CS 2019.02.01.11
Files > Conference Series > 2019 > Humboldt Kolleg 2019
Bionatura Conference Series Vol 2. No 1. 2019
“Breaking Paradigms: Towards a Multi-, Inter- and Transdisciplinary Science” In commemoration of the 250th Anniversary of Alexander von Humboldt
Effect of six bis-THTT derivatives in the control of parasitaemia in two rodent malaria species
Katherine S. Loachamin1, Hortensia M. Rodríguez2 and Lilian M. Spencer1*
Disponible en: http://dx.doi.org/10.21931/RB/CS/2019.02.01.11
ABSTRACT
Malaria is a life-threatening disease caused by parasites of the genus Plasmodium and is transmitted to humans by the bite of female mosquitoes of the genus Anopheles. WHO has reported 219 million cases of malaria and 435,000 deaths were estimated in 2017. The anti-malarial treatment more frequently used is based on Chloroquine, which has been used for several decades. This prolonged application has caused the parasite to develop resistance to the use of the mentioned drug, so it becomes necessary to search for new treatments. In addition, some tetrahydro-(2H)-1,3,5-thiadiazine-2-thione (THTT) derivatives have been previously studied as possible trypanosomicides, obtaining satisfactory results in the treatment to Trypanosoma cruzi; Trichomonas vaginalis and T. b. rhodesiense, although no studies against malaria have been reported. In the present work, six bis-THTT derivatives were evaluated as potential anti-malarial drugs (JH1, JH2, JH3, JH4, JH5, and JH6) with BALB/c mice, which were inoculated with Plasmodium berghei ANKA strain and Plasmodium yoelii 17XL strain. The percentages of parasitemia were determined for each tested compound, which was assessed daily on smears from tail blood, stained with Giemsa’s reagent and observed under light microscopy as evidence of cure. Our results showed that JH2 and JH4 presented effective parasitemia control similar to chloroquine in P. berghei. Besides, JH5 and JH6 exhibited better results than Chloroquine with P. yoelii infection. In summary, four of the six bis-THTT derivatives tested, could be considerate as potential new drugs to infection malaria rodent control. Immune response essays should be realized in order to confirm our preliminary results.
Keywords: Plasmodium berghei, Plasmodium yoelii, bis-thiadiazine, and parasitemia.
INTRODUCTION
Malaria is caused by protozoan parasites belonging to the genus Plasmodium and it has several characteristic symptoms, such as a very fast fever between 8-9 hours. Malaria has a mortality rate of 1-2 million people in tropical and sub-tropical regions, with 90% of this amount corresponding to children living in sub-African countries 1. There are several species of human malaria, such as P. vivax, P. ovale, P. malariae, P. knowlesi and P. falciparum, the latter is the most fatal in human malaria.
Currently, there are several difficulties with anti-malarial treatments because of drug resistance in endemic areas of high transmission. In this sense, the development of new effective drugs has been discouraging due to the low efficiency of them, and in consequence, the need for low-cost drugs without toxicity problems has grown to avoid resistance to anti-malarial drugs 2,3 .
In previous study the tetrahydro-(2H)-1,3,5-thiadiazine-2-thione (THTT) derivatives were studied as possible trypanosomicides, obtaining satisfactory results in the treatment to Trypanosoma cruzi; Trichomonas vaginalis and T. b. rhodesiense 4. In the present work, we evaluated the anti-malarial activity of six Bis-THTT derivatives in BALB/c strain mice inoculated with two Plasmodium strains rodent parasites (P. yoelii and P. berghei). Because, P. berghei is analogous to P. falciparum that generate malaria in human, they have a life cycle, structure, physiology, and pathology very similar5. In the same way, P. yoelii 17XL is analogous to P. vivax 6.
The effect of the cure was evaluated by observation microscopy optical from smears from each experimental group of mice treated with Bis-THTT derivative compounds and chloroquine (CQ) as cure control.
MATERIAL AND METHODS
Strains of Plasmodium berghei ANKA and Plasmodium yoelii 17XL were used in vivo the experiments to evaluated six THTT compounds. The parasites were kept cryopreserved (20% glycerol at -80 ° C) and passed through an intraperitoneal (IP) inoculation of 200 ml in adult female BALB/c mice (two mice per strain), approximately by 10 weeks. The parasitaemia was monitored daily until reaching a value equal to or higher than 40% of parasitaemia, by means of smears fixed with absolute methanol and stained with Giemsa´s, through optical microscopy immersed.
Mice with parasitemia greater than 40% were sacrificed and their blood was collected using heparinized Krebs solution (0.9% NaCl + 4.2% sorbitol in a 1:20 dilution of Heparin). The blood obtained was purified through a column of Cellulose (CF-11 (Sigma), Buffer NaCl 0. 9%), thus retaining the white blood cells and eluting the parasitized red blood cells (PRBCs). The PRBC sample was centrifuged at 2,000 rpm for five minutes at 4 °C, and then the pellet was resuspended in Krebs solution. Subsequently, the concentration of PRBC was determined in the Neubauer chamber.
The inoculum with P. berghei and P. yoelii (5000 PRBCs, parasite red blood cells in 200 µl) was administered intraperitoneally to 48 female BALB/c mice, (24 mice inoculated with P. berghei and 24 mice inoculated with P. yoelii) 7.
Six bis-THTT derivatives was called JH1, JH2, JH3, JH4, JH5, and JH6 were evaluated as possible anti-malarial compounds. CQ was used as cure control of malaria infection. The bis-THTT derivative compounds were used at a concentration of 20 mg/kg. To dissolve the compounds we used Dimethyl Sulfoxide (DMSO) at 1 %, and cellulose at 1% and Tween 80 at 0.5% were used as vehicle solution of compounds. The treatments were administered orally by 4 days consecutive (3 days after infection with parasites). In order to determinate the cure effect the parasitaemia was monitored daily by smears, fixed with absolute methanol and stained with Giemsa´s 8.
RESULTS AND DISCUSSION
Six compounds (JH1, JH2, JH3, JH4, JH5 and JH6) were evaluated as anti-malarial drugs and compared to CQ to control of malaria parasites infection. The parasitemia was monitored daily after the first administration of the Bis- THTTs derivative compounds and CQ was used as a positive control of cure. In Figure 1 shows the parasitaemia percentages after the challenge with P. berghei (Figure 1A and 1B). JH2 and JH4 showed a control infection better than the other tested compounds; although these do not exceed 17% of parasitemia up to 14 days after treatment. However, JH2 and JH4 compounds were not more effective than CQ in the control of the percentage of parasitemia. In order to the mice infected with P. yoelii, the percentage of parasitemia (Figure 1C and 1D) were not higher of 10 % for JH5 and JH6 derivative compounds. Our preliminary studies showed that CQ continues to be the best drug for malaria infection control, in this case, rodent malaria. But JH2 and JH4 presented a similar percentage of parasitemia on day 14 with P. berghei infection. The infection control without any treatment was longer to P. berhei than P. yoelii, and a possible explanation is that P. berghei strain is less virulent, because this strain was passed more time that the P. yoelii through the vertebrate host 9.
On the other hand, to P. yoelii infection, the JH5 and JH6 between 12 to 14 days were very similar the control of infection that CQ. This suggests that JH5 and JH6 could be a good alternative in areas resistant to chloroquine treatment.
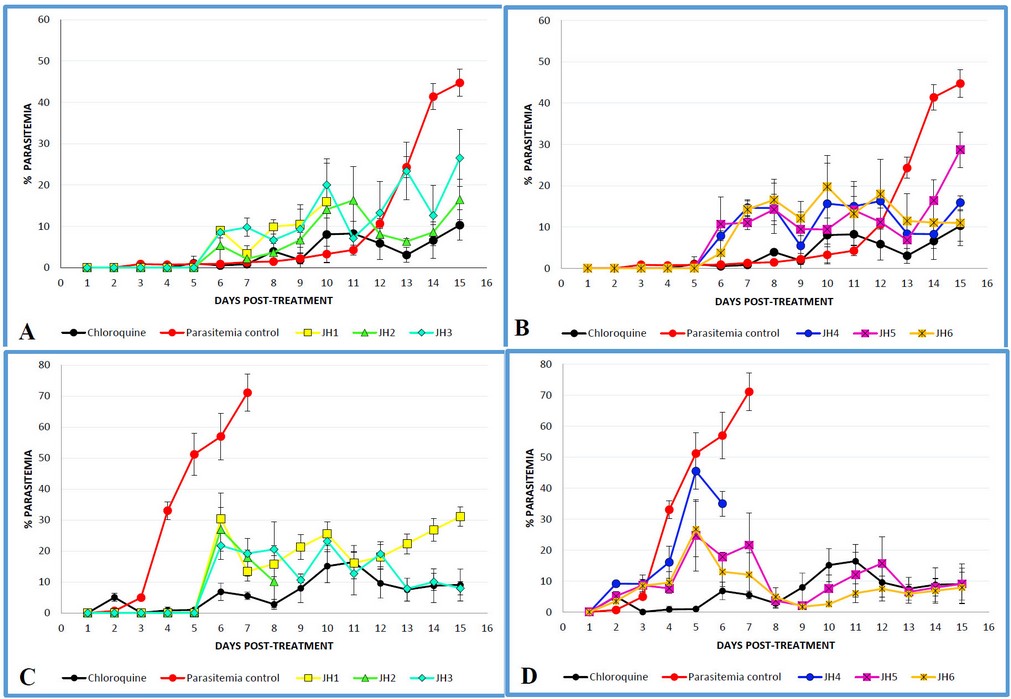
Fig. 1. Parasitemia-Time profile using BALB/c mice following the administration of 4 dose regimen of 20 mg/kg, Chloroquine (n=3), JH1 (n=3), JH2 (n=3), JH3 (n=3), JH4 (n=3), JH5 (n=3) and JH6 (n=3), administered 72 hours after IP inoculation with 105 P. berghei (Panels A and B) parasitized-erythrocytes and P.yoelii (Panels C and D). Data are shown as total parasitemia (mean percentage of infected erythrocytes/ total erythrocytes ± SD), starting from the time of drug administration. Parasitemia was monitored daily by smears fixed with absolute methanol and Giemsa´s stained.
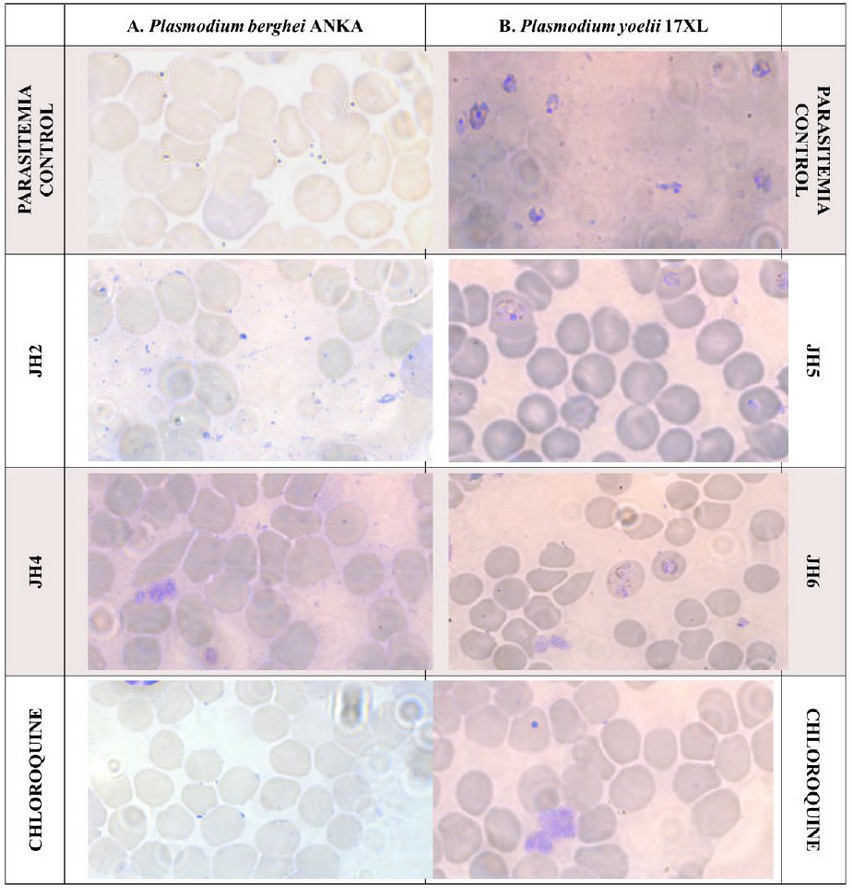
Figure 2. Blood smear of BALB/c mice infected with P. berghei (Panel A) and P. yoelii (Panel B), treated with the JH2, JH4, JH5 y JH6 compounds respectively and Chloroquine as cure control. The orange circles show red blood cells with parasites in merozoite stage and the red circles point out red blood cells with parasites in the mature schizonte stage.
Figure 2 shows different pictures from infected blood smears with the Plasmodium parasite 10. Figure 2A corresponds to P. berghei, and the orange circles point out the parasite in merozoite stage (A.1, A.2, A.3 and A.4). Figure 2B shows the blood smear with P. yoelii infection, and the red circles indicate the red blood cells with parasites in mature schizonte stage. In consequence, the P. yoelii infection was not very well controlled with JH5 and JH6 compounds, because the parasites can develop mature schizont stage. In addition, the P. yoelii strain is more virulent that P. berghei as we mention above. In both strain CQ presented less infection and this demonstrated that it the best treatment to malaria infection.
CONCLUSION
Our results suggest that the six bis-THTT tested have different behavior depending on the strain of Plasmodium to which the treatment was applied. In this case, the treatment was more effective in mice infected with P. yoelii, equivalent to Plasmodium vivax species in Humans. As shown in Figure 1, JH2 and JH4 had anti-malarial effect for P. berghei, and compounds JH5 and JH6 also had anti-malarial effect for P. yoelii infections. These compounds controlled the infections, presenting 17% parasitaemia by day 14. Nevertheless, they did not exceed the Chloroquine efficiency, which showed 10% parasitaemia at day 14 post-treatment.
However, cytotoxic evaluation of tested compounds in the VERO cell line with a MTS colorimetric test of the company Promega and its evaluation of the humoral response in indirect ELISA assays with the hyperimmune sera of mice immunized with each of these compounds must be done in order to corroborate the reported results.
REFERENCES
1. World Health Organizacion. (2018). Overview of malaria treatment. Retrieved from: https://www.who.int/malaria/areas/treatment/overview/en/
- Chinappi, M., Via, A., Marcatili, P., & Tramontano, A. (2010). On the Mechanism of Chloroquine Resistance in Plasmodium falciparum. PLoS ONE, 5(11), e14064.doi:10.1371/journal.pone.0014064.
3. Moore, B.; Page-Sharp, M.; Stoney, J.;. Ilett, K.; Jago, J.; and K. Batty. (2011) Pharmacokinetics, Pharmacodynamics, and Allometric Scaling of Chloroquine in a Murine Malaria Model. Antimicrobial agents and chemotherapy. 55(8): 3899–3907.
4. Coro, J., Atherton, R., Little, S., Wharton, H., Yardley, V., Alvarez, A., Rodríguez, H. (2006). Alkyl-linked bis-THTT derivatives as potent in vitro trypanocidal agents. Bioorganic & Medicinal Chemistry Letters, 16(5), 1312–1315.doi:10.1016/j.bmcl.2005.11.060
5. Craig, A.G.; Grau, G.E.; Janse C.; Kazura J.W.; Milner D.; Barnwell J.W.; Turner G.; and Langhorne J. (2012). The role of animal models for research on severe malaria. PLoS Pathog Feb;8(2):e1002401. doi: 10.1371/journal.ppat.1002401.
6. Yoeli, M., Hargreaves, B., Carter, R., &Walliker, D. (1975). Sudden increase in virulence in a strain of Plasmodium bergheiyoelii. Annals of Tropical Medicine & Parasitology, 69(2), 173–178. doi:10.1080/00034983.1975.11686998.
7. Spencer L., Quintana D. and Hidalgo L. (2008). An assay to evaluate the inhibition of invasion in vitro of P. yoelii strain with different monoclonal antibodies raised against MSP-119. Rev. Biomed. 19:45-51.
8. Spencer L. M.; Peña-Quintero, A.; Canuda N., Inojosa I. and Urdaneta N. (2018). Study of antimalarial effect of two photo-excitable compounds in a murine model with Plasmodium berghei. Revista Biología Tropical. 66(2):880-891
9. Andrade, B.B., Teixeira, C.R., Barral, A., &Barral-Netto, M. (2005). Haematophagous arthropod saliva and host defense system: a tale of tear and blood. Anais da Academia Brasileira de Ciencias, 77 4, 665-93. http://dx.doi.org/10.1590/S0001-37652005000400008.
10. Cowman, A. and B. Crabb. (2006) Invasion of Red Blood Cells by Malaria Parasites. Cell. 124:755–766.
Received: 24 April 2019
Accepted: 21 May 2019
Katherine S. Loachamin1, Hortensia M. Rodríguez2 and Lilian M. Spencer1*
1 School of Biological Sciences and Engineering, Yachay Tech University.
2 School of Chemical Sciences and Engineering Yachay Tech University.
*Correspondent author: [email protected]
