2022.07.02.54
Files > Volume 7 > Vol 7 No 2 2022
Jaleel Hussien Hammoodi Al obaidi 1,*
1 Department of surgery, Alshafah private Hospital Diyala Government Medical Director Iraq;
orcid.org/0000-0002-7993-5524
* Correspondence: [email protected]; Tel.: 009647722221381
Available from: http://dx.doi.org/10.21931/RB/2022.07.02.54
ABSTRACT
Abdominal hydatid cyst rupture is one of the critical situations which challenged the surgeon incidentally during explorative lobotomy for acute abdominal conditions. It is considered an endemic area for hydatid disease. To study and evaluate different modalities of surgical treatments used to deal with the incidental rupture of abdominal hydatid cyst. Patient and methodology: Patients (n=200) underwent surgical treatment for abdominal hydatid cysts in Al -Kindy teaching Hospital and Diala private hospital. A review was carried out from January 1996 to January 2006. About 18 patients (6%) had a rupture of abdominal hydatid cyst; in 15 patients (83.3%), the rupture was discovered incidentally during surgery for urgent acute abdomen, and 3 patients (16.7%) were detected clinically and using ultrasound. The median age was 32 years, and the female to male ratio was 2:1. 17 patients presented with signs & symptoms of acute abdomen. 11 patients presented with hypovolaemic shock after trauma to the liver (RTA in 9 patients, anaphylactic shock in 1 patient, allergic reaction in 1 patient). 4 patients presented with spontaneous rupture, 2 presented with secondary hydatidosis, and 1 presented with haematuria. Results: Twelve females and six males were affected. Rupture of abdominal hydatid cyst was diagnosed in only three patients by history, clinical examination, and ultrasound. At the same time, the other 15 patients were diagnosed during surgery. The mean hospital stay was 14 days. About 5 patients developed post-operative complications, i.e., wound infection (n=1), stress ulceration in the duodenum (n=1), subphrenic abscess (n=1), an infected remnant of hepatic hydatid cyst cavity (n=1), and recurrence of the hydatid cyst (n=1). Unfortunately, intra-operative mortality was recorded in 1 patient. The clinical diagnosis is usually tricky, but ultrasonography is an excellent initial diagnosis in suspected cases.
Keywords: Surgical treatment, Incidental Ruptured Abdominal hydatid cyst, Traumatic rupture.
INTRODUCTION
Hydatid disease is caused by Echinococcus granulosus, a common parasitic infestation in Iraq and worldwide. It is still an important and challenging medico-surgical problem in endemic countries like Iraq, Iran, Turkey, Australia, South America, and Europe 1. Generally, hydatid cysts are incidentally diagnosed via radiological assessment for another symptom2. Nevertheless, a few patients may show jaundice, vomiting, nausea, and abdominal pain depending on the hydatid cyst's localization and dimensions of the hydatid cyst2. Internal rupture perforation (intraperitoneal rupture, intrapleural rupture, intrapericardial rupture, bronchopleural fistula, broncho-biliary fistula, rupture into hollow viscous or cysto-biliary fistula), and neighboring organ compression, biliary compression, vascular compression, anaphylactoid reaction, bacterial superinfection or external rupture like cysto-cutaneous fistula are some of the hydatid disease-related complications3-5. The hydatid cyst intraperitoneal rupture is a low and lethal complexity of hydatid disease for which quick treatment and diagnosis are necessary to lower the death rate6, 7.
The primary carriers of hydatid disease in human beings are dogs. Infection can be through direct contact or ingesting ova of the parasite while consuming unwashed and uncooked vegetables or after the digestion of contaminated food. The embryo is released in the intestinal tract and carried to the liver by portal circulation8. The disease may attack every organ in the human body, but the most standard site of infection is the liver, with a rate of 50-70%1. A typical hydatid cyst of the liver is composed of host and parasite tissue. The former (pericyst), formed by the reaction of the liver to the presence of the parasite, is gray in color and thick. The latter (endocyst) is formed of two layers, and an outer laminated layer is formed of the parasite itself. The outer layer is whitish & elastic, and an inner germinal layer consists of the living part of a hydatid cyst. This inner layer internally secretes hydatid fluid, broods capsules scolices and externally consists of the laminated membrane.
Many cysts are asymptomatic or present as a painful mass in the abdomen. The patient may discover cysts during self-examination or by the routine investigation done by the physician. Urgent surgical interventions are required for unexpected problems occurred during laparotomy. Hydatid disease patients used different modes of treatment like medical treatment with albendazole9, ultrasound-guided PAIR (puncture, aspiration, injection, respiration), and albendazol treatment10 Laparoscopic (cystectomy, deroofing and omentoplasty)11. Surgical treatment is the standard treatment of hydatid disease. However, controversy still exists about the selection of different surgical procedures12. In the present study, we have evaluated the efficiency and complications of different modes of surgical treatments used to deal with rupture of abdominal hydatid cyst, which was discovered incidentally.
MATERIALS AND METHODS
Planing of a retrospective analytic study
It is a retrospective analytic study. Patients (n=200) who underwent surgical treatment for abdominal hydatid cysts in Al -Kindy teaching Hospital and Diala private hospital were screened. A review was carried out from January 1996 to January 2006.
Patient distribution
Out of 200, about 18 patients (6%) had rupture of abdominal hydatid cyst, in 15 patients (83.3%) rupture was discovered incidentally during surgery for urgent acute abdomen, and 3 patients (16.7%) were detected clinically and using ultrasound. The median age was 32 years, and the female to male ratio was 2:1 [Twelve females (64.6%) and six males (43.4%)]. About 17 patients presented symptoms of acute abdomen. About 11 patients presented with hypovolaemic shock after trauma to the liver (RTA in 9 patients, anaphylactic shock in 1 patient, allergic reaction in 1 patient). 4 patients presented with spontaneous rupture, 2 presented with secondary hydatidosis, and 1 presented with haematuria.
Operative procedure for patients
There are free intraperitoneal fluids mixed with hydatid cyst material (daughter cysts scolices sucked the fluid, and cystic material was removed). The peritoneal cavity was washed with normal saline followed by a 1% povidone-iodine solution (Figure 1A). Around four patients showed spontaneous intraabdominal rupture due to cyst infection forming, subdiaphragmatic abscess and intraperitoneal abscess represented as peritonitis. In this condition, the cystic rupture cavity was cleaned from infected contents and aspirate of the abscess from the intra-abdominal and sub-hepatic abscess. The peritoneal cavity was washed with normal saline followed by a 1% povidone-iodine solution. The tube drain was inserted inside the cystic cavity and the near hepatic cystic cavity.
Two patients noted secondary hydatidosis (Figures 1B and 1C). In one patient (Figure 1B), around 13 cysts were observed. Unfortunately, one cyst was ruptured due to some trauma before the cystectomy procedure (before hospitalization). The second patient showed four cysts in the intraperitoneal (3 cysts) and pancreas (1 cyst). The cyst was ruptured during the operation. The patient developed uncorrectable anaphylactic shock and died during the operation. Out of 18 patients, one patient showed haematuria due to a football hit on the abdomen. On the right loin, daughter cysts were clinically diagnosed by ultrasound. The patient reported the presence of blood in the urine. The hydatid occupies most renal parenchyma (Figure 1C). Transabdominal nephrectomy was done using the right para-median incision.

Figure 1. (a) Daughter cyst, scoliosis; (b) Secondary hydatidosis; (c) Nephrectomy.
Fifteen cases were diagnosed during explorative laparotomy, and three cases were diagnosed by ultrasound. One patient showed a cyst in the right kidney in these three cases. The second patient showed an allergic reaction after trauma manifested by rash, urticaria and visible swelling on the abdomen (Figure 2A). The ultrasound demonstrated two cysts in the liver, multiple cysts in the peritoneal cavity, and free peritoneal fluid (Figures 2B and 2C). The third patient had a history of surgery for hepatic disease before 3 years. All cystic rupture cavities were operated on according to their size, site and condition.
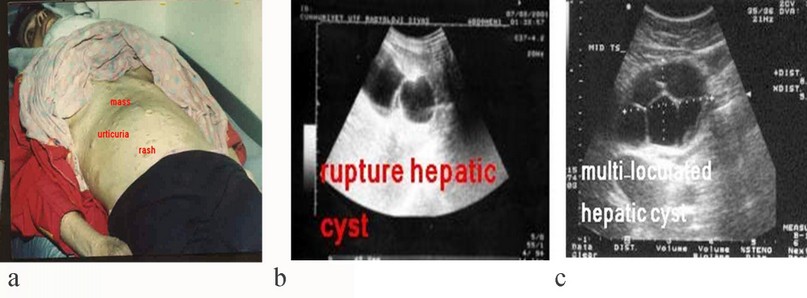
Figure 2. (a) Allergic reaction; (b) Ultrasound showing hepatic rupture cyst; (c) Ultrasound showing the multi-loculated hepatic cyst.
An omentoplasty was carried out for clear fluid cysts (Figure 3A). The bile stain containing cysts was operated with tube drainage (Figure 3B). The infected cyst contents were removed carefully if cystic-biliary communication was observed (Figure 3C). The opening was secured by sutured (synthetic absorbable 2/0 Dexon suture).
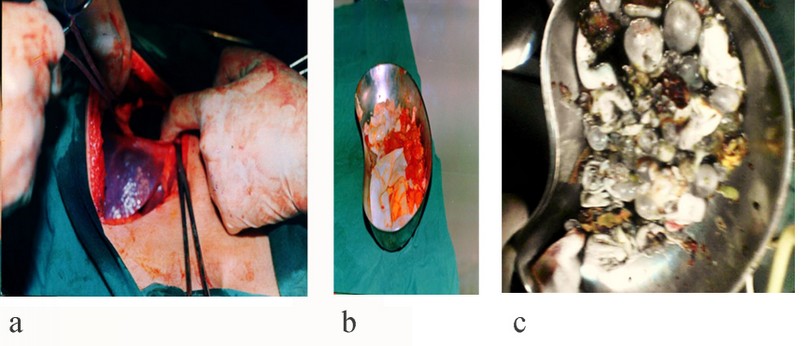
Figure 3. (a) Remnant huge cystic cavity; (b) Bile stain contents; (c) Infected contents.
Partial cystectomy was done for a large hydatid cystic cavity. Total cystectomy was done for extrahepatic or peripheral located hydatid and pedunculated cysts. Non-rupture hydatid cysts were operated on surgically except for one patient. This patient had urticarial. During this patient's surgery, gauze soaked in scolicida agent (10% povidone-iodine) was used to avoid dissemination of the parasite. Around 10-20ml hydatid fluid was aspirated, followed by a 10% povidone iodine injection into the hydatid cyst cavity for 10 min. The pseudocyst (pericyst) was opened. The laminated membrane and daughter cyst was removed by suction and sponging. The cystic cavity was incised between the suture. All cystic elements were evacuated by suction. Before the closure of the abdomen, the peritoneal cavity is clean with povidone-iodine (1%) to kill all scolices and prevent their recurrence. The tube drain was inserted in the peritoneal cavity beside the cyst (Figures 4A and 4B).
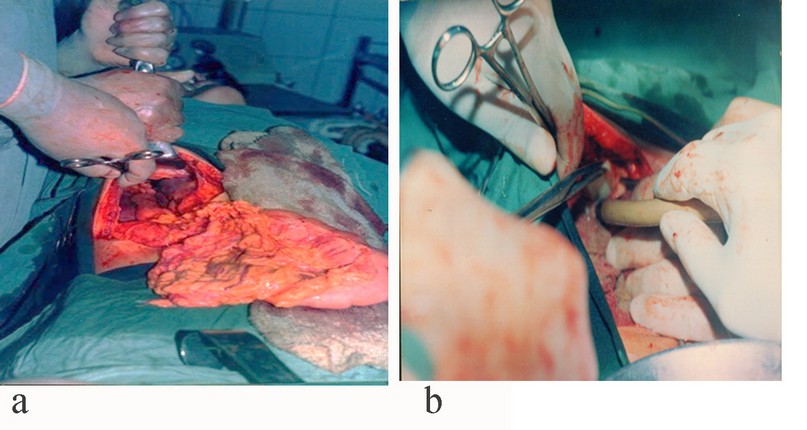
Figure 4. (a) Omentoplasty; (b) Tube drainage.
Post-operative care
All patients were given Albendazole (200 mg) twice a day. Three treatment cycle courses of 112 days were done. Each cycle was about 28 days, followed by 14 days in drug-free intervals.
Patient followup
All patients were followed up for 5 years and invited to attend every 3 months at which clinical examination, ultrasonography, and serological tests (indirect haemagglutinin reaction were performed), which is the only available test in Iraq.
Three patients need urgent reoperation, cyst abscess in one patient, treated by aspiration of the cyst under ultrasound guidance and antibiotics, peritonitis in one patient treated by re-exploration, suction of the peritoneal abscess and toilet with normal saline, and subdiaphragmatic abscess and right pleural effusion in other patient treated by suction of the abscess and chest tube..
RESULTS
Out of 18 patients who presented with symptoms and signs of acute abdomen, only 3 cases were diagnosed preoperatively by ultrasound. The first patient had a history of surgery for hepatic hydatid disease 3 years ago. The second patient presented with haematuria after hitting a football on his abdomen. The third patient presented with rash and urticaria with multiple masses in the abdomen after trauma. Fifteen cases (83.3%) were diagnosed incidentally during explorative laparotomy, and three cases (16.7%) were diagnosed clinically by ultrasound (Table 1).
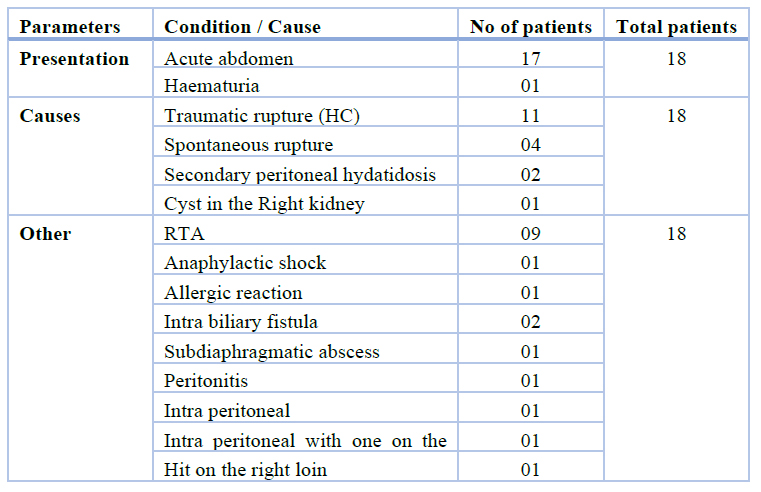
Table 1. Type of Presentation of 18 patients.
In this study period, a total of 48 cysts were treated. Around 30 cysts (62.5%) were found in the liver, while the remaining 18 cysts (37.5%) were found in the extrahepatic region (17 cysts in the intraperitoneal cavity and 1 cyst in the right kidney). In the liver, around 24 cysts (80%) were in the right lobe (size 6-10cm), and 6 cysts (20%) were in the left lobe (size 4-6cm). In the right lobe cysts, 15 cysts (2 were cystic-biliary communication) were ruptured, and 9 cysts were non-ruptured. While, in the left lobe cysts, 1 cyst was ruptured, and 5 cysts were non-ruptured. The localization of the cysts is depicted in Figure 5.

Figure 5. Localization of the cysts.
Omentoplasty was done to operate on 14 cysts that contain clean fluid. Tube drainage of the cystic cavity was carried out in 10 patients (2 bile stain content with cysto-biliary communication and infected cyst in 8 patients). Extrahepatic, peripheral located or pedunculated cyst was operated on with total cystectomy (23 cysts). These cysts were in the peritoneal cavity (17 cysts), in the liver (right lobe 1 cyst and left lobe 4 cysts), and in the right kidney (1 cyst). Hepatomy with selective vascular ligation suture of the inferior vena-cava was carried out in 1 cyst.
Out of 200, around 18 patients (09%) showed spontaneous rupture of hydatid cysts (Table 2). Of these 18 patients, around 12 were female (64.6%), and 6 were male (43.4%). The female to male ratio was 2:1. The mean age group was 36 years and ranged from 12-52 years. Around 16 days of hospital stay were observed.
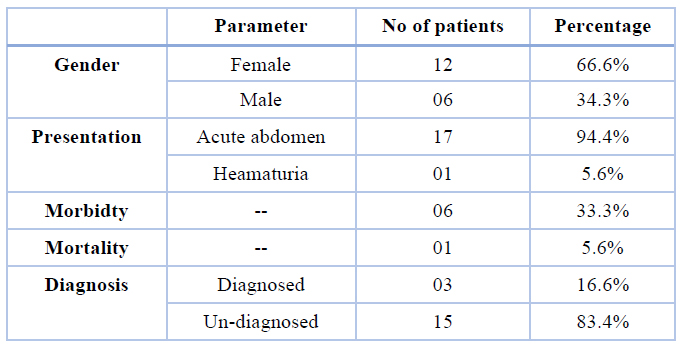
Table 2. The main character of the patients with incidental ruptured hydatid cysts (n=18).
Management was done according to the site, cyst size, and type of complications. Urgent surgical treatment is done after appropriate correction of shock having fluid and electrolyte upsets. Before the closure of the abdomen, irrigation of the peritoneal cavity was done with a povidone-iodine solution of 1%, and post-operative medical treatment was done with Albendazole. Physical examination, ultrasonography, and serological tests were carried out to evaluate the recurrence and symptoms. The recurrence rate was in one case (5.6%), and the duration of follow-up has ranged 2-5 years. Post-operative morbidity occurred in 6 patients (33.3%). These patients showed wound infection (n=1), bleeding on stress ulcer (n=1), pleural effusion with hepatic abscess (n=1), infected cystic cavity (n=1, with tube drain), and peritonitis (n=1) and recurrence of the hepatic cysts (n=1). Out of these 6 patients, 3 patients (with hepatic abscess, infection) required urgently reoperated. The ultrasonography showed a 100% success rate. Echinococcus granulosus was confirmed histologically in all cases.
DISCUSSION
Rupture of hydatid cyst was an urgent surgical condition that needed prompt surgical treatment after resuscitation of the patients. It is a rare complication. The present study shows that female gets more affected than males, and the mean age of patients was 36 years, which was lower than the mean age mentioned by 13. This may occur when female and young patients contact dogs or consume contaminated un-cooked vegetables with the parasite's eggs on the farm and houses in the rural area.
The clinical features of the hydatid disease depend on the site and size and may produce very few symptoms until complications occur. Complications of hydatid disease are traumatic rupture of hydatid cyst, the intraperitoneal release of contents of hydatid cyst (fluid, scolices daughter cyst) into the peritoneum14. Hydatid disease may lead to allergic reactions15, anaphylactic shock and form new cysts (secondary hydatidosis) independent of hepatic cyst16. This also occurs during a previous surgery. This cycle takes several years. Intra biliary spontaneous rupture causes obstructive jaundice and cholangitis17, 18. Sub diaphragmatic and hepatic abscess or spontaneous rupture occurs due to cyst infection. Fever supervenes if there is a secondary bacterial infection, post-operative medical treatment is mandatory in rupture of cysts, and Albendazole is currently the drug of choice19.
Acute abdomen constitutes (94.4%) which is more than explained in a study by Gunay et al.20. Anaphylactic shock (5.6%) and allergic reaction (5.6%) have the same results as another author (27%). Haematuria in 1 patient (5.6%) is a rare presentation. Spontaneous rupture in four patients (27%) is more than explained by Becker et al.21. Patients in rural areas have no facilities to do investigations. Urgent surgical treatment remains the primary treatment of choice in managing complicated hydatid disease. Total cystectomy is the best treatment if possible depending on the location of the cyst and clinical condition of the patient. Tube drainage of the cystic cavity after the evacuation of the cystic contents had complications more than obliteration by omentum, like hepatic abscess and a more extended hospital stay, and this result corresponds with Erguney et al.22. In our opinion, irrigation of the peritoneum with 10% povidone-iodine solution and post-operative medical treatment with Albendazole is the treatment of choice to decrease the incidence of recurrence, which is 5.6% less than explained by Mottaghian and Saidi.23. Trauma causes rupture to the right lobe of the liver and a large cyst more than the left lobe. Spontaneous rupture occurs due to infection of the cyst.
Secondary hydatidosis occurs after the first operation due to the spillage of hydatid fluid. Broods scolices become more extensive in the peritoneum and are usually multiple8. The first operation for hydatid disease is essential. If all cyst material is not cleaned correctly, secondary cyst formation in the liver & peritoneum will be unavoidable.
Pre-operative diagnosis is difficult because patients are generally admitted urgently. For acute abdomen and hypotension, diagnostic ultrasound should be performed initially in the evaluation process as it is fast and has high accuracy. Laboratory tests should be limited as they consume time.
CONCLUSIONS
Spontaneous or traumatic rupture of the liver was found to be rare. It is considered the most severe complication. In the case of acute abdomen, anaphylaxis, or allergic reaction in the endemic region, the diagnosis is tricky, and ultrasonography is suitable for initial investigation in the suspected case. Early diagnosis and urgent surgical treatment reduce the morbidity and mortality associated with this disease. Before the closure of the abdomen, it is irrigated with a sporicidal agent. Surgical treatment of rupture of hydatid cyst is still the treatment of choice. Total cystectomy and omentoplasty are preferred methods with the lowest morbidity rate and acceptable rate of recurrence. The cystic cavity should be managed according to the site, size and contents before the closure of the abdomen. The peritoneal cavity should be irrigated with 1% povidone-iodine solution, and post-operative Albendazole would decrease the incidence of cyst implantation after rupture and secondary hydatidosis development.
Funding: This research received no external funding.
REFERENCES
1. Kumar, A. and T. Chattopadhyay, Management of hydatid disease of the liver. Postgraduate medical journal, 1992. 68(805): p. 853.
2. Yilmaz, M., et al., Liver hydatid cyst rupture into the peritoneal cavity after abdominal trauma: case report and literature review. International surgery, 2012. 97(3): p. 239-244.
3. Belli, S., et al., Spontaneous giant splenic hydatid cyst rupture causing fatal anaphylactic shock: a case report and brief literature review. Turkish Journal of Gastroenterology, 2014. 25(1).
4. Akbulut, S., Parietal complication of the hydatid disease: comprehensive literature review. Medicine, 2018. 97(21).
5. Toumi, O., et al., Intraperitoneal rupture of hydatid cysts. European Journal of Trauma and Emergency Surgery, 2017. 43(3): p. 387-391.
6. Mouaqit, O., et al., Acute intraperitoneal rupture of hydatid cysts: a surgical experience with 14 cases. World Journal of Emergency Surgery, 2013. 8(1): p. 1-7.
7. Velitchkov, N., et al., Life threatening traumatic rupture of a liver hydatid cyst. European Journal of Emergency Medicine, 2001. 8(3): p. 225-228.
8. Safioleas, M., et al., Diagnostic evaluation and surgical management of hydatid disease of the liver. World journal of surgery, 1994. 18(6): p. 859-865.
9. Morris, D., Pre‐operative albendazole therapy for hydatid cyst. British journal of surgery, 1987. 74(9): p. 805-806.
10. Williams, N., et al., Love's short practice of surgery. The vermiform appendix, 2008. 1211.
11. Bailey, H., Love McN. Short Practice of Surgery 24th edition London. 2004, Hodder Arnold.
12. Zinner, M.J., S.I. Schwartz, and H. Ellis, Maingot's abdominal operations. Journal of the American College of Surgeons, 1997. 3(185): p. 307.
13. Mawhorter, S., et al., Nonsurgical therapy for pulmonary hydatid cyst disease. Chest, 1997. 112(5): p. 1432-1436.
14. Cassibba, G., et al., Spontaneous intraperitoneal rupture of a hepatic achinococcal cyst. Minerva chirurgica, 1982. 37(18): p. 1391-1397.
15. Neumayr, A., et al., Justified concern or exaggerated fear: the risk of anaphylaxis in percutaneous treatment of cystic echinococcosis—a systematic literature review. PLoS neglected tropical diseases, 2011. 5(6): p. e1154.
16. Karavias, D.D., et al., Peritoneal echinococcosis. World journal of surgery, 1996. 20(3): p. 337-340.
17. Paccione, F., Rupture of parasitic cysts and spontaneous rupture of the liver. Minerva chirurgica, 1974. 29(11): p. 685-690.
18. Paksoy, M., et al., rupture of the hydatid disease of the liver into the biliary tracts. Digestive Surgery, 1998. 15(1): p. 25-29.
19. Samama, M., et al., Low molecular weight heparin compared with unfractionated heparin in prevention of post-operative thrombosis. British journal of surgery, 1988. 75(2): p. 128-131.
20. Gunay, K., et al., Traumatic rupture of hydatid cysts: a 12-year experience from an endemic region. Journal of Trauma and Acute Care Surgery, 1999. 46(1): p. 164-167.
21. Becker, K., et al., Resolution of hydatid liver cyst by spontaneous rupture into the biliary tract. Journal of hepatology, 1997. 26(6): p. 1408-1412.
22. Ergüney, S., et al. Complicated hydatid cysts of the liver. in Annales de Chirurgie. 1991.
23. Mottaghian, H. and F. Saidi, Post-operative recurrence of hydatid disease. Journal of British Surgery, 1978. 65(4): p. 237-242.
Received: 4 March 2022 / Accepted: 31 March 2022 / Published:15 May 2022
Citation. Hammoodi Al obaidi J H. Management of Incidental Rupture of Abdominal Hydatid Cyst. Revis Bionatura 2022;7(2) 54. http://dx.doi.org/10.21931/RB/2022.07.02.54
