2023.08.01.35
Files > Volume 8 > Vol 8 No 1 2023
Knowledge and awareness of chronic hepatitis C and liver fibrosis among health care personnel and other domains in Iraq
1 Middle Technical University(MTU), Baquba Technical Institute, Baquba, Iraq
2 Middle Technical University, Baquba Technical Institute, Baquba, Iraq
*Correspondence authors. [email protected]
Available from: http://dx.doi.org/10.21931/RB/2023.08.01.35
ABSTRACT
As a significant public health disease, the Hepatitis C virus (HCV) infects more than 185 million worldwide. Chronic infections are led by 170 million illnesses, resulting in 350,000 because of liver and cirrhosis cancer. Injuring of chronic liver from several insults leads to occur fibrosis. For example, metabolic disease (nonalcoholic fatty liver disease), infections (hepatitis B [HBV] and C viruses [HCV]), and toxins (alcohol). This study evaluates the knowledge and awareness about Of Chronic Hepatitis C and Liver Fibrosis among Health Care Workers and other domains of workers in Iraq. This study was carried out as cross-sectional research in Diyala, Iraq, from February / 2021 to January / 2022. In this work, 350 persons participated; the age range was (18-62) years, with a mean age of (25.9 + 9.79). The participants consisted of 100 males and 250 females. Also, they were divided into two groups: groups I and II. I (health care workers group) consists of 200 students studying in the medical department of Baquba technical institute and workers in Diyala hospitals ). Group II (other domains Workers) includes (100) participants who work in several domains. Similar to previous studies, a questionnaire was adopted to collect this research data. The outcomes demonstrate higher knowledge about HCV, Liver fibrosis, transmission, and a vaccine was noticed with a statistically significant difference among females compared to males. Regarding residency, the ability of HCV and liver fibrosis in Q1, Q2, and Q5 only among Health Care Workers compared to other domains Workers with a statistically significant difference (P<0.05).
Keywords: Chronic Hepatitis C, Liver Fibrosis, Health Care Workers and other domains Workers
INTRODUCTION
As a significant public health disease, the Hepatitis C virus (HCV) infects more than 185 million worldwide 1, 2. Chronic infections are led by 170 million infections, resulting in 350,000 because of liver and cirrhosis cancer 3. In Iran, the rate of tee overall seroprevalence of HCV infection reaches 0.6% 4. Spontaneously, a few patients (20–30%) recover, while the remaining (70–80%) progress into a chronic infection, of whom 25% lead to hepatocellular carcinoma and cirrhosis 5, 6. There are seven genotypes in the HCV, including more than 65 subtypes 7, 8. Around the world, the most common HCV genotype 1 9–11. Approximately 1% of Canadians are hepatitis C (HCV)- infected 12, 13. HCV confers a more significant burden regarding reduced functioning and premature mortality among many infectious diseases 14. Including hepatocellular carcinoma and liver failure, the liver-specific complications of HCV are well developed, and so are the benefits of curative HCV antiviral therapy on these findings 15. On the other hand, the burden of associated extrahepatic comorbidity is less well known. Many works have established HCV is associated with renal impairment and chronic kidney disease 16 –21.
The most advanced stage of hepatic fibrosis, with 0.1% of the European population affected by cirrhosis, is a continuous growth of the burden of chronic liver disease 22. Fibrogenesis is the common pathological mechanism that causes cirrhosis, although the disease's etiology varies among countries. Injuring of chronic liver from several insults leads to occur fibrosis. For example, metabolic disease (nonalcoholic fatty liver disease), infections (hepatitis B [HBV] and C viruses [HCV]), and toxins (alcohol) 23.
MATERIALS AND METHODS
Participants
In this work, 350 persons participated; the age range was (18-62) years, with a mean age of (25.9 + 9.79). The participants consisted of 100 males and 250 females. Also, they were divided into two groups: groups I and II. Specifically, group I (health care workers group) consists of 200 students studying in the medical department of Baquba technical institute and workers in Diyala hospitals ). Group II (other domains Workers) includes (100) participants who work in several domains. Similar to previous studies, a questionnaire was used to collect the data for this study.
Measures
Similar to previous works, as listed in table 1, a self-administered questionnaire was used to measure participants' knowledge and awareness of Liver Fibrosis and HCV. In this study, two microbiologist experts (from the microbiology division in the Medicine and Education for Pure Science Colleges) confirmed this questionnaire's validation. The Arabic language was used to write the questionnaire; then, it was translated to English. To collect the data, the questionnaire was categorized into two parts:
1. Demographic characteristics.
2. Ten questions related to the knowledge of HCV infection and liver fibrosis, the questions evaluating knowledge were "Yes / No / Don't know patterns" shown in table 2 .
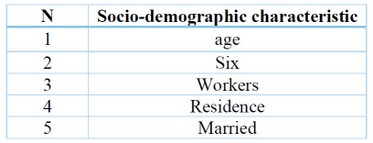
Table 1. Show the Demographic characteristics
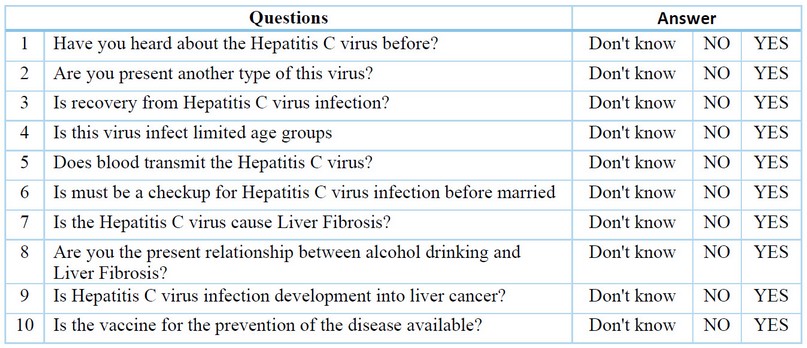
Table 2. Ten questions related to the knowledge of HCV infection and liver fibrosis
Procedure
As a cross-sectional study, this work was conducted in Baqubah-Diyala province from February / 2021 to January / 2022. A face-to-face interview was conducted. Before the discussion started, all the participants in this work gave prior approval. After the conversation, the contributors received information about HCV infection and liver fibrosis
Data Analysis
SPSS software 22nd edition was adopted to perform the statistical analysis. The percentage test used the correct answer only to compare different variables.
RESULTS
Three hundred and fifty ( 350 ) members joined in this research. Table 3 illustrates the members' quantitative starting point data: mean age, sex, groups and residence.
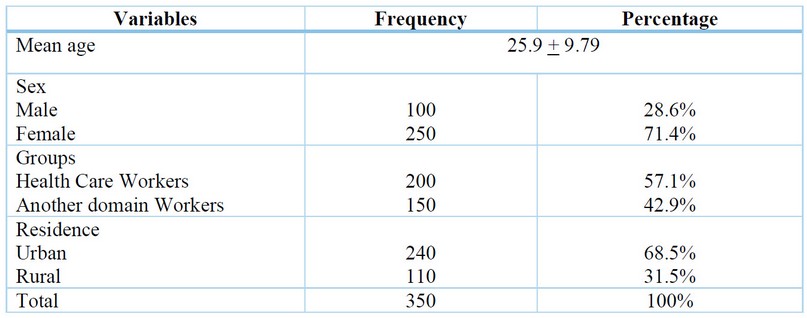
Table 3. Baseline data of participants
Table 4 lists the quantitative results of evaluating participants' liver fibrosis HCV infection knowledge levels.
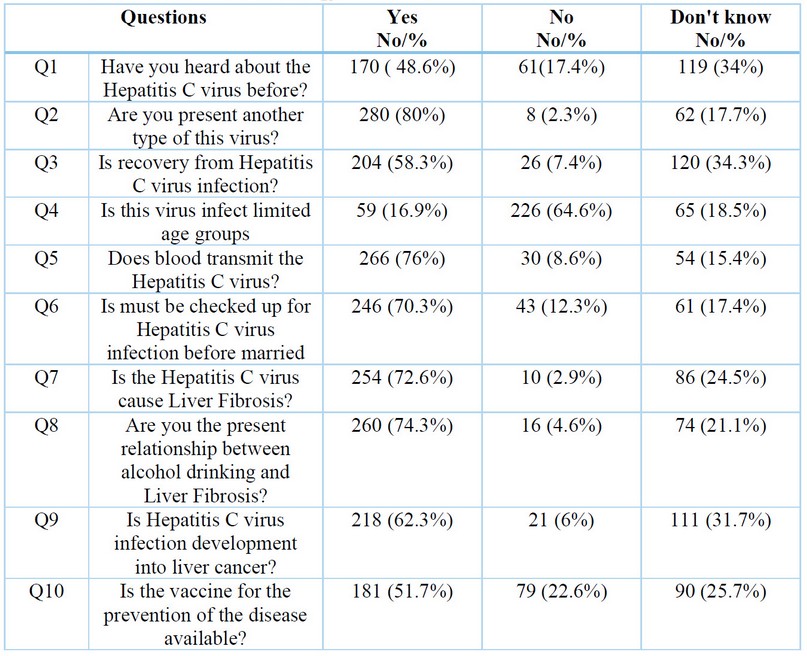
Table 4. Knowledge Of Chronic Hepatitis C and Liver Fibrosis among participants.
The results show higher knowledge about HCV, Liver fibrosis, vaccine, and transmission was noticed among women compared to men with a statistically significant difference (P < 0.05) in table 5 .
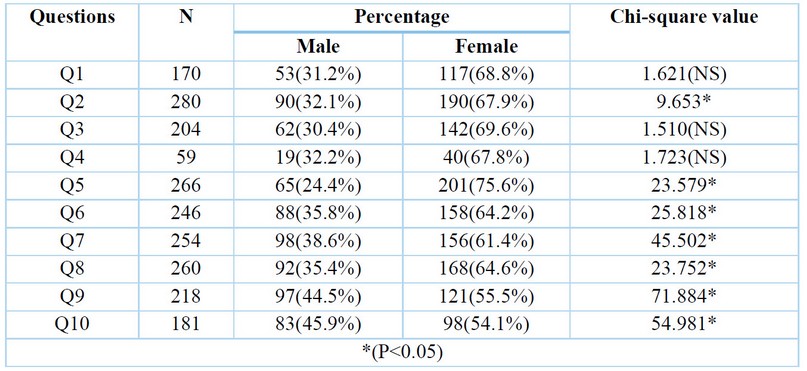
Table 5. The effect of sex according to the answer to the question –yes (percentage)
Among health care and other domains Workers, Table 6 compares the percentage knowledge (regarding the residency) of HCV and liver fibrosis in Q1, Q2, and Q5 only with a statistically significant difference (P < 0.05).
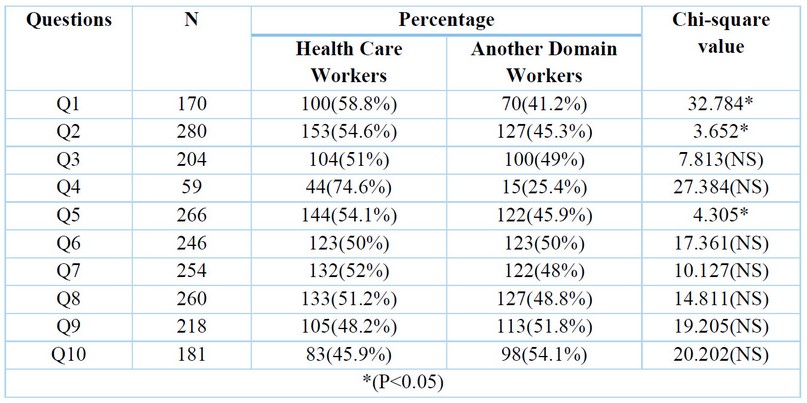
Table 6. Percentage comparison among healthcare and other domains Workers according to their yes responses.
Regarding the residency among urban participants, Table 7 shows knowledge about HCV and Liver fibrosis in Q2, Q4, Q5, Q6, Q7, Q8, and Q10 was more significant than in rural participants (P<0.05).
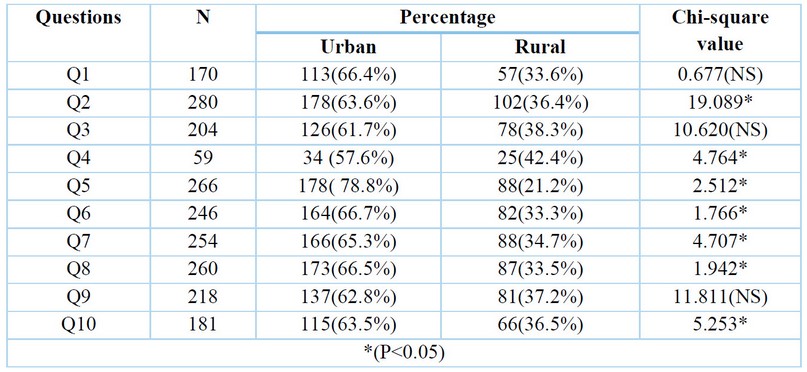
Table 7. Percentage of residence effect according to their yes responses.
DISCUSSION
To the best of our knowledge, this evaluation is the first study conducted in Diyala society to determine knowledge and awareness about Of Chronic Hepatitis C and Liver Fibrosis among Health Care Workers and other domains of Workers. As listed in table 2, according to Original Bloom's cut-off Points 24, the outcomes revealed good knowledge and awareness about HCV, Liver Fibrosis, infection transmission, risk factors (alcohol drinking), and vaccines. In particular,170 (48.6%) participants said they had heard about HCV. Despite few real works assessing the awareness of hepatitis C in specific populations, the literature states that knowledge about HCV is poor. In a cohort of 3,768 females who were or had at risk for infection of HIV, about (1/4) of those with chronic HCV infection were not aware of their infection status 25. Black and younger females were less likely to be mindful of the status of their HCV infection.
In contrast, females with a history of injection drugs, past alcohol treatment, or increased liver enzyme (alanine aminotransferase) were more likely to be aware that they were positive for HCV infection. Most participants had very high knowledge about HCV transmission, where 266 (76%) of them correctly answered. These outcomes agree with Stein et al. (2001) survey conducted on 306 former IDUs about their knowledge of liver disease risk, HCV transmission, and infection status 26. By sharing contaminated needles and blood, the authors determined that about all the participants know about how HCV is transmitted. 82% were HCV seropositive among people who did not know their test results or had not been tested. As in other surveys, 1/3 of participants stated that seronegative were seropositive, demonstrating that self-reported infection status is unreliable. In the next ten years, 81% of the respondents anticipated their risk of developing liver disease (specifically cirrhosis) at 50% or greater. The authors in 35, 36 reported on healthcare providers' knowledge of HCV transmission. Most healthcare providers identified the main transmission routes in the studies as sharing needles while injecting drugs, exposure to blood during sexual activity, and blood transfusions 35-36. In hemodialysis clinics in Italy, 12% misbelieved kissing in one of the methods that contributed to HCV transmission, 19% of nurses did not know HCV transmitted that getting in tattoo work 35.
Only 254 (72.6%) of the participants' respondents knew that Is Hepatitis C virus cause Liver Fibrosis. The public's knowledge about HCV's natural history 27,28,33 has been published in eight works. In two Canadian works, 83–90% of participants believed that someone with HCV is unaware of an existing infection 30, 32. Likewise, about (57%) of US baby boomers believed that liver cancer results from HCV infection. Additionally, (61%) stated that no symptoms could be presented to anyone infected with HCV [27]. Another work published previously stated that (1/3) of MSN believed that anyone infected with HCV could lead to liver failure (37%) and liver cancer (31%) 33.
In contrast, a study has been conducted on immigrants from Asia stated that there is uncertainty about the natural history of HCV and confusion about the different categories of hepatitis infections 33. This research demonstrated that females have limited knowledge and awareness that HCV infects limited age groups; only 59(16.9%) correctly answered. Concerning the vaccine for prevention, 181 (51.7%) of participants correctly responded that the vaccine is available to prevent the disease. The authors in 29, 31, 34 found a misconception about vaccine availability to avoid infection among the general public. (1/2) of the participants interviewed in a Candian study knew about the vaccine availability to prevent the infection 30. Similarly, 60% of African-American baby boomers and 42% of American baby boomers in two US studies knew about HCV prevention by vaccine 27, 29.
Compared with rural participants, the urban showed high knowledge about HCV history, vaccine, type of virus, transmission, liver cancer, and alcohol drinking with statistically significant differences (P). Assessing high-risk populations (such as incarcerated or indigenous peoples) will likely be included in future works with consistent and clear definitions of knowledge and awareness. Additionally, adopting assessing factors associated with differences in knowledge and awareness (e.g., socioeconomic status). Future knowledge translation and exchange products are the main targets of further studies on healthcare providers' knowledge of the infection. Therefore, there is a need to increase the general public's knowledge and awareness of HCV with healthcare providers to support the discussion of considering HCV tests. This study's obtained gaps and findings can help public health campaigns and future interventions for HCV.
CONCLUSION
This work showed inadequate knowledge and awareness about HCV, Liver fibrosis, transmission, and vaccine (especially the other domains Workers) among study groups. Such as Liver fibrosis, HCV infection, and its complications negatively affect all humans. Accordingly, screening programs and Education are crucial to avoiding HCV infections.
REFERENCES
1. Hajarizadeh B, Razavi-Shearer D, Merat S, Alavian SM, Malekzadeh R, Razavi H. Liver disease burden of hepatitis C virus infection in Iran and the potential impact of various treatment strategies on the disease burden. Hepat Mon. 2016;16(7):e37234.
2. Rahimi P, Solati R, Shokri M, Vahabpour R, Mahmoudizad F, Aghasadeghi M, et al. Evaluation of full length E1 and E2 glycoproteins of HCV expressed in P. pastoris as a protein-based vaccine candidate. Vacc Res. 2015;2(3):74–80.
3. Mirminachi B, Mohammadi Z, Merat S, Neishabouri A, Sharif AH, Alavian SH, et al. Update on the prevalence of hepatitis C virus infection among Iranian general population: a systematic review and meta-analysis. Hepat Mon. 2017;17(2):e42291.
4. Sarvari J, Mansouri M, Hashempoor T, Hosseini SY, Moattari A, Pirbonyeh N, et al. Association of genotype and haplotype of IL-28B gene with hepatitis C infection outcome in Iran: spontaneous clearance versus chronic infection. Hepat Mon. 2017;17(5):e45745.
5. Tameshkel FS, Niya MHK, Sohrabi M, Panahi M, Zamani F, Imanzade F, et al. Polymorphism of IL-28B gene (rs12979860) in HCV genotype 1 patients treated by pegylated interferon and ribavirin. Iran J Pathol. 2016;11(3):216.
6. Sarvari J, Norozian H, Fattahi MR, Pirbonyeh N, Moattari A. The role of inter‑ feron gamma gene polymorphism (+874A/T, +2109A/G, and −183G/T) in response to treatment among hepatitis C infected patients in Fars Province, Southern Iran. Hepat Mon. 2014;14(1):e14476.
7. Chen Y, Yu C, Yin X, Guo X, Wu S, Hou J. Hepatitis C virus genotypes and sub‑ types circulating in Mainland China. Emerg Microbes infect. 2017;6(1):1–7.
8. Messina JP, Humphreys I, Flaxman A, Brown A, Cooke GS, Pybus OG, et al. Global distribution and prevalence of hepatitis C virus genotypes. Hepatol‑ ogy. 2015;61(1):77–87.
9. Mahmud S, Akbarzadeh V, Abu-Raddad LJ. The epidemiology of hepatitis C virus in Iran: systematic review and meta-analyses. Sci Rep. 2018;8(1):150.
10. Ansari N, Doosti M, Ahmadi A, Kakavandi E, Yazdani S, Shayestehpour M. Distribution of hepatitis C virus genotypes in Yazd, Central Province of Iran: increasing the mixed genotypes. Iran J Virol. 2016;10(2):19–24.
11. Ashraf Hafez A, Baharlou R, Mousavi Nasab SD, Ahmadi Vasmehjani A, Shayestehpour M, Joharinia N, et al. Molecular epidemiology of diferent hepatitis C genotypes in serum and peripheral blood mononuclear cells in Jahrom city of Iran. Hepat Mon. 2014;14(5):e16391.
12. Rotermann M, Langlois K, Andonov A, Trubnikov M. Seroprevalence of hepatitis B and C virus infections: results from the 2007 to 2009 and 2009 to 2011 Canadian health measures survey. Health Rep. 2013;24(11):3–13.
13. Payne E, Totten S, Archibald C. Hepatitis C surveillance in Canada. Can Commun Dis Rep. 2014;40(19):421–8.
14. Kwong JC, Ratnasingham S, Campitelli MA, et al. The impact of infection on population health: results of the Ontario burden of infectious diseases study. PLoS One. 2012;7(9):e44103.
15. Myers RP, Krajden M, Bilodeau M, et al. burden of disease and cost of chronic hepatitis C infection in Canada. Can J Gastroenterol Hepatol. 2014; 28(5):243–50.
16. Fabrizi F, Donato FM, Messa P. Association between hepatitis C virus and chronic kidney disease: a systematic review and meta-analysis. Ann Hepatol. 2018;17(3):364–91.
17. Henson JB, Sise ME. The association of hepatitis C infection with the onset of CKD and progression into ESRD. Semin Dial. 2019;32(2):108–18.
18. Kuna L, Jakab J, Smolic R, Wu GY, Smolic M. HCV extrahepatic manifestations. J Clin Transl Hepatol. 2019;7(2):172–82.
19. Park H, Chen C, Wang W, Henry L, Cook RL, Nelson DR. Chronic hepatitis C virus (HCV) increases the risk of chronic kidney disease (CKD) while effective HCV treatment decreases the incidence of CKD. Hepatology. 2018;67(2):492–504.
20. Pol S, Parlati L, Jadoul M. Hepatitis C virus and the kidney. Nat Rev Nephrol. 2019;15(2):73–86.
21. Tsui JI, Vittinghoff E, Shlipak MG, et al. Association of hepatitis C seropositivity with increased risk for developing end-stage renal disease. Arch Intern Med. 2007;167(12):1271–6.
22. Pimpin L et al. Burden of liver disease in Europe: Epidemiology and analysis of risk factors to identify prevention policies. J Hepatol. 2018;69(3):718-35.
23. Pinzani M. Pathophysiology of Liver Fibrosis. Dig Dis. 2015;33(4):492-7.
24. Johon, J. The knowledge and attitudes, practice and perceived barriers towards screening for premalignant cervical lesions among women aged 18 years and above, In Songea Urban, Ruvuma. Thesis. Muhimbili University of Health and Ahied Science. 2011.
25. Cohen, M. H., D. Grey, J. A. Cook, K. Anastos, E. Seaberg, M. Augenbraun, P. Burian, M. Peters, M. Young, and A. French. 2007. Awareness of hepatitis C infection among women with and at risk for HIV. Journal of General Internal Medicine 22(12):1689-1694.
26. Stein, M. D., J. Maksad, and J. Clarke. 2001. Hepatitis C disease among injection drug users: Knowledge, perceived risk and willingness to receive treatment. Drug and Alcohol Dependence 61(3):211-215.
27. Allison WE, Chiang W, Rubin A, Oshva L, Carmody E. Knowledge about hepatitis C virus infection and acceptability of testing in the 1945–1965 birth cohort (baby boomers) presenting to a large urban emergency department: a pilot study. J Emerg Med 2016 Jun;50(6):825–831.e2. http://dx.doi.org/10.1016/j.
jemermed.2016.02.001.
jemermed.2016.02.001.
28. CATIE. Room for improvement: knowledge exchange needs of people living with hepatitis C. Toronto: CATIE; 2015.
29. Crutzen R, Göritz AS. Public awareness and practical knowledge regarding Hepatitis A, B, and C: a two-country survey. J Infect Public Health 2012 Apr;5(2):195–8. http://dx.doi.org/10.1016/j. jiph.2011.12.001.
30. EKOS Research Associates Inc. 2012 HIV/AIDS attitudinal tracking
survey. Ottawa: EKOS; 2012 Oct. http://www.catie.ca/sites/default/ files/2012-HIV-AIDS-attitudinal-tracking-survey-final-report.pdf
survey. Ottawa: EKOS; 2012 Oct. http://www.catie.ca/sites/default/ files/2012-HIV-AIDS-attitudinal-tracking-survey-final-report.pdf
31. Hopwood M, Lea T, Aggleton P. Multiple strategies are required to address the information and support needs of gay and bisexual men with hepatitis C in Australia. J Public Health (Oxf) 2016 Mar;38(1):156–62. http://dx.doi.org/10.1093/pubmed/fdv002.
32. Ipsos Healthcare. Survey on hepatitis C knowledge and perception among Canadians and GP, September 2012. Paris: Ipsos; 2012.
33. Owiti JA, Greenhalgh T, Sweeney L, Foster GR, Bhui KS. Illness perceptions and explanatory models of viral hepatitis B & C among immigrants and refugees: a narrative systematic review. BMC Public Health 2015 Feb;15:151. http://dx.doi.org/10.1186/s12889-015- 1476-0.
34. Rashrash ME, Maneno MK, Wutoh AK, Ettienne EB, Daftary MN. An evaluation of hepatitis C knowledge and correlations with health belief model constructs among African American "baby boomers". J Infect Public Health 2016 Jul-Aug;9(4):436–42. http://dx.doi. org/10.1016/j.jiph.2015.11.005.
35. Bianco A, Bova F, Nobile CG, Pileggi C, Pavia M; Collaborative Working Group. Healthcare workers and prevention of hepatitis C virus transmission: exploring knowledge, attitudes and evidence-based practices in hemodialysis units in Italy. BMC Infect Dis 2013 Feb;13(76):76. http://dx.doi.org/10.1186/1471-2334-13-76.
36. Todorova TT, Tsankova G, Tsankova D, Kostadinova T, Lodozova N.
Knowledge and attitude towards hepatitis B and hepatitis C among
dental medicine students. J of IMAB 2015;21(3):810–3.
Knowledge and attitude towards hepatitis B and hepatitis C among
dental medicine students. J of IMAB 2015;21(3):810–3.
Received: October 23, 2022 / Accepted: January 15, 2023 / Published:15 February 2023
Citation: Mohammed Mohsen S, Hussein Majeed G. Knowledge and awareness of chronic hepatitis C and liver fibrosis among health care personnel and other domains in Iraq.Revis Bionatura 2023;8 (1)35. http://dx.doi.org/10.21931/RB/2023.08.01.35
