2022.07.04.60
Files > Volume 7 > Vol 7 No 4 2022
The association of serum visfatin in women with polycystic ovary syndrome: A case-control study
1 Department of Gynecology and Obstetrics, College of Medicine, Kufa University, Al-Najaf, Iraq; [email protected].
2 Department of Gynecology and Obstetrics, Al-Najaf Health Directorate, Ministry of Health, Al-Najaf, Iraq;
3 Department of Cardiothoracic and Vascular Surgery, Al-Sadder Teaching Medical City, Al-Najaf Health Directorate, Ministry of Health, Al-Najaf, Iraq; [email protected].
* Correspondence: [email protected]; Tel.: +964 783 249 5436
Available from: http://dx.doi.org/10.21931/RB/2022.07.04.60
ABSTRACT
Polycystic ovarian syndrome (PCOS) is the most common endocrinopathy among women of reproductive age. Visfatin is an adipokine secreted by fat tissue and macrophages involved in regulating glucose homeostasis, adipose tissue inflammation, chronic systemic inflammation, cardiovascular disease and endothelial dysfunction. The study sample (100 patients) includes 50 PCOS women and 50 control matched for age and body mass index (BMI). The women with PCOS were divided into obese or overweighed according to BMI ≥ 25 Kg/m2 and non-obese BMI ≤ 25 Kg/m2. The control group was also divided into obese and non-obese. The results showed that serum visfatin was significantly increased in obese women with POCS compared to obese control (5.61 ± 1.27 ng/mL vs. 0.48 ±0.28 ng/mL) and in non-obese women with polycystic ovarian syndrome compared to non-obese control (5.22± 1.36 ng/mL vs. 0.33± 0.26 ng/mL). These findings might suggest that visfatin could play a role in pathogenesis and the long-term consequences of PCOS.
Keywords: visfatin; polycystic ovarian syndrome; body mass index; obese women
INTRODUCTION
Polycystic ovary syndrome (PCOS) is the most common endocrine, a metabolic disorder affecting 5% to 10% of women in the reproductive age 1. It has significant and diverse clinical implications, including reproductive, infertility, hyperandrogenism, hirsutism, metabolic; insulin resistance, impaired glucose tolerance, diabetes mellitus type 2, adverse cardiovascular risk profiles and psychological features; increased anxiety, depression and worsened quality of life 2. Its management should focus on support, education, addressing psychological factors and strongly emphasizing healthy lifestyle with targeted medical therapy, monitoring and control of long-term metabolic complications 3.
The adipose tissue (AT) secretes many bioactive factors, called adipokines, that act locally within the fatty tissue and affects distant organs. These are tumor necrosis factor (TNF-𝛼), interleukins (IL), angiotensinogen, plasminogen activator inhibitor-1 (PAI-1), leptin, visfatin, resistin, and apelin 4,5.
Visfatin is highly in various tissues and cell types, including adipocytes, lymphocytes, bone marrow, liver, muscle, trophoblast, and fetal membranes 6. Although there are conflicting data on the relationship between visfatin and obesity, a recent meta-analysis revealed that plasma visfatin is significantly increased in subjects diagnosed with overweight/obesity, DM type 2, metabolic syndrome, and cardiovascular diseases (CVD) 7. Many studies demonstrated that visfatin displayed proinflammatory properties and modulated immune functions; as a result, rising visfatin levels correlate with the degree of endothelial dysfunction, and it is expressed higher in the atherosclerotic lesions of symptomatic patients than in the lesions of asymptomatic patients, further emphasizing the role of this adipokine in plaque destabilization and acute cardiovascular events 8,9. Likewise, elevated visfatin levels in PCOS may also signal heightened cardiovascular risk in particular women with this syndrome, particularly in those with insulin resistance 10.
This study aims to determine the serum levels of visfatin in women with PCOS and compare them with healthy control.
MATERIALS AND METHODS
This case-control study was done at Fertility Center, Al-Sadder Medical City and Al-Zahra'a Teaching Hospital for maternity and pediatrics, Najaf, Iraq, from March 1, 2019, to December 1, 2019. In this study, one hundred women were included, sub-divided into 50 patients with PCOS and 50 cases as control (were healthy matched for ages and BMI with the regular menstrual cycle). The women with PCOS were further divided into obese BMI≥ 25 Kg/m2 and non-obese BMI ≤25 Kg/m2. The control group was divided into obese and non-obese. The diagnosis of PCOS depends on the European Society of Human Reproduction and Embryology and the American Society for Reproductive Medicine (ESHRE / ASRM) in Rotterdam, Netherlands, in Oct 2003 11.
Inclusion criteria ( two of three)
1) Oligo ovulation and anovulation.
2) Clinical manifestations of androgen excess and/or hyperandrogenism.
3) Polycystic ovaries changes: ≥ 12 follicles (2-9 mm in diameter) in one side or both sides of the ovaries and/or ovarian volume ≥ 10 mL.
Exclusion criteria
1) Diabetes, cardiovascular disease, hypertension, infections, hypothyroidism, hyperprolactinemia, or other serious medical problems.
2) Patients use anti-inflammatory drugs (within the previous three months), or drugs are known to affect carbohydrate and lipid metabolism, oral contraceptives, glucocorticoids, ovulation induction agents, antidiabetic and antiobesity drugs, estrogenic, or antiandrogenic or antihypertensive medication.
3) Other causes of hyperandrogenism like Cushing's syndrome, congenital adrenal hyperplasia adrenal and pituitary tumors.
After explaining the whole procedure, patients information were documented in detail, including age and BMI. A physical examination and baseline assessment were done for the patients on day 2 or 3 of the menstrual cycle. BMI was calculated as body weight in kilograms divided by height in squared meters (Kg/m2). A transvaginal ultrasound scan was performed for all participants by real-time ultrasound device using a vaginal probe 7.5 MHZ. The morphology of polycystic ovaries was considered if there were 12 or more follicles of 2-9 mm in diameter in each ovary and/or an enlarged ovary (ovarian volume >10 cm3) 12. The scan is also used to measure the endometrial thickness and check the surrounding structures. Blood samples were taken through a standard venipuncture of the antecubital vein to withdraw about 5ml at the first 2-3 days of the menstrual cycle and centrifuged to collect serum. Part of the serum was used to measure hormones, including estradiol, FSH, LH and prolactin. Serum visfatin was determined by ELISA quantitative in vitro diagnostic measurement. The kit name was (cloud-clone corporation 1304 Langham Greek organization suit 226 Houston Tx 77084, USA ).
Statistical analysis was performed using SPSS 20.0 statistical software. Measurement data were expressed as mean ± standard deviation, and one-way ANOVA (analysis of variance) was used to compare different measurements (numerical data). The p-value <0.05 is statistically significant.
RESULTS
In this study, the mean age for PCOS women was 26 years, and for control, women were 28 years. BMI for PCOS women was 25.7 Kg/m2, and for management, women were 26.1 Kg/m2. Regarding hormonal assay for PCOS women and control women, respectively, were shown in table 1.
Regarding visfatin level in PCOS women was 5.41 ng/mL, while in control women was 0.40 ng/mL. In Obese, PCOS was 5.61 ng/mL, while in non-obese, PCOS was 5.22 ng/mL, as shown in Table 2.
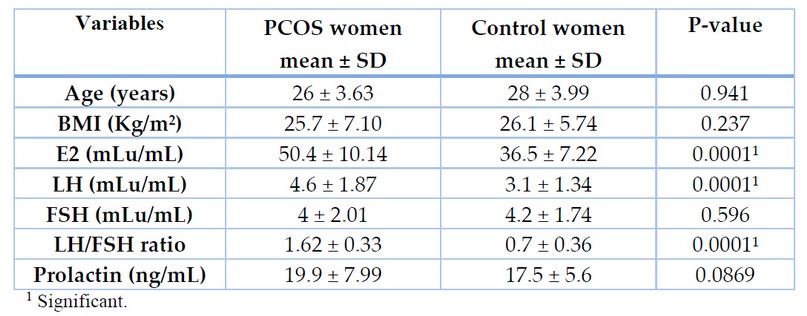
Table 1. Hormonal, BMI and age differences between PCOS women and control women.
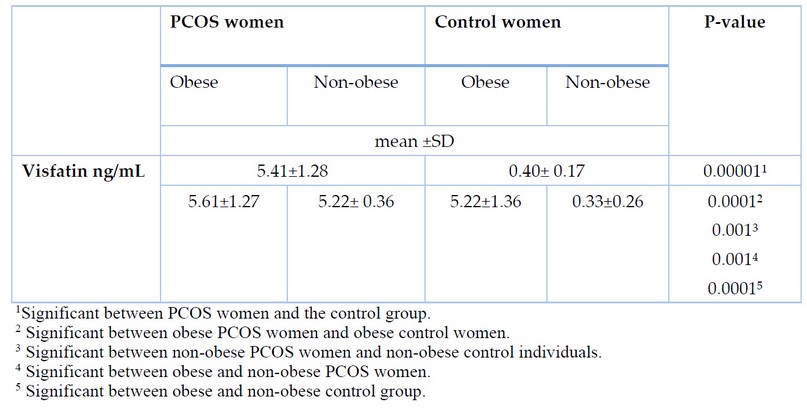
Table 2. Visfatin level in Obese PCOS, non- obese PCOS women and control women.
DISCUSSION
Visfatin is considered to have many actions, such as insulin-like activity under physiological conditions, lowering blood glucose levels, an ability to stimulate proinflammatory activity by enhancing TNF-α and IL-6 secretion, a direct contributor to vascular inflammation and endothelial dysfunction that are considered key features of atherosclerosis diseases linked to metabolic syndrome 13,14,15.
The present study showed that serum visfatin levels were significantly higher in the PCOS group than in the control group (P=0.0001). There was a significant difference between obese PCOS women and non-obese PCOS (P=0.001) concerning their visfatin levels. It was significantly increased in obese women with PCOS compared to obese control (P=0.0001) and in non-obese women with PCOS compared to non-obese control (P=0.0001).
Dıkmen et al. found that serum visfatin levels were similar in normal-weight PCOS and control group, and the level of visfatin observed in obese and overweight patients with PCOS was higher than that found in control women with equal BMI; in addition, obese women with PCOS also had significantly higher levels than normal weight women with PCOS 16.
El-said et al. found that visfatin levels are increased in women with PCOS compared to healthy controls. There was a positive correlation between visfatin and free androgen index in PCOS patients 17. While Kandasamy et al., and Jongwutiwes et al., found that visfatin level of visfatin was significantly increased in women with PCOS than in healthy control subjects, and also it was positively correlated with insulin resistance and BMI, so the result indicates that South Indian women with PCOS exhibit higher levels and elevated insulin resistance, which suggest that visfatin could be a potential biomarker for PCOS 18,19.
On the other hand, Kowalska et al. found that the PCOS group had lower insulin sensitivity and higher serum visfatin than the control group, and a decrease in insulin sensitivity was present in both the lean and obese PCOS subjects. In contrast, the increase in visfatin level was observed only in lean PCOS subjects. In addition, serum visfatin was negatively correlated with insulin sensitivity. This may indicate that it is associated with insulin resistance and markers of hyperandrogenism in lean PCOS patients 20.
Another study done by Al Dallow Yamam et al. reported that plasma visfatin levels were significantly increased in normal weight and obese women with PCOS compared to control. It had a positive linear correlation with BMI, fasting insulin and HOMA-IR. These findings suggest that it may be related to obesity and insulin resistance 21.
Güdücü et al. reported that visfatin levels were higher in normal-weight PCOS compared to obese PCOS, but it did not reach statistical significance. It correlated negatively with fasting blood glucose, total cholesterol (TC), low-density lipoprotein (LDL) and lipoprotein-a levels in PCOS patients. It had no correlation with homeostasis model assessment-insulin resistance and fasting insulin levels, but the negative correlation between plasma visfatin levels and lipoprotein-a, fasting plasma glucose, TC and LDL levels may indicate a role for it in cardiovascular disease independent of insulin resistance 22. Authors should discuss the results and how they can be interpreted from the perspective of previous studies and of the working hypotheses. The findings and their implications should be discussed in the broadest context possible. Future research directions may also be highlighted.
CONCLUSIONS
This study concludes that plasma visfatin level was increased in polycystic ovary syndrome women and in obese women more than non-obese. These findings might suggest that visfatin could play a role in pathogenesis and the long-term consequences of PCOS.
Author Contributions: “Conceptualization, B.S.A., A.A.M. and A.M.F.; methodology, B.S.A., and A.A.M.; software, B.S.A.; validation, B.S.A., A.A.M. and A.M.F.; formal analysis, A.A.M. and A.M.F.; investigation, A.A.M. and A.M.F.; resources, A.A.M. and A.M.F.; data curation, A.A.M. and A.M.F.; writing—original draft preparation, A.A.M. and A.M.F.; writing—review and editing, A.A.M. and A.M.F.; visualization, A.A.M. and A.M.F.; supervision, B.S.A.; project administration, B.S.A.; funding acquisition, B.S.A.. All authors have read and agreed to the published version of the manuscript."
Funding: "This research received no external funding".
Institutional Review Board Statement: "The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of College of Medicine, Kufa University (protocol code 2021.2298734 and 04/02/2019)."
Informed Consent Statement: "Informed consent was obtained from all subjects involved in the study."
"Written informed consent has been obtained from the patient(s) to publish this paper".
Conflicts of Interest: "The authors declare no conflict of interest."
REFERENCES
1. Sirmans, S. M., Pate, K. A. Epidemiology, diagnosis, and management of polycystic ovary syndrome. Clinical epidemiology, 2013, 6, 1–13. https://doi.org/10.2147/CLEP.S37559.
2. Diamanti-Kandarakis E. Insulin resistance in PCOS. Endocrine, 2006, 30(1), 13–17. https://doi.org/10.1385/ENDO:30:1:13.
3. Bargiota, A., & Diamanti-Kandarakis, E. The effects of old, new and emerging medicines on metabolic aberrations in PCOS. Therapeutic advances in endocrinology and metabolism, 2012, 3(1), 27–47. https://doi.org/10.1177/2042018812437355.
4. Fortuño, A., Rodríguez, A., Gómez-Ambrosi, J., Frühbeck, G., & Díez, J. Adipose tissue as an endocrine organ: role of leptin and adiponectin in the pathogenesis of cardiovascular diseases. Journal of physiology and biochemistry, 2003, 59(1), 51–60. https://doi.org/10.1007/BF03179868.
5. Fukuhara, A., Matsuda, M., Nishizawa, M., Segawa, K., Tanaka, M., Kishimoto, K., Matsuki, Y., Murakami, M., Ichisaka, T., Murakami, H., Watanabe, E., Takagi, T., Akiyoshi, M., Ohtsubo, T., Kihara, S., Yamashita, S., Makishima, M., Funahashi, T., Yamanaka, S., Hiramatsu, R., … Shimomura, I. Visfatin: a protein secreted by visceral fat that mimics the effects of insulin. Science (New York, N.Y.), 2005, 307(5708), 426–430. https://doi.org/10.1126/science.1097243.
6. Astern, J. M., Collier, A. C., & Kendal-Wright, C. E. Pre-B cell colony enhancing factor (PBEF/NAMPT/Visfatin) and vascular endothelial growth factor (VEGF) cooperate to increase the permeability of the human placental amnion. Placenta, 2013, 34(1), 42–49. https://doi.org/10.1016/j.placenta.2012.10.008.
7. Moschen, A. R., Kaser, A., Enrich, B., Mosheimer, B., Theurl, M., Niederegger, H., & Tilg, H. Visfatin, an adipocytokine with proinflammatory and immunomodulating properties. Journal of immunology (Baltimore, Md. : 1950), 2007, 178(3), 1748–1758. https://doi.org/10.4049/jimmunol.178.3.1748.
8. Adya, R., Tan, B. K., Chen, J., & Randeva, H. S. Nuclear factor-kappaB induction by visfatin in human vascular endothelial cells: its role in MMP-2/9 production and activation. Diabetes care, 2008, 31(4), 758–760. https://doi.org/10.2337/dc07-1544Title of Site. Available online: URL (accessed on Day Month Year).
9. Auguet, T., Aragonès, G., Guiu-Jurado, E., Berlanga, A., Curriu, M., Martinez, S., Alibalic, A., Aguilar, C., Camara, M. L., Hernández, E., Ruyra, X., Martín-Paredero, V., & Richart, C. Adipo/cytokines in atherosclerotic secretomes: increased visfatin levels in unstable carotid plaque. BMC cardiovascular disorders, 2016, 16(1), 149. https://doi.org/10.1186/s12872-016-0320-5
10. Roberts, C. K., Hevener, A. L., & Barnard, R. J. Metabolic syndrome and insulin resistance: underlying causes and modification by exercise training. Comprehensive Physiology, 2013, 3(1), 1–58. https://doi.org/10.1002/cphy.c110062
11. Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertility and sterility, 2004, 81(1), 19–25. https://doi.org/10.1016/j.fertnstert.2003.10.004
12. Bachanek, M., Abdalla, N., Cendrowski, K., & Sawicki, W. Value of ultrasonography in the diagnosis of polycystic ovary syndrome - literature review. Journal of ultrasonography, 2015, 15(63), 410–422. https://doi.org/10.15557/JoU.2015.0038
13. Jung, U. J., & Choi, M. S. Obesity and its metabolic complications: the role of adipokines and the relationship between obesity, inflammation, insulin resistance, dyslipidemia and nonalcoholic fatty liver disease. International journal of molecular sciences, 2014, 15(4), 6184–6223. https://doi.org/10.3390/ijms15046184
14. Sun, Y., Wu, Z., Wei, L., Liu, C., Zhu, S., & Tang, S. High-visfatin levels in women with polycystic ovary syndrome: evidence from a meta-analysis. Gynecological endocrinology: the official journal of the International Society of Gynecological Endocrinology, 2015, 31(10), 808–814. https://doi.org/10.3109/09513590.2015.1056140
15. Berezin, A. Does Visfatin Predict Cardiovascular Complications in Metabolic Syndrome Patients? Endocrinol Metab Syndrome.2016, 5(1); 1-5.
16. Dıkmen, E., Tarkun, I., Cantürk, Z., & Cetınarslan, B. Plasma visfatin level in women with polycystic ovary syndrome. Gynecological endocrinology : the official journal of the International Society of Gynecological Endocrinology, 2011, 27(7), 475–479. https://doi.org/10.3109/09513590.2010.495796
17. El-said, M. H., El-said, N. H., Abd El-ghaffar, M. N. Plasma Visfatin Concentrations in Polycystic Ovary Syndrome: Relationships with Indices of Insulin Resistance and Hyperandrogenism. Med. J. Cairo Univ., 2009, 77(3): 1-7.
18. Kandasamy S, Inmozhisivagamasundari. R, Bupathy. A study of serum visfatin in South Indian women with polycystic ovary syndrome. International Journal of Current Research in Medical Sciences. 2016, 2(9):1-7.
19. Jongwutiwes, T., Lertvikool, S., Leelaphiwat, S., Rattanasiri, S., Jultanmas, R., & Weerakiet, S. Serum visfatin in Asian women with polycystic ovary syndrome. Gynecological endocrinology: the official journal of the International Society of Gynecological Endocrinology, 2009, 25(8), 536–542. https://doi.org/10.1080/09513590903015478
20. Kowalska, I., Straczkowski, M., Nikolajuk, A., Adamska, A., Karczewska-Kupczewska, M., Otziomek, E., Wolczynski, S., & Gorska, M. Serum visfatin in relation to insulin resistance and markers of hyperandrogenism in lean and obese women with polycystic ovary syndrome. Human reproduction (Oxford, England), 2007, 22(7), 1824–1829. https://doi.org/10.1093/humrep/dem118
21. Yamam, A., Kaleel, A., Shaden, H. Plasma Visfatin Level in Women with Polycystic Ovary Syndrome.Int. J. Pharm. Sci. Rev. Res., 2013, 22(7):38-40.
22. Güdücü, N., İşçi, H., Görmüş, U., Yiğiter, A. B., & Dünder, I. Serum visfatin levels in women with polycystic ovary syndrome. Gynecological endocrinology: the official journal of the International Society of Gynecological Endocrinology, 2012, 28(8), 619–623. https://doi.org/10.3109/09513590.2011.650749
Received: April 22, 2022 / Accepted: June 18, 2022 / Published:15 November 2022
Citation: Al- Ghazali B S, Mohammed A A, Fahad A M. The association of serum visfatin in women with polycystic ovary syndrome: A case-control study. Revis Bionatura 2022;7(4) 60. http://dx.doi.org/10.21931/RB/2022.07.04.60
