2023.08.02.67
Files > Volume 8 > Vol 8 No 2 2023
Estimate of the most common bacteria cause of UTI and
effective drug in Alrefaai City

Murtadha
A. Al‑khegane1,*, Wisam Jasim Abed Ali2, Zainab Ashour3,
Dip Turki Ibrahim4, Murtadha K. Najim5, Qais R. Lahhob6,*
1 Department of Pathological
Analysis, College of Science, University of Sumer, Dhi Qar, Alrefaai, Iraq.
2 Department of Pathological
Analysis, College of Science, University of Sumer, Dhi Qar, Alrefaai, Iraq.
3 Department of Pathological
Analysis, College of Science, University of Sumer, Dhi Qar, Alrefaai, Iraq.
4 AlRifaai General
Hospital. Iraq.
5 AlRifaai General
Hospital. Iraq.
6 National University of
Science and Technology, Nasiriyah, Iraq.
*
Correspondence: [email protected],
[email protected].
Available
from: http://dx.doi.org/10.21931/RB/2023.08.02.67
ABSTRACT
Background:
Urinary Tract Infection is a worldwide prevalence disease that infects both
males and females in different ratios. Escherichia coli is the most infectious
pathogen, followed by Klebsiella and Pseudomonas. Through time bacteria
increase their resistance to most antibiotics, increasing bacterial prevalence
and pathogenesis. Fifty patients with UTI symptoms were randomly selected in
Alrefaai Hospital from October 2021 to April 2022. A 10-15 ml urine sample was
collected from each patient and cultured to calculate colony forming unit and detect
the type of bacteria with biochemical tests. Most patients were female 66%
compared to male 34% with age groups 1-30 years 68% and those more than other
groups. Escherichia coli is the most prevalent, 54%, while the second one is
Staphylococcus aureus 20%, then Coagulase -ve Staphylococcus 14% and less
infection was with Klebsiella and Proteus, 6%. Antibiotic Imipenem,
Chloramphenicol, Gentamycin, Norfloxacin, Ciprofloxacin and Tobramycin play
highly effective roles on most bacteria. We found that most patients with UTI were
from the city center and in the age group 1-30 years. The most prevalent
pathogens of UTI were Escherichia coli and then Staphylococcus aureus.
Almost Imipenem,
Chloramphenicol,
Gentamycin,
Norfloxacin,
Ciprofloxacin and
Tobramycin
are the best effective antibiotics against our study's
bacteria.
Keywords: Urinary
Tract Infection, Recurrent UTI, Alrefaai city, Antibiotic susceptibility.
INTRODUCTION
Urinary tract infections (UTIs) are severe public health
caused by a variety of pathogens with topping bacterial infections in community
practice; bacterial infections have a high incidence of morbidity and financial
cost 1,2. UTI is a worldwide
disease affecting both males and females in different ratios, especially those
between 50 and 70. In the Iraqi population, the prevalence rate is 23% for all
infections 2. The female is more commonly infected than the male,
which puts it at risk of UTI because the female urethra is physically less efficient
at blocking the bacterial entrance, also short of the urethra that eases trans bacteria
from the anus to the urinary system 3, 1. Many risk factors have a role
in increasing the average of infections like diabetic mellitus, hospitalization,
pregnancy, hospitalization and stone 4,5; also, neonates with
bacteremia are considered as one of the risk groups because of loss of the
ability to speak, so parents report fever, lethargy, irritability, poor feeding
or vomiting 6. UTIs can affect the lower urinary tract, as well as
the upper urinary tract in some cases. The lower UTI infection is called
cystitis, which is characterized by symptoms such as dysuria, frequency,
urgency, and suprapubic soreness without chills, fever, or back pain. 7,
while Symptoms of pyelonephritis, such as loin pain, flank discomfort, fever,
or other indicators of a systemic inflammatory reaction, are familiar with
upper UTI 8.
The most common pathogenic infectious of the urinary
tract is the bacteria in both types' Gram-positive and Gram-negative; the most
responsible genus for UTIs infections within Gram-negative is Escherichia
coli,
followed by Klebsiella, Pseudomonas, and Proteus
spp. While the gram-positive groups are Staphylococcus spp and Streptococcus
spp.9. Sometimes, no growth of bacteria appears in the bacterial
culture of urine despite clinical manifestation and appearing of pus in urine
above the normal range; this reflects many influences like using of Antibiotics
less than 3 days before sample collection, Mycobacterial infection, Viral
infection, Parasite infection and Fungal infection. 10,11. The
antibiotic resistance of bacteria is worldwide; some patients use different
types of antibiotics without medical consultation, others start treatment with
highly effective antibiotics at younger age, and some patients use the drug in a
short time12,13. All of these factors facilitate bacterial
development and then increase the mechanism of resistance to antibiotics. We
aimed to estimate of most prevalent bacteria and the most effective antibiotics
on the bacteria.
MATERIAL AND METHOD
Patients
Urine samples were collected from
50 patients with recurrent symptoms of UTI (most of them with upper UTI); a random
selection of patient's gender and age was in
Alrefaai Hospital from October 2021 to April 2022, and all of them resisted
some antibiotics used at the past without healing. The physician sent them to
the laboratory to detect the best choice of antibiotic. The patients stopped
using antibiotics less than 3 days before urine collection—patients' data such as
name, age and address in central or peripheral of Alrefaai city.
Culture
Midstream random urine samples (10 - 15 mL) were
collected in sterile disposable containers and transferred to the Microbiology
Laboratory of Alrefaai Hospital for culture.
To record the colony-forming units (CFUs) of
bacteria in the urine sample manually, bacterial strains were isolated through
serially diluting urine samples and spreading on CLED (cystine-lactose-electrolyte
deficient) agar then incubated at 37 C for 24 h in an incubator. The colony
count cultures ≥ 105CFU/ml were considered
significant and included in the study. Colonies were purified using the
multiple-streak method and preserved in glycerol stock at -20C for further
culturing and characterization experiments.
Preserved and cultured colony was cultured on Blood,
and MacConkey agar was prepared according to the manufacturer
company (Himedia) 's instruction to differentiate between Gram-positive and
Gram-negative bacteria; also, some chemical and biological tests were done to distinguish between
bacterial genera.
The antibacterial susceptibility testing of the
isolate samples was done using the Kirby-Bauer disk diffusion method 14
on Mueller Hinton agar after streaking of bacteria on its surface; the
antibiotics containing discs were from Oxoid.
RESULTS
Of fifty patients there are (66%) were female, and
most were in both age groups, 1-15 years and 16-30 years, male was (34%) and
also distributed in the same age group. Patients from the center of the city were
(78%) while the other (22%) from the Peripheral appear in Table 1.
Central patients were distributed within the 16-30 years
age group more than other groups, and the less group was the 31-45 years
contain 3 patients; peripheral patients were distributed within the 1-15 years
age group more than others and not there any patient within 61-75 years.
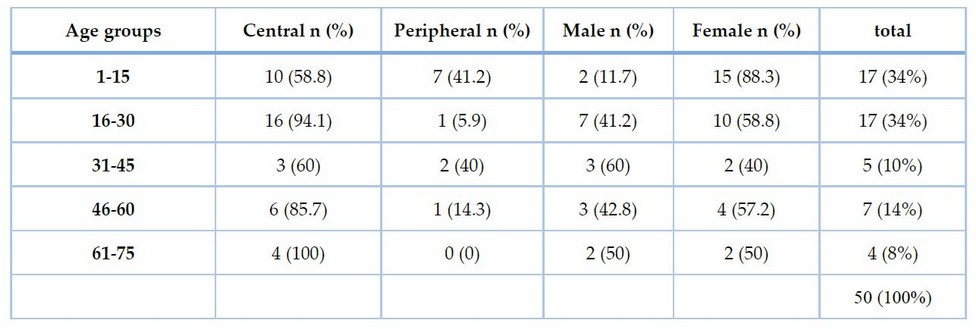
Table
1.
Selected socio-demographic characteristics and gender of patients with UTI
E.coli is the most prevalent infected
pathogen that causes UTI in Alrefaai city with ratio (54%); the second one is Staphylococcus
aureus (20%), then Coagulase -ve
Staphylococcus (14%) while less infected
is Klebsiella and Proteus (6%) as appear in Figure 1.
Of central patients, 39 are (46%) infected with E.Coli
and (23%) with Coagulase-negative Staphylococcus. Spp compared to mostly
peripheral patients (82%) infected with E.Coli. Not there mix growth observed
in our samples.
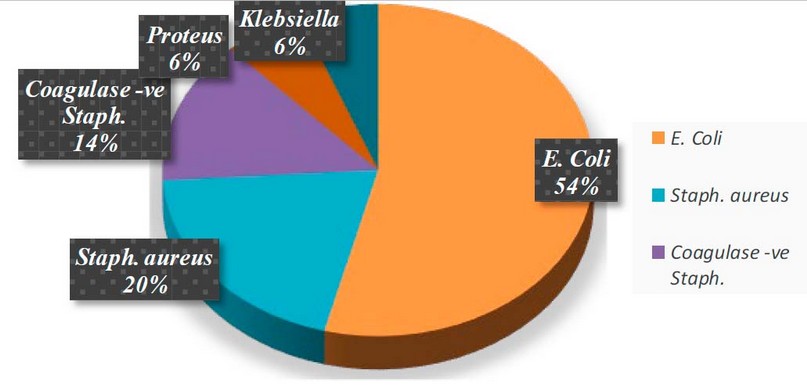
Figure
1. Type
of bacteria in UTI infection
Table 2 describe the age groups
of patients and show up the age group 1-15 years and 16-30 years more infected
than other groups (34%) for each group, also all types of bacteria in our
research and all Proteus present in childhood age group 1-15 years.
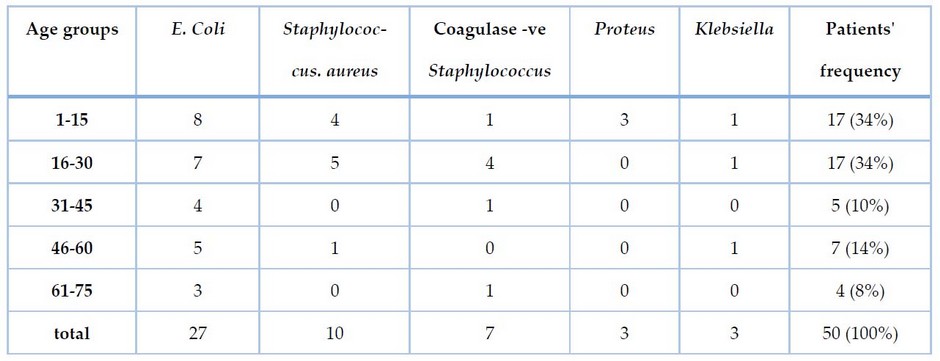
Table
2.
Frequency Distribution of bacterial infection of the urinary system according
to age groups.
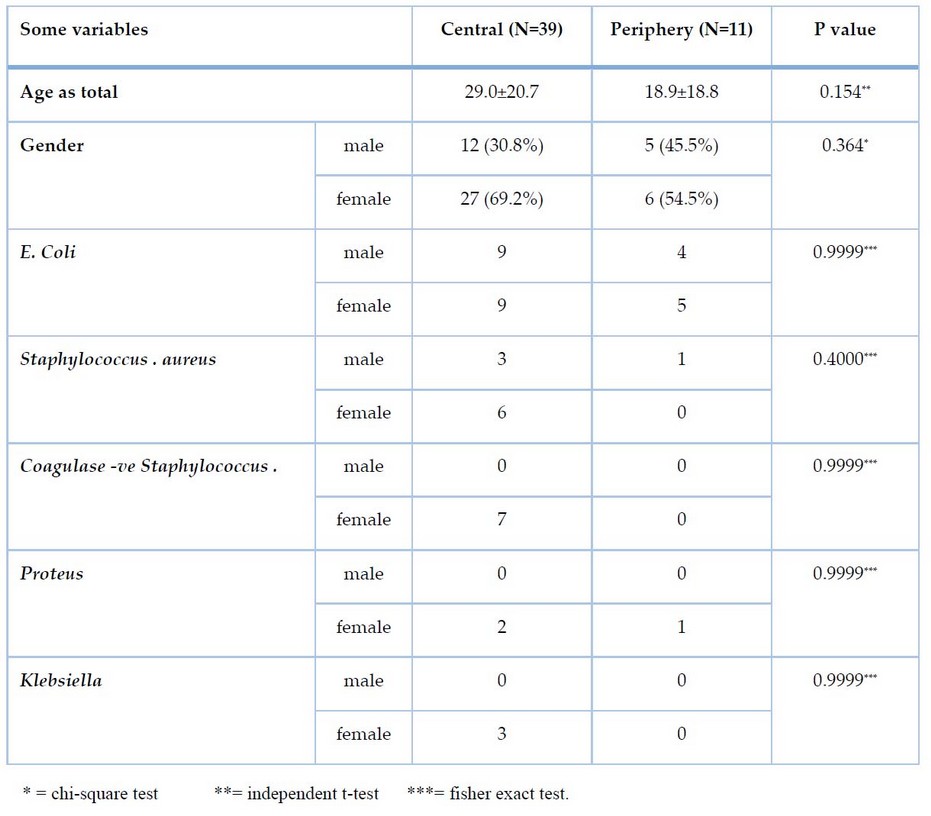
Table
3. Distribution
and comparison of bacteria and patients' Age and Gender to Central and
periphery groups.
Female distribution was 33 (66%)
more than the male 17 (34%). Not their significant difference between the Male
group of central 12 (30.8%) and periphery 5 (45.5%) from the side and between the
female group from central 27 (69.2%) and periphery 6 (54.5%) from the other side.
Staphylococcus aureus infects females more than males, while Proteus,
Klebsiella and coagulase-negative Staphylococcus spp. Infect only the female in
our study as described in Table 3.
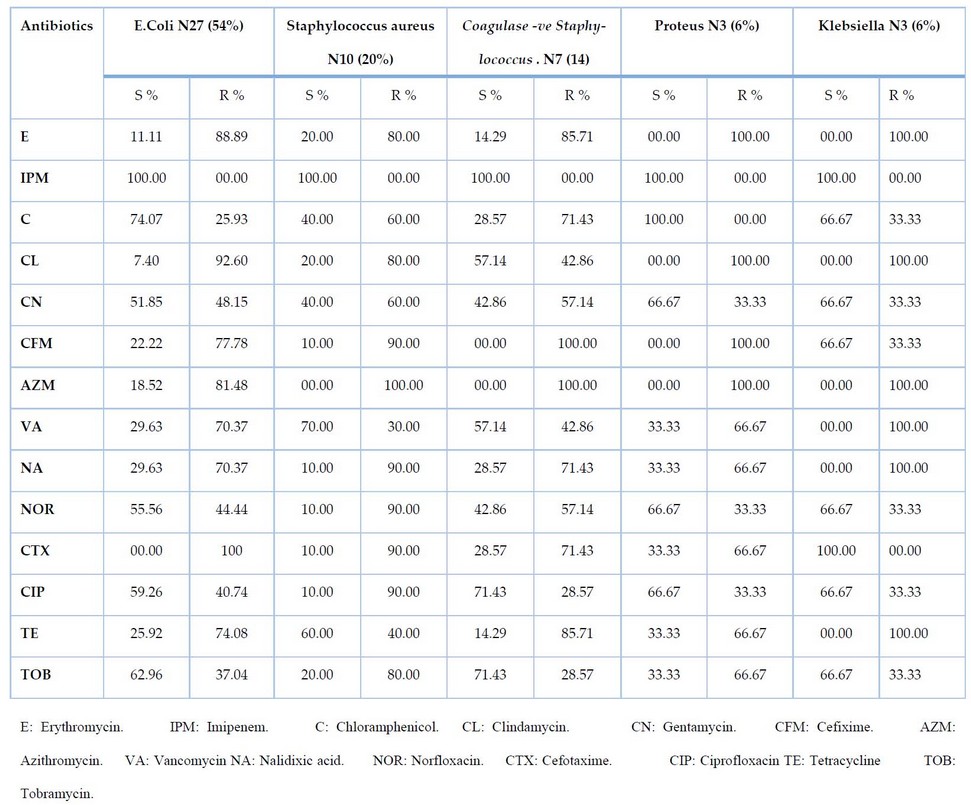
Table
4.
Resistant and susceptibility rate (%) of isolated uro pathogens.
Several
antibiotics resisted by some bacteria, such as E and CL, do not affect Proteus
and Klebsiella, Coagulase -ve staphylococcus gonococcus and Proteus resist CFM
100 %, AZM completely resist by Staphylococcus aureus, Coagulase -ve Staphylococcus
diplococcus, Proteus and Klebsiella. VA, NA and TE also did not affect
Klebsiella, and CTX was 100 % resisted by E.Coli.
Sensitivity
tests to the five types of bacteria appearing in the IPM is the broad spread
spectrum sensitive antibiotic. C, CN and NOR antibiotics affect more than 50%
of isolated bacteria; E.Coli, Proteus and Klebsiella, CIP and TOB affect more
than 50% of E.Coli, Proteus, Klebsiella and Coagulase -ve Staphylococcus. Staphylococcus
aureus is a highly resistant bacteria for most antibiotics but is sensitive to more
than 50% of samples for just VA and TE.
Some
antibiotics with shallow sensitivity effects, such as AZM, have less effect on
only E.coli (18.52%), while the resistance from all other bacteria, E and NA
appear with a low sensitivity spectrum on all types of bacteria.
DISCUSSION
This
study provides information about the most prevalent bacteria that cause central
and peripheral urinary tract infections in Alrefaai City. Also, please give us
an idea about the most effective antibiotic for the five bacteria in our study.
Females
were more than males in our sample that suffer from UTI 66 % compared to males
34%, and these results were compatible exactly with most studies like 15,16.
Most
UTI patients within age groups 1-15 and 16-30 years, 17% for each one and these
results close to 17 in Nigeria that appear age group patients 74.7%
with UTI 20-50 years and lowest at >50 years age group 10.3%. Conversely, it
differs from the study of 2,18 patients in the age group 41-60 years
59.9% and more than 45 years 64%, respectively. Of patients from the center,
78% were more than peripheral 22%. Patients from the peripheral almost do not
use the antibiotic early, so antibiotics are more effective in the first dose.
From
50 samples of uropathogenic bacterial infection, there are 17 (34%) Gram-positive
and 32 (66%) Gram-negative. This distribution ratio differs from 15,18 9.68%
and 19% for Gram-positive and Gram-negative 90.32% and 81%, respectively.
E.coli is the most prevalent pathogen in our study, and almost other studies
distributed in most age groups 19.
E.coli
was the most prevalent at 54%, while the second was Staphylococcus aureus at 20%,
followed by Coagulase -ve Staphylococcus at 14%. Proteus and Klebsiella
distribution were Less typical at 6%. This result was compatible with 20,2,15
in E.coli distribution but different in the second pathogen, Klebsiella 18.71%
and the low ratio was for Enterobacter spp. In studies of Aboderin in Nigeria and
Prakash in India appear, P.aerogenousa and Klebsiella are the second pathogens
and this difference with our study 21,15.
Periphery
patients infected with E.coli except two; one infected with Staphylococcus aureus
and another with Proteus. In central patients, E.coli is also the most prevalent
infection at 46.1 %.
E.coli
infect both genders in an equal ratio of 23.0% for Central patients; results
from the periphery appear the convergence between male 36.36% and female 45.45%,
and this is compatible with 22 but different with 23,24,15
that appears the ratio of female infected with E.coli more than male.
The
closeness of the urethral meatus to the anus, shorter urethra, sexual
intercourse, incontinence, and improper bathroom habits all contribute to the
increased prevalence of UTI in females 25,15.
Males
have a reduced infection rate due to the length of the urethra, the dry environment
around the meatus, and prostatic fluid's antibacterial qualities 20.
Between
all antibiotics used in this study (IPM) was sensitive (100%) for all pathogens
E. Coli, Staphylococcus aureus, Coagulase -ve Staphylococcus, Proteus and Klebsiella,
this result different with 26,27.
E.coli
is resistant to most antibiotics 28; in our study, it's resistant to
E 88.9%, CL 92.6%, CFM 77.78%, AZM 81.48%, VA 70.37%, NA 70.37%, CTX 100% and
TE 74.08%. This result compatible with 15 and 30 in
resistance of bacteria to NAL, CTX and CIP, CTX, respectively, different in
CIP, TOB, and CTZ that also resistance in study of 15. Also, our
study appears compatible with 5.
Proteus
resist for E 100%, CL 100%, CFM 100%, AZM 100%, VA 66.67%, NA 66.67%, CTX
66.67%, TE and TOB: 66.67%. The results were completely different, with 28
while 20 compatible in TE and a difference in meager resistance for
CN and NA. The study difference in CIP resistance was 58.6 % for Gajdács study 5.
Klebsiella
resists E 100%, CL 100%, AZM 100%, VA 100 %, NA 100 %, TE 66.67%, and this
result appears different from 15 that appear to resist for CIP and
IMP and with 28 in resistance of NA. 30
Staphylococcus
aureus resists E 80%, Cl 80%, CFM 90%, AZM 100%, NA 90%, NOR 90%, CTX 90%, CIP
90% and TOB 80%. This result appears compatible with 29,15 and just
in CTX with 15. Also, the result compatible with 28 in NA
resistance and different in E, CIP, V, CL, CN and C and compatible with Gajdács
5.
Coagulase
-ve Staphylococcus resist for E 85.71%, C 71.43%, CFM 100%, AZM 100%, NA
71.43%, CTX 71.43% and TE 85.71%. This result is compatible with 28
in E and NA resistance and different in CIP, V, CL, CN and C. Our Result is compatible
with 20 in TE and different in CN, NA, and C, which are less sensitive.
There
are significant etiological variables that increase the risk of Multiple
Drug Resistance (MDR) infections, including the use of broad-spectrum
antibiotics inappropriately (without investigation of antibiotic resistance),
Lack of infection control strategies 28, poor hygiene,
immunosuppression, and a prolonged stay in the hospital 31.
Low
birth weight, premature delivery, cystitis, and pyelonephritis are all possible
side consequences of untreated recurrent UTI 32.
CONCLUSION
Our
study is the first one in Alrefaai City central and peripheral, estimating the
most prevalent bacterial pathogens and antibiotic sensitivity. We found that most of the patients with UTI were from the
city center and in the age group 1-30 years. The most prevalent bacteria were E.coli
and then Staphylococcus aureus. IPM, C, CN, NOR, CIP and TOB is the best
effective antibiotic against all bacteria in our study.
REFERENCES
1.
Ikram,
Rosemary, Rebecca Psutka, Alison Carter, and Patricia Priest. "An Outbreak
of Multi-Drug Resistant Escherichia Coli Urinary Tract Infection in an Elderly
Population: A Case-Control Study of Risk Factors." BMC Infectious
Diseases. 2015; 15(1): 1–7. http://dx.doi.org/10.1186/s12879-015-0974-0.
2.
Majeed,
Heba Takleef, and Ahmed Abduljabbar Jaloob Aljanaby. "Antibiotic
Susceptibility Patterns and Prevalence of Some Extended Spectrum
Beta-Lactamases Genes in Gram-Negative Bacteria Isolated from Patients Infected
with Urinary Tract Infections in Al-Najaf City, Iraq." Avicenna journal
of medical biotechnology. 2019; 11(2): 192.
3.
Al-Bazy,
F. I. .; Abdulateef, S. M. .; Sulimn, B. F. . Impact Of Feeds Containing
Optifeed®, Vêo® Premium, And Oleobiotec®. On The Lipid Peroxidation Of Male
Broilers Under Heat Stress. JLSAR 2022, 3, 25-31.
4.
Foxman,
Betsy. "Urinary Tract Infection Syndromes: Occurrence, Recurrence,
Bacteriology, Risk Factors, and Disease Burden." Infectious Disease
Clinics. 2014; 28(1): 1–13.
5.
Gajdács,
Márió, Marianna Ábrók, Andrea Lázár, and Katalin Burián. "Urinary Tract
Infections in Elderly Patients: A 10-Year Study on Their Epidemiology and
Antibiotic Resistance Based on the Who Access, Watch, Reserve (Aware)
Classification." Antibiotics. 2021; 10(9).
6.
Kaufman,
Jonathan, Meredith Temple-Smith, and Lena Sanci. "Urinary Tract Infections
in Children: An Overview of Diagnosis and Management." BMJ paediatrics
open. 2019; 3(1).
7.
Pallett,
Ann, and Kieran Hand. "Complicated Urinary Tract Infections: Practical
Solutions for the Treatment of Multiresistant Gram-Negative Bacteria." Journal
of antimicrobial chemotherapy. 2010; 65(suppl_3): iii25–33.
8.
Buettcher,
Michael et al., “Swiss Consensus Recommendations on Urinary Tract Infections in
Children of the Kidney and Urinary Tract CFU Colony Forming Units CRP C-Reactive
Protein ESBL Extended-Spectrum Beta-Lactamase MCUG Micturition Cystourethrogram
MDR Multi Drug Resistant.” European Journal of Pediatrics, 2021; 180:
663–74. https://doi.org/10.1007/s00431-020-03714-4.
9.
Ahmed,
Syed Suhail et al., "Uropathogens and Their Antimicrobial Resistance
Patterns: Relationship with Urinary Tract Infections." International
Journal of Health Sciences. 2019; 13(2): 48.
10.
Bennett,
John E, Raphael Dolin, and Martin J Blaser. Mandell, Douglas, and Bennett's
Principles and Practice of Infectious Diseases E-Book. Elsevier Health
Sciences. 2019.
11.
Wesley,
W Emmons. "Urinary Tract Infection, Females." Med J . 2002;3:
33–41.
12.
Freitas,
Ana R, Tomasz M Karpiński, and Bingyun Li. "Antimicrobials and Anticancers
of Bacterial Origins." Frontiers in Microbiology, 2020; 11:
842.
13.
Olubukola,
O, A Olubusola, and F Kehinde. "Evaluation of Use of Antibiotic without
Prescription among Young Adults." African Journal of pharmacy and
pharmacology. 2010; 4(10): 760–62.
14.
Hudzicki,
Jan. "Kirby-Bauer Disk Diffusion Susceptibility Test Protocol." American
society for microbiology. 2009; 15: 55–63.
15.
Prakash,
Devanand, and Ramchandra Sahai Saxena. "Distribution and Antimicrobial
Susceptibility Pattern of Bacterial Pathogens Causing Urinary Tract Infection
in Urban Community of Meerut City, India." International scholarly research
notices, 2013a.
16.
Sood,
Smita, and Ravi Gupta. "Antibiotic Resistance Pattern of Community
Acquired Uropathogens at a Tertiary Care Hospital in Jaipur, Rajasthan." Indian
journal of community medicine: official publication of Indian Association of
Preventive & Social Medicine. 2012; 37(1): 39.
17.
Omigie,
Orhiosefe, Lawrence Okoror, Patience Umolu, and Gladys Ikuuh. "Increasing
Resistance to Quinolones: A Four-Year Prospective Study of Urinary Tract Infection
Pathogens." International Journal of General Medicine. 2009;
2: 171.
18.
Tektook,
Nihad Khalawe, Khalid Ibrahim Al-Lehibi, and Raad K Al-Husseinei. “Prevalence
Some Pathogenic Bacteria Causing Uti in Diabetic Patients in/Specialized Center
for Endocrinology and Diabetes of Baghdad City–Iraq.” Medical Journal of
Babylon. 2017; 14(2): 260–66.
19.
Kahlmeter,
G. "An International Survey of the Antimicrobial Susceptibility of
Pathogens from Uncomplicated Urinary Tract Infections: The ECO· SENS Project."
Journal of antimicrobial Chemotherapy. 2003; 51(1): 69–76.
20.
Abubakar,
El-Mahmood Muhammad. "Antimicrobial Susceptibility Pattern of Pathogenic
Bacteria Causing Urinary Tract Infections at the Specialist Hospital, Yola,
Adamawa State, Nigeria." Journal of clinical medicine and research.
2009; 1(1): 1–8.
21.
Aboderin,
Oladipo A, Abdul-Rasheed Abdu, Babatunde W Odetoyin, and Adebayo Lamikanra. "Antimicrobial
Resistance in Escherichia Coli Strains from Urinary Tract Infections." Journal
of the national medical association. 2009; 101(12): 1268–73.
22.
Lipsky,
Benjamin A. "Prostatitis and Urinary Tract Infection in Men: What's New;
What's True?" The American journal of medicine. 1999; 106(3):
327–34.
23.
Nys,
S. "Antibiotic Resistance and the Commensal Flora." Microbiology:
142. 2005.
24.
Nys,
Sita, T Van Merode, A I M Bartelds, and E E Stobberingh. "Urinary Tract
Infections in General Practice Patients: Diagnostic Tests versus
Bacteriological Culture." Journal of Antimicrobial Chemotherapy, 2006;
57(5): 955–58.
25.
Manjula,
N G et al. "Incidence of Urinary Tract Infections and Its Aetiological
Agents among Pregnant Women in Karnataka Region." Advances in Microbiology,
2013.
26.
Alipourfard,
Iraj, and Nilufar Yeasmin Nili. "Antibiogram of Extended Spectrum
Beta-Lactamase (ESBL) Producing Escherichia Coli and Klebsiella Pneumoniae
Isolated from Hospital Samples." Bangladesh Journal of Medical
Microbiology, 2010; 4(1): 32–36.
27.
Mangaiarkkarasi,
A, R M Ali, and R Gopal. "Study of Antimicrobial Susceptibility Pattern of
Escherichia Coli Isolated from Clinical Specimens in a Teaching Hospital, Pondicherry."
Research Journal of Pharmaceutical, Biological and Chemical Sciences, 2013;
4(1): 1365–71.
28.
Ranjbar,
Reza, Ashtiani M T Haghi, Jafari N Joneydi, And M Abedini. "The Prevalence
And Antimicrobial Susceptibility Of Bacterial Uropathogens Isolated From Pediatric
Patients." 2009.
29.
Folliero,
Veronica et al., "Prevalence and Antimicrobial Susceptibility Patterns of
Bacterial Pathogens in Urinary Tract Infections in University Hospital of
Campania' Luigi Vanvitelli' between 2017 and 2018." Antibiotics. 2020;
9(5): 215.
30.
Asmat,
Umema, Muhammad Z Mumtaz, and Arif Malik. "Rising Prevalence of
Multidrug-Resistant Uropathogenic Bacteria from Urinary Tract Infections in
Pregnant Women." Journal of Taibah University Medical Sciences. 2021;
16(1): 102–11.
31.
Manjunath,
G N, R Prakash, and Kiran Shetty Vamseedhar Annam. "Changing Trends in the
Spectrum of Antimicrobial Drug Resistance Pattern of Uropathogens Isolated from
Hospitals and Community Patients with Urinary Tract Infections in Tumkur and
Bangalore." Int J Biol Med Res. 2011; 2(2): 504–7.
32.
LeFevre,
Michael. "Urinary Tract Infections during Pregnancy." American
family physician. 2000; 61(3): 713–20.
33.
Al-Taha,
N K. "The Role of Gram-Negative Bacteria in Hospital Infections." 2000.
34.
Prakash,
D., & Saxena, R. S. "Distribution and Antimicrobial Susceptibility
Pattern of Bacterial Pathogens Causing Urinary Tract Infection in Urban
Community of Meerut City, India." ISRN Microbiology, 2013: 1–13.
Received: May 15, 2023/ Accepted: June 10, 2023 / Published:
June 15, 2023
Citation: Al‑Khegane, M.A.; Abed Ali, W.J.; Ashour, Z.; Ibrahim, D.T.; Najim, M.K.; Lahhob , Q.R. Estimate of the most common bacteria cause of
UTI and effective drug in Alrefaai City. Revis Bionatura 2023;8 (2) 67. http://dx.doi.org/10.21931/RB/2023.08.02.67