 (38 aa - QHI42199.1).
CONCLUSIONS
The present research has shown that for the COVID- 19 epidemic, an epidemic spike somewhat of an epidemic height, owing to the length of the height cycle from week to month and beyond. For this, the epidemic spike is emotional rather than a strong epidemic. Accurate enough, as figures and quadratic growth are contained here, are the details necessary to discern between early exponential growths.
It is also noteworthy that the fit isolates of January 20/2020 are a deciding moment for the creation of the gulf breakup among the Gulf States. It has been predicted that growth would not be exponential and that they would get degrees slowly off in response to demographic changes and interventions. The case fatality rate in the gulf community is already still below 5 percent, but monitoring measures should be optimistic that this will not rise. Significant gaps in our knowledge of epidemiology, community prevalence, and clinical spectrum of infection and disease need urgent definition.
After its diagnosis as a causative agent of pneumonia cases in China, COVID-19 has become a pandemic and affects almost all places in the whole words. Arab countries in the Gulf region recorded their first case of infection from persons who came from Iran. Arab countries became alert for the new pandemic disease and gave serious attention to overcome COVID-19.
Blood group is One of the most critical subjects in controlling COVID-19 and its severity; many serious diseases link to blood group either through antigens located at the erythrocyte or encoding different genes that correlate to diseases. Diseases such as hypertension, diabetes, coronary heart disease, cytokines secretion as well as infection by the virus itself. Knowledge of disease history to a person with COVID-19 allowed proper cure, observation, and treatment to avoid the severity of the infection.
REFERENCES
1. Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterization and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–74.
2. Tuite AR, Fisman DN. Reporting, Epidemic Growth, and Reproduction Numbers for the 2019 Novel Coronavirus (2019-nCoV) Epidemic. Ann Intern, Med. 2020. (February):2019–20. 2.
3. Zhao S, Cao P, Gao D, Zhuang Z, Chong MKC, Cai Y. Epidemic growth and reproduction number for the novel coronavirus disease (COVID-19) outbreak on the Diamond Princess cruise ship from 20 January to 19 February, 2020: A preliminary data-driven analysis. SSRN. 2020. Preprint at: https://ssrn.com/abstract=3543150.
4. Zhang W, Du RH, Li B, Zheng XS, Yang XL, Hu B. (2020). Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect.;9(1):386–9.
5. Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis.J Pathol. 2004;203(2):631–7.
6. Chen YS, K.; Qian, W. Asians Do Not Exhibit Elevated Expression or Unique Genetic Polymorphisms for ACE2, the Cell-Entry Receptor of SARS-CoV-2. Preprints, 2020, 2020020258. 2020.
7. Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W. (2020). A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature.https://doi.org/10.1038/s41586-020-2012-7.
8. Roussel, Y., Giraud-Gatineau, A., Jimeno, M. T., Rolain, J. M., Zandotti, C., Colson, P., & Raoult, D. (2020). SARS-CoV-2: fear versus data. International journal of antimicrobial agents, 105947. Advance online publication. https://doi.org/10.1016/j.ijantimicag.2020.105947
9. Coleman CM, Sisk JM, Mingo RM, Nelson EA, White JM, Frieman MB. Abelson Kinase Inhibitors Are Potent Inhibitors of Severe Acute Respiratory Syndrome Coronavirus and Middle East Respiratory Syndrome Coronavirus Fusion. J Virol. 2016;90(19):8924–8933. Published 2016 12 September. doi:10.1128/JVI.01429-16
10. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y. (2020). Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia.N Engl J Med. https://doi.org/10.1056/NEJMoa2001316 [Epub ahead of print].
11. Lee PI, Hsueh PR. (2020). Emerging threats from zoonotic coronaviruses-from SARSand MERS to 2019-nCoV. J Microbiol Immunol Infect. https://doi.org/10.1016/j.jmii.2020.02.001 [Epub ahead of print].
12. ZhaoJ., Yang Y., Huang H., , Li D. Gu D., Xiangfeng, Lu X, Zhang Z, Liu L., Liu T., Liu Y. He Y., Sun B., Wei M., Yang G. , Wang X., Zhang L. Zhou X.Xing M. Wang P. G. (2020). Relationship between the ABO Blood Group and the COVID-19 Susceptibility.https://doi.org/10.1101/2020.03.11.20031096.
13. Hutson A.M., Atmar R. L., Graham D. Y. and ester M. K. (2002). Norwalk virus infection and disease is associated with ABO Histo- Blood group Type. The Journal of Infectious Diseases, 185:1335–1337.
14. Jing W, Zhao S, Liu J, et al. ABO blood groups and hepatitis B virus infection: a systematic review and meta-analysis. BMJ Open 2020; 10:e034114. doi:10.1136/ bmjopen-2019-034114.
15. Mazda T, Yabe R, NaThalang O, Thammavong T, Tadokoro K. 2007.Differences in ABO antibody levels among blood donors: a comparison between past and present Japanese, Laotian and Thai populations. Immunohematology,23:38–42.
16. Guillon P, Clement M, Sebille V, Rivain J-G, Chou C-F, Ruvoen-Clouet N, Le Pendu J.(2008). Inhibition of the interaction between the SARS-CoV spike protein and its cellular receptor by anti-histo-blood group antibodies. Glycobiology18:1085–1093. http://dx.doi.org/10.1093/glycob/cwn093.
17. Saleh, S. M. and Abood A. S. (2016). ABO and Rh (D) Blood Groups’ Distribution and Gene Frequencies in North Baghdad Population–Iraq. International Journal of Scientific & Engineering Research, 7(8): 581-584. http://www.ijser.org.
18. Sarhan MA, Saleh KA, Bin-Dajem SM. (2009) Distribution of ABO blood groups and rhesus factor in Southwest Saudi Arabia. Saudi Med J.;30(1):116–119.
19. Al-Bustan S, El-Zawahri M, Al-Azmi D, Al-Bashir AA. (2002). Allele frequencies and molecular genotyping of the ABO blood group system in a Kuwaiti population. Int J Hematol.;75(2):147–153.
20. Boskabady MH, Shademan A, Ghamami G, Mazloom R.(2005). Distribution of blood groups among population of the city of Mashhad (North East of Iran). Pak J Med Sci Q.;21(2):194–198.
21. ZhaoJ., Yang Y., Huang H., , Li D. Gu D., Xiangfeng, Lu X, Zhang Z, Liu L., Liu T., Liu Y. He Y., Sun B., Wei M., Yang G. , Wang X., Zhang L. Zhou X.Xing M. Wang P. G. (2020). Relationship between the ABO Blood Group and the COVID-19 Susceptibility.https://doi.org/10.1101/2020.03.11.20031096.
22. Cooling L. (2015).Blood Groups in Infection and Host Susceptibility.Clinical Microbiology Reviews, 28 ( 3):801- 870.
23. Fagherazzi G, Gusto G, Clavel-Chapelon F, Balkau B, Bonnet F. (2015). ABO and Rhesus blood groups and risk of type 2 diabetes: evidence from the large E3N cohort study. Diabetologia.; 58(3):519-22. PMID: 25533388
24. Bener A. andYousafzai MT. (2014).The distribution of the ABO blood groups among diabetes mellitus patients in Qatar. Niger J ClinPract.; 17(5):565-8. PMID: 25244264
25. Moinzadeh F, MahdiehNajafabady G, Toghiani A. (2005). Type 2 diabetes mellitus and ABO/Rhblood groups. J Res Med Sci. 2014; 19(4): 382. PMID: 25097615.
26. Kearney PM, Whelton M, Reynolds K et al. (2005): Global burden of hypertension: Analysis of worldwide data. Lancet, 365:217-23.
- Okeke CO., Okoro US. and Babatunda A. (2018). Variation in activated partial thromboplastin time and prothrombin time in indivisuals of A, B, AB and O blood groups. Iraqi J. Hematol. 7: 85-89.
28. Jasim W. E. (2012). Association of ABO blood group in Iraqis with hypercholesterolemia, hypertension and diabetes mellitus. EMHJ 18 (8):888-891.
29. Anvari M. S., Boroumand M. A., BineshEmami, AbbasaliKarimi, Maryam Soleymanzadeh, SeyedHesameddinAbbasi, SoheilSaadat, (2009). ABO Blood Group and Coronary Artery Diseases in Iranian Patients Awaiting Coronary Artery Bypass Graft Surgery: A Review of 10,641 Cases.Lab medicine, 40 ( 9 ) :528-530.
30. Johansson Å, Alfredsson J, Eriksson N, Wallentin L, Siegbahn A (2015) Genome-Wide Association Study Identifies That the ABO Blood Group System Influences Interleukin-10 Levels and the Risk of Clinical Events in Patients with Acute Coronary Syndrome. PLoS ONE 10(11): e0142518. doi:10.1371/journal.pone.0142518.
31. Hussain, A., Bhowmik, B., & do Vale Moreira, N. C. (2020). COVID-19 and diabetes: Knowledge in progress. Diabetes research and clinical practice, 162, 108142. Advance online publication. https://doi.org/10.1016/j.diabres.2020.108142
32. Bruce Bode , Valerie Garrett, Jordan Messler, Raymie McFarland, Jennifer Crowe, Robby Booth, David C. Klonoff, M.D.(2020). Glycemic Characteristics and Clinical Outcomes of COVID-19 Patients Hospitalized in the United States.
33. Metha P., McAutey D. F., Brown M., Sanchez E., Tatterall R. and Mansan J. J.(28 March 2020). COVID-19 considers cytokine storm syndrome and immunosuppression. Lancet,395(10229).
34. Jacques A. Alexandre Jacques,1 Christian Bleau,1 Claire Turbide,2 Nicole Beauchemin2 and Lucie Lamontagne1 et al. Macrophage interleukin-6 and tumor necrosis factor-a are induced by coronavirus fixation to Toll-like receptor 2/heparansulphate receptors but not carcinoembryonic cell adhesion antigen 1a, Immunology (2009) doi: 10.1111/j.1365-2567.2008.02946.x
Received: 29 April 2020
Accepted: 8 May 2020
Raghad S. Mouhamad1
1, Ministry of Science and Technology, Baghdad, Iraq
https://orcid.org/0000-0003-3335-254X
Khlood Abedalelah Al-Khafaji 1
1, Ministry of Science and Technology, Baghdad, Iraq
Risala H. Allami2
https://orcid.org/0000-0002-3000-4614
2 Al-Nahrian University - College of biotechnology, Iraq
Michael Alabboud3
https://orcid.org/0000-0002-0246-0436
3 Department of Horticultural Sciences, UTCAN, University of Tehran, Iran
Maha Hameed Abdulla2,
https://orcid.org/0000-0001-8066-4584
2 Al-Nahrian University - College of biotechnology, Iraq.
Mohammed M. Jafaar
