2021.06.03.34
Files > Volume 6 > Vol 6 No 3 2021
Johanna Pilay Bajaña1, Evelyn Ramírez Carguacundo1, María José Vizcaino Tumbaco2, Daniel Silva-Ochoa 1,2, Davide Di Grumo3, Luis Dorado-Sanchez4, Silvia Orellana-Manzano3, Patricia Manzano1,5, Andrea Orellana-Manzano1,2,3*
Available from http://dx.doi.org/10.21931/RB/2021.06.03.34
ABSTRACT
The worldwide spread of the virus has claimed multiple lives, especially in vulnerable groups. Therefore, an investigation was carried out to present a viable solution for health personnel using the “JES” algorithm. The present study used the research to determine the possible complications presented by the sick individual, providing a viable and accessible healthcare personnel solution through the proposed “JES” algorithm. A non-experimental, descriptive, correlational, and explanatory research is presented. According to pathologies of interest, the articles were taken virtually from scientific journals present in Google Scholar and PubMed. The excluded publications were: articles that do not detail the established protocol for detecting SARS-CoV-2, studies that do not present a significant number of people with Covid-19 disease, articles that the person has the covid-19 disease but no underlying diseases of nutritional origin. It focused on the vulnerable or higher risk population group, including scientific information from children (over five years old), adults (over 18 years old), and older adults (over 65 years old) found in countries of the Asian and American continents. The R program analyzed the scientific articles using the ggplot2 package with a pie and bar diagram.
A higher prevalence in men than women (56% vs. 44%) stood out. Likewise, arterial hypertension was presented in the first place with 40.82%, followed by diabetes with 30.61%, obesity with 12.24%, overweight and dyslipidemia with 6.12%, malnutrition with 4.08%. There was a higher prevalence of stable individuals (29%) within the health facility than those admitted to the ICU (20%). Adults with 69.39%, followed by older adults with 16.33%, and mixed ages with 14.29%. Comorbidities stand out as risk factors in people infected with SARS-CoV-2, regardless of age. A more significant contagion was observed in the male versus female population; since men do not develop a rapid immune response and have a high content of cytokines that at the time of infection are released more quickly and can cause more significant damage
Keywords: Chronic diseases, vulnerable population, SARS-CoV-2, nutrition
INTRODUCTION
The World Health Organization defines chronic diseases as long-term chronic diseases and progressively slower 1. Among them are heart diseases, high blood pressure (40.82%), diabetes mellitus 2 (30.61%), severe obesity (BMI> 40) (12.24%), and dyslipidaemias(6.12%) 2.
The virus is known as SARS-CoV-2 3, whose disease is caused by COVID-19 4 . It is considered a new type of infectious and highly contagious coronavirus in a latency state 5. Its mechanism of action consists of the host organism’s infection through the ACE2 receptor 6, distributed to various organs and tissues such as lungs, heart, kidneys, intestine, and endothelial cells 7. Clinical practice has determined that a population is considered vulnerable or at higher risk of contagion 8, such as the elderly and people at any stage of life with chronic diseases 9, 10 . Those people who have at least one of these chronic conditions mentioned above and are not under medical supervision should pay more attention and health care against SARS-CoV-2 8. The Pan American Health Organization emphasizes more outstanding care in vulnerable groups since 1 in 4 people show a greater risk of obtaining unfavorable results due to underlying diseases 11. Therefore, a search for information was carried out to relate the diseases of nutritional origin mentioned above with those who present the SARS-CoV-2 condition allowing us to know the relationship between them and the severity of complications.12 .
METHODS
Exhaustive bibliographic research was carried out, compiling 40 articles at the international level, adding nine more publications found within the previously selected articles, excluding those not indexed, for subsequent analysis focused on health professionals. These articles, “original articles,” were carried out in China, the United States, Italy, Mexico, France, and at a multicenter level from January 2020 to July 2020. It is considered non-experimental, descriptive, and explanatory research by searching bibliographic materials published from 2018 to 2020, taken virtually through search engines such as PubMed[A9] [A10] and Google Scholar. Pathologies of nutritional origin of interest categorized these scientific articles, as shown in figures 1 and 2. The excluded publications were selected as follows: articles that do not detail an established protocol for detecting SARS-CoV-2. These studies do not present a significant number of people with Covid-19 disease (less than 50 people), articles that the person has the covid-19 disease but not underlying diseases of nutritional origin. The information found with limited access, prepaid, and documents in development stands out regarding the restrictions. The keywords used for this search are SARS-CoV-2, Coronavirus, arterial hypertension, type 2 diabetes, dyslipidemia, and malnutrition, the latter being divided into malnutrition, overweight, and obesity. It was compiled through scientific studies carried out in China (26), United States (10), Italy (8), France (3), and Mexico (1). The choice of these countries was made according to the number of relevant articles found up to the moment of the analysis, which provided outstanding information on the relationship between SARS-CoV-2 and the pathologies of interest, a protocol established for obtaining results, as well as variables of interest, highlighting the different age groups, sex, country of study, detection method of the SARS-CoV-2, sample size, nutritional parameters, and the results obtained in said scientific studies.
Figure 1.- General steps for obtaining information from this document.
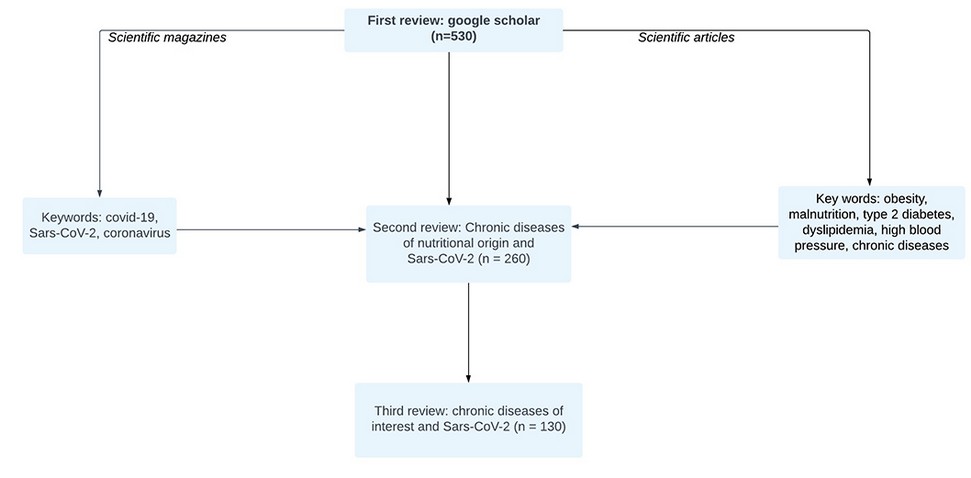
Figure 2.- Procedure for obtaining information.
The algorithm was carried out using the web-based diagramming tool called Lucidchart in its entirety due to the ease of implementation it presents and the different options it offers the user. It was based on the ten practical recommendations published by the European Society for Clinical Nutrition and Metabolism (ESPEN) in 2020, which presents an indicated guide for the nutritional management of patients with COVID-19. It contains relevant information about adequate nutritional management to treat patients with chronic diseases and SARS-CoV-2 simultaneously, highlighting the use of screening. Likewise, it indicates essential nutritional parameters to consider in the sick patient, such as BMI, ascites, folds, and brachial circumference.
For those patients with unfavorable results and a higher probability of mortality after contracting the SARS-COV-2 infection (older adults and people with multiple comorbidities), it is recommended to control the presence of malnutrition through screening tests for later timely evaluation using the NRS criteria. 2002 was established for hospitalized patients.
Likewise, it is recommended to maintain a good nutritional status for the prevention or treatment of malnutrition since it reduces complications and subsequent negative results in patients with nutritional risk due to the presence of nausea, vomiting, and diarrhea (typical of SARS-CoV-2 ), affecting the average intake and absorption of food in the body.
Optimal maintenance of nutritional status is prioritized through dietary advice from experienced professionals (Registered Dietitians, Experienced Nutrition Scientists, Clinical Nutritionists, and Specialty Physicians).
A daily intake of 27 kcal per kg of body weight is suggested in patients with multiple comorbidities over 65 years and 30 kcal per kg of body weight/day in patients with a much lower average weight and multiple comorbidities. However, these values are indicative and must be adjusted according to the energy intake in older people, nutritional status, physical activity, disease status, and food tolerance.
In patients with severe underweight, the goal of 30 kcal/kg of body weight should be gradually due to the refeeding syndrome.
It is estimated using already established formulas (1 g of protein per kg of body weight in older people) regarding protein needs. However, it must be adjusted according to nutritional status, physical activity, disease status, and food tolerance. The fat and carbohydrate needs are adapted according to the patient’s energy needs in a ratio of 30:70 (people without respiratory deficiency) and 50:50 (ventilated patients).
The use of oral nutritional supplements is recommended to achieve optimal nutritional goals through individualized dietary advice with at least 400 kcal/day, including 30 g or more protein per day and its continuation for at least one month.
Patients with type II diabetes mellitus, arterial hypertension, and malnutrition should be treated according to nutritional guidelines already established for each pathology, taking into account glucose levels, blood pressure, and caloric intake, respectively.
RESULTS
Chronic diseases of nutritional origin such as diabetes mellitus, hypertension, dyslipidemia, undernourishment, and obesity were observed in patients with SARS-CoV-2. These comorbidities help a better accommodation and progression of this virus in organs such as lungs, intestine, heart, and even brain conditions. Therefore, a general distribution was made with all previously selected articles, obtaining the following percentages (Figure 3): arterial hypertension (40.82%), diabetes mellitus (30.61%), obesity (12.24%), overweight (6.12%), dyslipidemia (6.12%) and undernourishment (4.08%), considering the risk factors in this vulnerable population, as we can see in table 1.
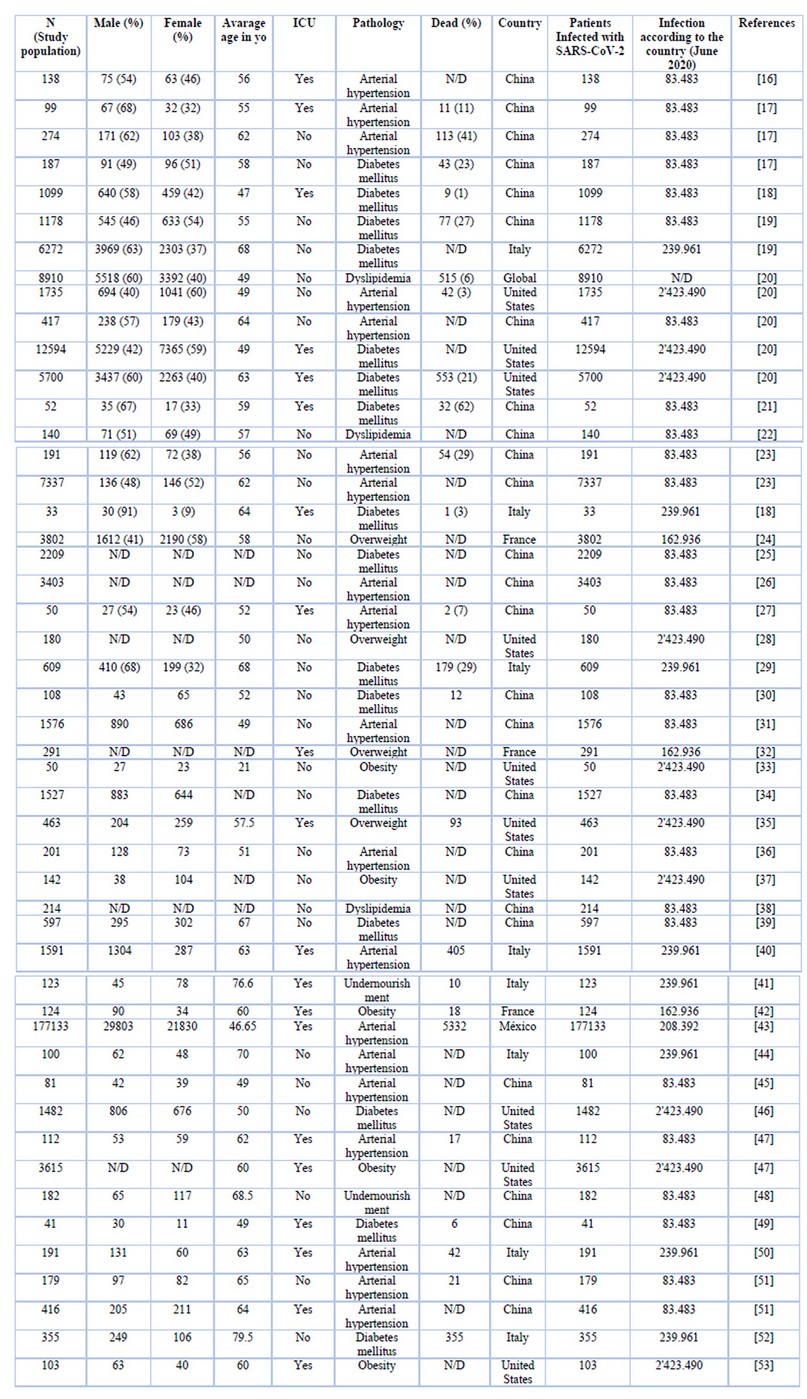
Table 1.- Classification of articles according to variables of interest
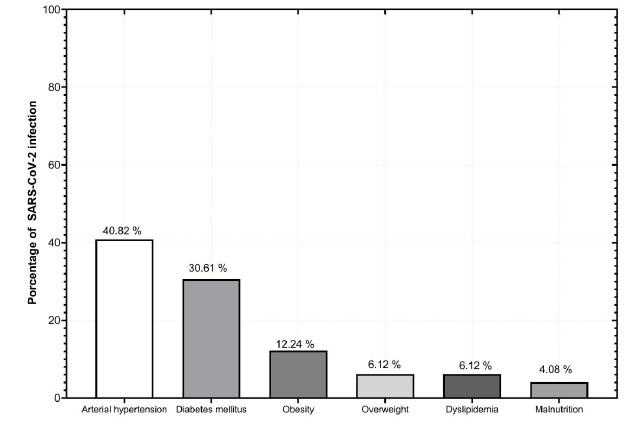
Figure 3.- Chronic diseases identified in patients infected by SARS-CoV-2.
Additionally, information was obtained according to the country of origin (Figure 4), obtaining the following results ordered from highest to lowest respectively: China 26 articles (53.06%), followed by the United States with 10 (20.41%), Italy with 8 (16.33%), France with 3 (6.12%) and articles on par between Mexico and multicenter level with 1 (2.04%) respectively. Likewise, the presence of a higher prevalence in men with SARS-CoV-2 compared to the women analyzed (56% vs. 44%) stands out. The presence of deceased people was not given in all the scientific articles reviewed. However, it can range from two to more than five thousand people (up to 23%). It should be noted that the variable number of deceased persons was later discarded from this analysis due to the little information presented following all the documents chosen.
According to Table II, presented in the supplementary material section, a higher prevalence of individuals who remained stable within the health facility was observed than those admitted to the ICU (29 vs. 20). In the age ranges, the presence of adults stood out, obtaining a total of 34 articles (69.39%), followed by older adults with 8 (16.33%) and finally mixed ages with 7 (14.29%). For its part, the average age was a minimum of 21 years and a maximum of 79 years .
According to Table II, presented in the supplementary material section, a higher prevalence of individuals who remained stable within the health facility was observed than those admitted to the ICU (29 vs. 20). In the age ranges, the presence of adults stood out, obtaining a total of 34 articles (69.39%), followed by older adults with 8 (16.33%) and finally mixed ages with 7 (14.29%). For its part, the average age was a minimum of 21 years and a maximum of 79 years .
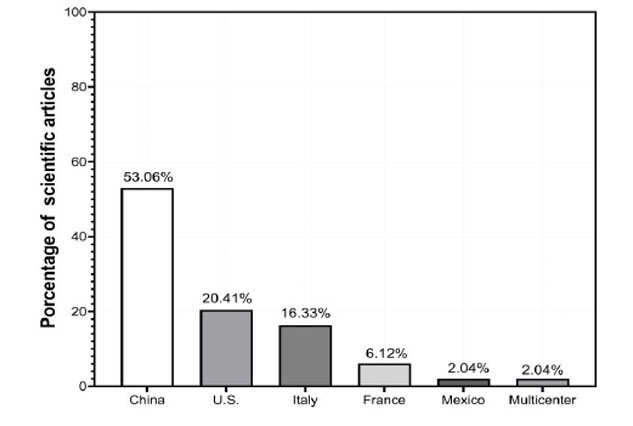
Figure 4.- Scientific articles by country of origin.
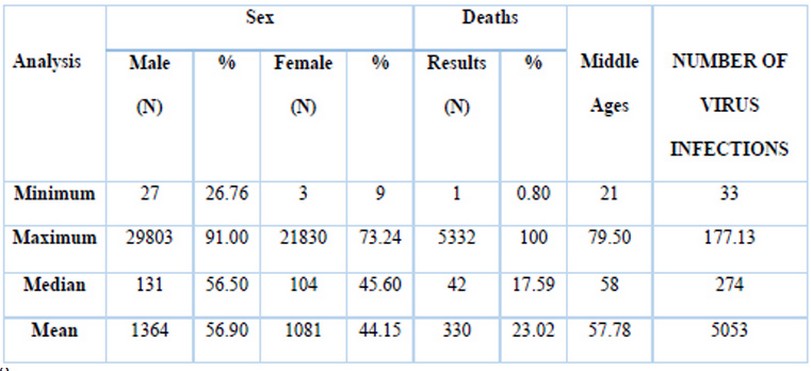
Table 2.- Deaths according to sex and age
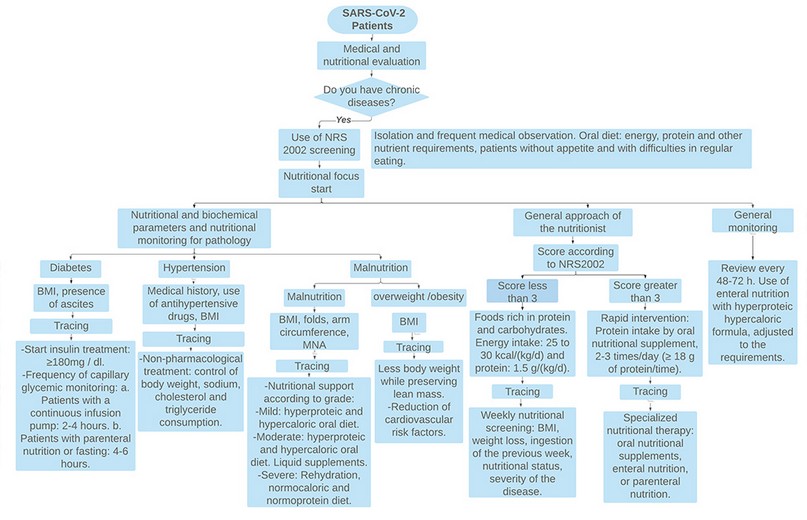
Figure 5. Nutritional Algorithm
The algorithm presented in Figure 5 is composed of nutritional parameters and nutritional monitoring for the pathology of interest according to the presence of SARS-CoV-2 in the individual. Likewise, it presents a general approach by the nutritionist through the Score according to NRS2002, dividing it into a score less than three and a score greater than 3, highlighting the intake of proteins and carbohydrates in the first case and a rapid nutritional intervention through supplementation for the second. In general, specific monitoring is suggested every 48 to 72 hours maximum, adjusting your energy requirements if necessary.
DISCUSSION
This article was developed with Open Access research that had no economic cost at the time of its preparation since all the information was obtained free of charge through high-impact scientific journals.
However, in public health, the generation of additional costs due to the stay in the ICU of public hospitals is estimated, with values ranging between $ 1,000 to $ 3,000 per day, depending on the complications that the patient’s health status presents 13. While in hospitals and private clinics, the prices vary between $ 1,000 to $ 5,000 per day, depending on the establishment, health status, and the care required for their improvement during the first wave in Ecuador 14. For this reason, the consolidated information present in this document is essential, since it is expected to reduce costs in these areas, as well as a greater understanding about the pathologies of nutritional origin present in cases with the SARS-Cov-2 virus, preventing conditions critical health measures in the sick individual and turn, generating an economically viable solution for society.
Table I highlights the strengths and weaknesses found in the previous systematic review obtained from reliable scientific articles such as gender, current information from countries that reported more extensive clinical trials on confirmed coronavirus cases, pathology, number of infected, among others.
Among the weaknesses is the small variety of countries analyzed due to clinical trials not found until the end of this document’s research period and a null contribution by the selected documents about the treatment given to each patient diagnosed with comorbidities SARS-CoV-2.
The indications and guidelines for future research lie in expanding the sample size of scientific articles analyzed, the addition of other comorbidities of nutritional origin as the object of study, and a more generous selection of documents that present the number of people who died SARS-CoV-2 and comorbidities. The percentage of countries analyzed was obtained using the R program version 1.3.1056 using the ggplot2 package with a sector and bar diagram, highlighting China, followed by the United States and Italy. Regarding the age range, the presence of adults (69.39%) and older adults (16.33%) stood out, which were obtained through the previously described program.
According to reviews and subsequent updates in the high-impact literature, it is known that suffering from chronic non-communicable diseases and COVID-19 disease is still high risk, as the CDC mentions the number of times of risk that the person has when suffering one or more NCDs varying between 3 and 5 times the risk of severity[15].
CONCLUSIONS
Comorbidities are considered risk factors in sick individuals with SARS-CoV-2, highlighting hypertension with 40.82%, diabetes with 30.61%, and obesity with 12.24% concerning the total articles analyzed. SARS-CoV-2 affects any age group, highlighting the presence of adults with 69.39%, followed by older adults with 16.33%, according to studies carried out in health centers internationally. Men’s presence was 56% compared to women with 44%, denoting more significant contagion in the male population. The individuals found in the ICU department were 40.82% compared to 59.19% who did not require it due to the timely intervention. Comorbidities can be significantly aggravated if not controlled and under timely medical supervision. Among the weaknesses, incorporating nutritional treatments for each comorbidity and/or specific pathology and the majority incorporation of individuals in the childhood stage stands out for a more significant expansion of the study field. It is recommended to carry out nutritional treatments with other pathologies and with more significant expansion in age ranges, as well as the incorporation of information that it deems appropriate for a better analysis of the situation
Acknowledgments
The authors wish to acknowledge the support of ESPOL, FCV-60-2020, for letting the study be part of the COVID-19 research.
REFERENCES
1. Organizacion Mundial de la Salud O. OMS | Enfermedades crónicas. World Health Organization; 2017.
2. OPS. Las ENT de un vistazo: Mortalidad por enfermedades no transmisibles y prevalencia de sus factores de riesgo en la Región de las Américas. Organización Panamericana de la salud, Washington, D.C. OPS; 2019 Dec.
3. Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Vol. 395, The Lancet. Lancet Publishing Group; 2020. p. 1225–8.
4. Schwartz DA. An Analysis of 38 Pregnant Women with COVID-19, Their Newborn Infants, and Maternal-Fetal Transmission of SARS-CoV-2: Maternal Coronavirus Infections and Pregnancy Outcomes. Arch Pathol Lab Med. 2020 Mar;
5. Fifield K. Cómo la enfermedad COVID-19 afecta los órganos del cuerpo. 2020.
6. South AM, Diz DI, Chappell MC. COVID-19, ACE2, and the cardiovascular consequences. Am J Physiol Circ Physiol. 2020 May;318(5):H1084–90.
7. Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Vol. 395, The Lancet. Lancet Publishing Group; 2020. p. 1417–8.
8. Acosta G, Escobar G, Bernaola G, Alfaro J, Taype W, Marcos C, et al. Original Breve Caracterización De Pacientes Con Covid-19 Grave Atendidos En Un Hospital Treated in a National Referral Hospital in Peru. Rev Peru Med Exp Salud Publica. 2020;2019(2):253–8.
9. Enviroment D of H and. Enfermedades crónicas y COVID-19: lo que necesita saber. 2020.
10. Gandhi RT, Lynch JB, del Rio C. Mild or Moderate Covid-19. N Engl J Med. 2020 Apr;
11. OPS/OMS. Directora de la OPS dice que la lucha contra la pandemia COVID-19 debe incluir atención de enfermedades crónicas - OPS/OMS | Organización Panamericana de la Salud. Organización Panamericana de la la Salud. 2020.
12. Thais M, -Urizarri P, Raúl, Aguilera-Rodríguez, Luis E, Mederos A-. hipertensión, diabetes y enfermedad renal crónica como factores de riesgo para covid-19 grave. I Congreso Virtual de Ciencias Básicas Biomédicas de Granma. 2020.
13. Rodriguez A. El Telégrafo - Noticias del Ecuador y del mundo - Un día en cuidados intensivos cuesta más de $ 1.500. El Telégrafo. 2020.
14. Heredia V, Rosero M. IESS no está derivando a pacientes con covid-19 a clínicas privadas. 2020.
15. Morejón A. Enfermedades Crónicas No Transmisibles Y Covid-19: La Convergencia De Dos Crisis Globales. Scielo. 2020;
16. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA - J Am Med Assoc. 2020 Mar;323(11):1061–9.
17. Cappuccio FP, Siani A. Covid-19 and cardiovascular risk: Susceptibility to infection to SARS-CoV-2, severity and prognosis of Covid-19 and blockade of the renin-angiotensin-aldosterone system. An evidence-based viewpoint. Nutr Metab Cardiovasc Dis. 2020;30:1227–35.
18. Piva S, Filippini M, Turla F, Cattaneo S, Margola A, De Fulviis S, et al. Clinical presentation and initial management critically ill patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in Brescia, Italy. J Crit Care. 2020;58:29–33.
19. Li J, Wang X, Chen J, Zhang H, Deng A. Association of Renin-Angiotensin System Inhibitors with Severity or Risk of Death in Patients with Hypertension Hospitalized for Coronavirus Disease 2019 (COVID-19) Infection in Wuhan, China. JAMA Cardiol. 2020;
20. Mehra MR, Desai SS, Kuy S, Henry TD, Patel AN. Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19. N Engl J Med. 2020 Jun;382(25):e102.
21. Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020 May;8(5):475–81.
22. Zhang J, Dong X, Cao Y, Yuan Y, Yang Y, Yan Y, et al. Clinical characteristics of 140 patients infected with SARS‐CoV‐2 in Wuhan, China. Allergy. 2020 Jul;75(7):1730–41.
23. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 Mar;395(10229):1054–62.
24. de Lusignan S, Dorward J, Correa A, Jones N, Akinyemi O, Amirthalingam G, et al. Risk factors for SARS-CoV-2 among patients in the Oxford Royal College of General Practitioners Research and Surveillance Centre primary care network: a cross-sectional study. Lancet Infect Dis. 2020 Sep;20(9):1034–42.
25. Singh AK, Gupta R, Misra A. Comorbidities in COVID-19: Outcomes in hypertensive cohort and controversies with renin angiotensin system blockers. Diabetes Metab Syndr Clin Res Rev. 2020 Jul;14(4):283–7.
26. Bajgain KT, Badal S, Bajgain BB, Santana MJ. Prevalence of comorbidities among individuals with COVID-19: A rapid review of current literature. American Journal of Infection Control. Mosby Inc.; 2020.
27. Zachariah P, Johnson CL, Halabi KC, Ahn D, Sen AI, Fischer A, et al. Epidemiology, Clinical Features, and Disease Severity in Patients with Coronavirus Disease 2019 (COVID-19) in a Children’s Hospital in New York City, New York. JAMA Pediatr. 2020 Oct;174(10):202430.
28. Garg S, Kim L, Whitaker M, O’Halloran A, Cummings C, Holstein R, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 — Covid-net, 14 states, March 1–30, 2020. Vol. 69, Morbidity and Mortality Weekly Report. Department of Health and Human Services; 2020. p. 458–64.
29. Tedeschi S, Giannella M, Bartoletti M, Trapani F, Tadolini M, Borghi C, et al. Clinical Impact of Renin-angiotensin System Inhibitors on In-hospital Mortality of Patients With Hypertension Hospitalized for Coronavirus Disease 2019. Clin Infect Dis. 2020 Jul;71(15):899–901.
30. Yao Q, Wang P, Wang X, Qie G, Meng M, Tong X, et al. A retrospective study of risk factors for severe acute respiratory syndrome coronavirus 2 infections in hospitalized adult patients. Polish Arch Intern Med. 2020 May;130(5):390–9.
31. Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. prevalence of comorbidities and its effects in coronavirus disease 2019 patients: A systematic review and meta-analysis. Int J Infect Dis. 2020 May;94:91–5.
32. Petrova D, Salamanca-Fernández E, Barranco MR, Pérez PN, Juan Jiménez Moleón J, Sánchez M-J. La obesidad como factor de riesgo en personas con COVID-19: Posibles mecanismos e implicaciones. Atención Primaria. 2020 May;
33. Huang Z, Cao J, Yao Y, Jin X, Luo Z, Xue Y, et al. The effect of RAS blockers on the clinical characteristics of COVID-19 patients with hypertension. Ann Transl Med. 2020 Apr;8(7):430–430.
34. Li B, Yang J, Zhao F, Zhi L, Wang X, Liu L, et al. prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Vol. 109, Clinical Research in Cardiology. Springer; 2020. p. 531–8.
35. Suleyman G, Fadel RA, Malette KM, Hammond C, Abdulla H, Entz A, et al. Clinical Characteristics and Morbidity Associated With Coronavirus Disease 2019 in a Series of Patients in Metropolitan Detroit. Vol. 3, JAMA network open. NLM (Medline); 2020. p. e2012270.
36. Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern Med. 2020 Jul;180(7):934.
37. Roxby AC, Greninger AL, Hatfield KM, Lynch JB, Dellit TH, James A, et al. Outbreak investigation of COVID-19 among residents and staff of an independent and assisted living community for older adults in Seattle, Washington. JAMA Intern Med. 2020 Aug;180(8):1101–5.
38. Zheng KI, Gao F, Wang XB, Sun QF, Pan KH, Wang TY, et al. Letter to the Editor: Obesity as a risk factor for greater severity of COVID-19 in patients with metabolic associated fatty liver disease. Metabolism. 2020 Jul;108:154244.
39. Wei X, Zeng W, Su J, Wan H, Yu X, Cao X, et al. Hypolipidemia is associated with the severity of COVID-19. J Clin Lipidol. 2020 May;14(3):297–304.
40. Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline Characteristics and Outcomes of 1591 Patients Infected with SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA - J Am Med Assoc. 2020 Apr;323(16):1574–81.
41. Doglietto F, Vezzoli M, Gheza F, Lussardi GL, Domenicucci M, Vecchiarelli L, et al. Factors Associated with Surgical Mortality and Complications among Patients with and without Coronavirus Disease 2019 (COVID-19) in Italy. JAMA Surg. 2020 Aug;155(8):691–702.
42. Simonnet A, Chetboun M, Poissy J, Raverdy V, Noulette J, Duhamel A, et al. High Prevalence of Obesity in Severe Acute Respiratory Syndrome Coronavirus‐2 (SARS‐CoV‐2) Requiring Invasive Mechanical Ventilation. Obesity. 2020 Jul;28(7):1195–9.
43. Bello-Chavolla OY, Bahena-López JP, Antonio-Villa NE, Vargas-Vázquez A, González-Díaz A, Márquez-Salinas A, et al. Predicting Mortality Due to SARS-CoV-2: A Mechanistic Score Relating Obesity and Diabetes to COVID-19 Outcomes in Mexico. J Clin Endocrinol Metab. 2020 Aug;105(8):2752–61.
44. Moriconi D, Masi S, Rebelos E, Virdis A, Manca ML, De Marco S, et al. obesity prolongs the hospital stay in patients affected by COVID-19, and may impact on SARS-COV-2 shedding. Obes Res Clin Pract. 2020 May;14(3):205–9.
45. Engin AB, Engin ED, Engin A. Two important controversial risk factors in SARS-CoV-2 infection: Obesity and smoking. Vol. 78, Environmental Toxicology and Pharmacology. Elsevier B.V.; 2020. p. 103411.
46. Finer N, Garnett SP, Bruun JM. COVID‐19 and obesity. Clin Obes. 2020 Jun;10(3):e12365.
47. Watanabe M, Risi R, Tuccinardi D, Baquero CJ, Manfrini S, Gnessi L. Obesity and SARS-CoV-2: a population to safeguard. Diabetes/Metabolism Research and Reviews. John Wiley and Sons Ltd; 2020.
48. Li T, Zhang Y, Gong C, Wang J, Liu B, Shi L, et al. prevalence of malnutrition and analysis of related factors in elderly patients with COVID-19 in Wuhan, China. Eur J Clin Nutr. 2020 Jun;74(6):871–5.
49. Devaux CA, Rolain JM, Raoult D. ACE2 receptor polymorphism: Susceptibility to SARS-CoV-2, hypertension, multi-organ failure, and COVID-19 disease outcome. Vol. 53, Journal of Microbiology, Immunology and Infection. Elsevier Ltd; 2020. p. 425–35.
50. Tsioufis C, Dimitriadis K, Tousoulis D. The interplay of hypertension, ACE-2 and SARS-CoV-2: Emerging data as the “Ariadne’s thread” for the “labyrinth” of COVID-19. Vol. 61, Hellenic Journal of Cardiology. Hellenic Cardiological Society; 2020. p. 31–3.
51. Brojakowska A, Narula J, Shimony R, Bander J. Clinical Implications of SARS-CoV-2 Interaction With Renin Angiotensin System. J Am Coll Cardiol. 2020 Jun;75(24):3085–95.
52. Iaccarino G, Borghi C, Cicero AFG, Ferri C, Minuz P, Muiesan ML, et al. Renin-Angiotensin System Inhibition in Cardiovascular Patients at the Time of COVID19: Much Ado for Nothing? A Statement of Activity from the Directors of the Board and the Scientific Directors of the Italian Society of Hypertension. High Blood Press Cardiovasc Prev. 2020 Apr;27(2):105–8.
53. Kalligeros M, Shehadeh F, Mylona EK, Benitez G, Beckwith CG, Chan PA, et al. Association of Obesity with Disease Severity Among Patients with Coronavirus Disease 2019. Obesity. 2020 Jul;28(7):1200–4.
Received: 16 April 2021
accepted: 10 July 2021
Johanna Pilay Bajaña1, Evelyn Ramírez Carguacundo1, María José Vizcaino Tumbaco2, Daniel Silva-Ochoa 1,2, Davide Di Grumo3, Luis Dorado-Sanchez4, Silvia Orellana-Manzano3, Patricia Manzano1,5, Andrea Orellana-Manzano1,2,3*
1 ESPOL Polytechnic University, Facultad de Ciencias de la Vida (FCV), Campus Gustavo Galindo, Km. 30.5 vía Perimetral, P.O. Box 09-01-5863, Guayaquil, Ecuador.
2 ESPOL Polytechnic University, Laboratory for Biomedical Research, Facultad de Ciencias de la Vida (FCV), Campus Gustavo Galindo Km 30.5 vía Perimetral, P.O. Box 09-01-5863, Guayaquil, Ecuador.
3 Escuela de Odontología, Universidad Espíritu Santo, Ecuador
4Hospital General Monte Sinatí, Guayaquil, Ecuador.
5ESPOL Polytechnic University, Escuela Superior Politécnica del Litoral, ESPOL, Centro de Investigaciones Biotecnológicas del Ecuador (CIBE), Campus Gustavo Galindo Km. 30.5 Vía Perimetral, P.O. Box 09-01-5863, Guayaquil, Ecuador
Corresponding author: Andrea Orellana Manzano, Address: Campus Gustavo Galindo Km 30.5 vía Perimetral, P.O. Box 09-01-5863, Guayaquil, Ecuador, email: [email protected]
