CS 2019.02.01.18
Files > Conference Series > 2019 > Humboldt Kolleg 2019
Bionatura Conference Series Vol 2. No 1. 2019
“Breaking Paradigms: Towards a Multi-, Inter- and Transdisciplinary Science” In commemoration of the 250th Anniversary of Alexander von Humboldt
Therapeutic angiogenesis as a treatment for Coronary Artery Occlusions
Sebastian Alcivar, Jonathan Hermenejildo
available in: http://dx.doi.org/10.21931/RB/CS/2019.02.01.18
ABSTRACT
Cardiovascular diseases are one of the leading causes of death in the world. The inflammation or accumulation of a substance in arteries generates the formation of atherosclerosis, stenosis, coronary artery disease, coronary thrombosis, and occlusion. The present study offers some solutions under investigation for the mentioned pathologies. Traditionally this condition is treated mainly by a percutaneous coronary intervention, bypass, or by specific medications.
In the present review, based on original articles, the more suitable treatments were chosen. These angiogenic treatments show the best assessments on coronary artery occlusions. All these treatments focus on the generation of new blood vessels from the already existing vasculature.
Keywords: occlusion, angiogenesis, angiogenic factors, collateral formation.
INTRODUCTION
Despite advances in medicine, mortality from cardiovascular diseases is one of the leading causes. For example, according to the statistical analysis of the European society of cardiology, deaths due to coronary heart disease is amount to 1.8 million in Europe alone1. The disease develops when the narrowing of the coronary artery reduces the flow of essential nutrients to the heart due to the deposit of cholesterol, calcium, inflammatory cells, and other substances2. The total or partial occlusion of the coronary artery is commonly known as atherosclerosis, stenosis, coronary arteriopathy, coronary artery disease, and coronary thrombosis. While, for the diagnosis of this pathology, it is done through the use of angiograms with the evaluation of the frames generated by it. In addition, there are other forms of exploration, such as electrocardiograms that can evaluate a previous or current heart attack; by computerized tomography in which the deposits of substances in the arteries like calcium are observed; by echocardiograms in which the waves generated by the physical effort of the patient will be evaluated; also, intravascular ultrasound, radiography and nuclear exploration of heart3.
Percutaneous coronary intervention (PCI) is one of the main procedures traditionally used to improve and restore blood flow. This procedure uses a catheter for the placement of a stent to allow passage of flow through the arteries affected by the occlusion of any of the substances mentioned above4. Another of the interventions to treat this pathology is the bypass that, like the stent, helps improve blood flow. However, this treatment is carried out employing a surgical surgery, which consists of creating a new route or derivation around the obstruction of the artery. The material used for the new route is a piece of a blood vessel from the leg, chest, or another part of the body to graft it into the coronary artery of interest5,6. Apart from this, it is possible to treat coronary occlusion with drugs such as cholesterol modifying, aspirin, Beta-blockers, calcium channel blockers, ranolazine, nitroglycerine, angiotensin-converting enzyme inhibitors, and angiotensin II receptor blockers7.
Therapeutic angiogenesis is a procedure made to treat ischemic diseases by generating new blood vessels from already existing vasculature8. Its primary focus is to induce, develop, and control the angiogenic responses of the subject, to revascularize ischemic tissues9. This therapeutic angiogenesis is based on the delivery of exogenous factors, which are the ones that will stimulate the formation of new vasculature, these factors can be either genes, proteins or cells, due to the best efficacy showed in animal studies8. Growth factors, such as the vascular endothelial growth factor (VEGF) and fibroblast growth factor (FGF) can be delivered as proteins or genes encoding target proteins. The underlying hypothesis of therapeutic angiogenesis is to apply angiogenic factors in ischemic tissues to guide angiogenic cellular and tissue behavior9.
Figure 1. Artery disease coronary illness as a medical concept with gradual plaque formation resulting in clogged arteries and atherosclerosis with a human anatomy diagram with 3D elements. ID 124718479 © Skypixel | Dreamstime.com
Treatments
Erythropoietin and VEGF
Erythropoietin (EPO) is a glycoprotein cytosine that regulates the proliferation and differentiation of erythrocyte progenitor cells10. Westenbrink et al. demonstrated that EPO induces neovascularization in ischemic hearts. In addition to improving micro vascularization and cardiac function in patients with ischemia11. EPO stimulates vessel growth known as angiogenesis through the use of bone marrow cells and increased myocardial expression of VEGF12.
According to the study of Jaquet et al. several angiogenic factors were used, mainly EPO which gave favorable results with a maximum effect on the endothelial cells developed from myocardial tissue. While with the continuous supply of recombinant human erythropoietin (rHuEpo) it resulted in a 220% increase in the length of the endothelium. Besides, they obtained that EPO and VEGF165 demonstrate an equal angiogenic potential. Additional experiments revealed that when they were applied at the same time as growth factors, they do not generate a further increase in proliferative capacity. The combination of VEGF and bFGF resulted in a slight increase in the length of the endothelium growths compared to VEGF. Additionally, it was observed that by combining VEGF and aFGF, they mutually inhibit each other13.
In conclusion, EPO has angiogenic potential in human myocardial tissue. Angiogenesis and among others are essential functions of the EPO14, which makes it a substance considered for the treatment of coronary heart diseases.
Autologous vascular smooth muscle cell-based myocardial gene therapy
The use of gene therapy has a high success rate in stimulating angiogenesis. Various cytokines have been found to be mediating agents for collateral growth and angiogenesis, between these agents we have VEGF, platelet-derived growth factor (PDGF), and basic fibroblast growth factor (bFGF)15,16. Nevertheless, there are still problems related to this kind of therapy, for example, a poor transfection efficiency, nonspecific effects of the transfection, and the organ-specific transfection. Moreover, as the technique has been based on direct injection of the vector (plasmid or viral) in the myocardium, more issues come with it, such as the non-uniformity of the transfection and the possibility that a substantial fraction of the vectors can reach the blood circulation, thus transfection other organs.
A proposal to go past these problems is to use autologous cells, more specific vascular smooth muscle cells (VSMC) that can transfect the genes in the myocardium in a uniform way via intracoronary administration. The main reasons to work with this type of cells is because of their ease to obtain, their division is quickly, and their limited plasticity will not let them differentiate or dedifferentiate16,17. VSMC are administered via intracoronary injection to avoid a non-organ-specific transfection, as the cells due to its larger size are going to stay at the precapillary portions.
In the most relevant study found, they use autologous VSMC transfected with the VEGF gene and the enhanced green fluorescent protein (EGFP) gene, delivered via an intracoronary pathway to accelerate collateral development. The model of the study were dogs with induced repetitive ischemia over 21 days. The study had three groups, the animals which were injected with the VSMCs transfected with the VEGF gene and the EGFP gene, the control group which only had the enhanced green fluorescent protein-transfected cells, and the sham group (no cell transplantation). The collateral flow showed an increase in the VEGF group; however, it never reached the natural collateral flow levels, and the suspicions were a diminish of the VEGF expression in the transfected group or that VEGF needs to work with other factors. Implying that VEGF is essential and useful for the initiation of collateral development, but it needs other growth factors to complete the process. Another consideration found to be needed for a better action of VEGF is existing ischemia16.
Basic fibroblast growth factor
FGF is a powerful and widely used angiogenic factor; this family of growth factors is conformed by nine factors named basic FGF (bFGF), acidic FGF, FGF 3-98,18. b(FGF) and acidic (FGF) are the most characterized of this family of FGF18. b(FGF) is one of the first discovered angiogenic factors that have angiogenic and arteriogenic properties9. This member of the FGF family is a monomeric polypeptide which induces angiogenesis in vivo studies, induces the proliferation of endothelial cells and smooth muscle cells due to the expression of FGF receptors, and also it is involved in the regulation of homeostasis and proliferation of blood vessels9,19. Nevertheless, as many of the other growth factors, preclinical data have established that eventually the delivery of bFGF results in unstable vessel growth, this can be addressed to different factors, such as its rapid diffusion, impaired biostability, and short half-live9.
However, there are good examples of studies that have demonstrated excellent results using bFGF as an angiogenic factor. Unger et al. made the most relevant study; their research aim was to determine if the administration of exogenous bFGF could accelerate myocardial angiogenesis and improve the collateral flow19. The model of the study were mongrel dogs with an induced occlusion made by a hydraulic balloon placed on the left circumflex coronary artery. Their results show an increase in the collateral flow in the affected zones and also an increase in cellular proliferation in areas of the scar. Also, they found that bFGF has vasodilator properties. Demonstrating that bFGF is a good prospect as a therapy for ischemic heart diseases, by enhancing collateral development19.
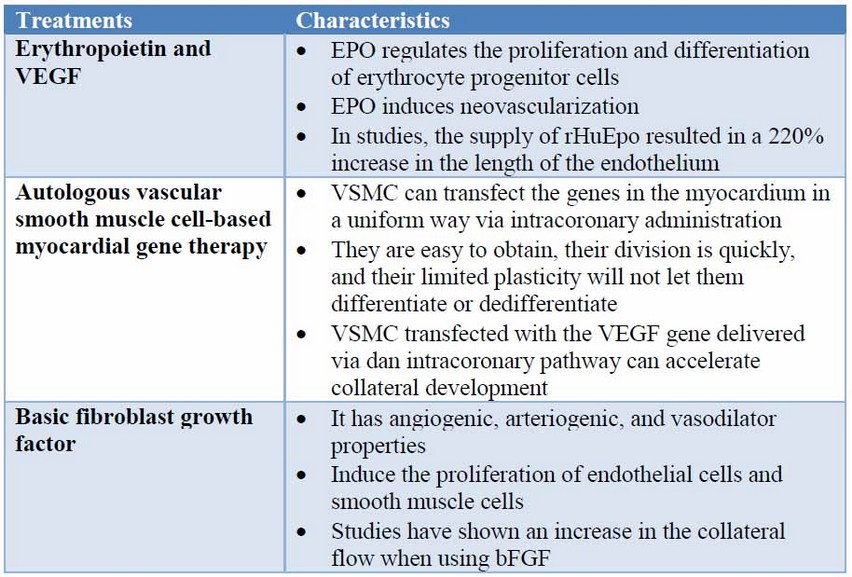
Table 1. Characteristics of the treatments
Monitoring method
Serum CXCL10 and CXCL12 chemokine levels
Inflammation influences the formation of atherosclerosis, and other diseases produced in the coronary arteries. In the first place, chemokines are inflammatory mediators which suppress certain biological functions, such as the migration of leukocytes with inflammatory signals. Based on the study of Vahid et al., they evaluate the potential correlation between serum levels of the chemokines (CXCL-10 and CXCL-12) and the degree of coronary stenosis, and also the degree of occlusion of the coronary artery. The processes of angiogenesis and angiostasis can be attributed to chemokines, which intervene in the development of collateral circulation20.
Chemokines are part of a subcategory of cytokines. Something to note about these proteins is that they are the first to transmigrate to infection, inflammation, and traumatic tissue injury sites21. Additionally, chemokines influence angiogenesis, initiation of the formation of new blood vessels, or angiostasis, inhibition of the formation of new blood vessels22. The mentioned chemokines CXCL-10 and CXCL-12 belonging to CXC, one of the four significant subclasses of chemokines, are an example of this23.
According to Vahid et al., there was an increase in CXCL-10 chemokines, such as CXCL-12 in men, which represents the interaction between the balance of angiogenesis, inflammation, and atherosclerosis20. It has been found that male hormones and globulin, through their impact on angiogenic CXCL-12, affect the pathogenesis of coronary artery diseases that induces the expression and production of chemokines mentioned24. Moreover, the older the person, the higher the risk of arterial calcification and rigidity. Also, it was determined that diabetes, endothelial and acute cell dysfunction contribute to vascular inflammation and the development of atherosclerotic coronary arteries and that chemokines possess antisclerotic functions25.
One of the striking findings in their study is the correlation between CXCL10 and CXCL12 chemokine concentrations and coronary artery occlusion. Where they found intense competition between these two chemokines and each chemokine increases in an attempt to influence the balance of angiogenesis/angiostasis20. It is worth mentioning that in other studies, cytokines such as TNF-α, IL-27, CXCL-8, and CRP play a role in the degree of occlusion of the coronary artery26.
Thus, if an equilibrium will be induced between the two chemokines, and the influence of the angiogenic chemokine was more significant than the angiostatic one, satisfactory results could be generated for the improvement and efficiency of these blood vessels.
DISCUSSION
Nowadays, one of the most significant challenges for future medicine is to search ways to treat coronary artery diseases, without the surgical intervention of implants like stents and grafts like the bypass, that do not necessarily ensure a long and reliable solution, as the aforementioned treatments come with risks like heart rhythm problems, blood clots, and many other problems27. Thus, the creation and implementation of reliable solutions are needed to improve the management of patients with artery coronary occlusions. It has been demonstrated that certain angiogenic factors, such as VEGF and bFGF, increase the collateral flow and formation, even enhance the cellular proliferation on the damaged zones by the occlusion. As well as that EPO is an angiogenic growth factor as it induces neovascularization. We have also to consider, the different ways of monitoring and control the angiogenic process, researchers have found two types of chemokine (CXCL10 and CXCL12) that by concentrations level it is possible to measure the grade of angiogenesis and angiostasis produced in areas of a coronary artery.
Even though there are strong pieces of evidence that these therapies using angiogenic factors are useful and have good results, there are still some issues that are needed to be addressed, like the optimal dose, time course, routes of administration. Also, the comprehension of the exact mechanism of how these factors work to correctly combine these components in a single complemented treatment between them is an issue.
CONCLUSION
Our review cites several research papers, in which various authors evaluate and demonstrate the different new techniques to treat and rehabilitate damages caused by occlusions on the coronary artery. All these treatments have shown good efficacy to treat the problem by increasing the collateral flow in the coronary arteries, and are suitable solutions to treat this problem on humans.
REFERENCES
1. European Heart Journal, Volume 34, Issue 39, 14 October 2013, Pages 3028–3034,https://doi.org/10.1093/eurheartj/eht356
2. Nadal, L. L., Cynamon, J., Lipsitz, E. C., & Bolia, A. (2004). Subintimal angioplasty for chronic arterial occlusions. Techniques in Vascular and Interventional Radiology, 7(1), 16–22.doi:10.1053/j.tvir.2004.01.008
3. Sianos G, Werner GS, Galassi AR, et al. Recanalisation of chronic total coronary occlusions: 2012 consensus document from the EuroCTO club. EuroIntervention. 2012;8:139–45
4. Park SJ et al. Drug-eluting stent versus optimal medical therapy in patients with coronary chronic total occlusion: DECISION CTO randomized trial. Abstract 405-15. American College of Cardiology 2017 Scientific Sessions, 17-19 March 2017.
5. Kahn JK, Hartzler GO. Retrograde coronary angioplasty of isolated arterial segments through saphenous vein bypass grafts. Cathet Cardiovasc Diagn. 1990;20(2):88-93.
6. Coronary Artery Bypass. Texas Heart Institute. https://www.texasheart.org/heart-health/heart-information-center/topics/coronary-artery-bypass/.
7. Coronary artery disease. Mayo Clinic 2018. https://www.mayoclinic.org/diseases-conditions/coronary-artery-disease/diagnosis-treatment/drc-20350619.
8. Chu H, Wang Y. Therapeutic angiogenesis: controlled delivery of angiogenic factors. Therapeutic Delivery 2012;3:693–714. doi:10.4155/tde.12.50.
9. Deveza L, Choi J, Yang F. Therapeutic Angiogenesis for Treating Cardiovascular Diseases. Theranostics 2012;2:801–14. doi:10.7150/thno.4419.
10. Jelkmann, W. (1994). Biology of erythropoietin. Clin. Invest. 72, S3–10.
11. Westenbrink B.D., Oeseburg H., Kleijn L., van der Harst P., Belonje A.M., Voors A.A., Schoemaker R.G., de Boer R.A., van Veldhuisen D.J., van Gilst W.H. Erythropoietin stimulates normal endothelial progenitor cell-mediated endothelial turnover but attributes to neovascularization only in the presence of local ischemia. Cardiovasc. Drugs Ther. 2008;22:265–274. doi: 10.1007/s10557-008-6094-y.
12. Westenbrink BD, Lipsic E, van der Meer P, van der HP, Oeseburg H, Du Marchie Sarvaas GJ, et al. erythropoietin improves cardiac function through endothelial progenitor cell and vascular endothelial growth factor-mediated neovascularization. Eur Heart J 2007; 28: 2018-27.
13. Jaquet K, Krause K, Tawakol-Khodai M, Geidel S, Kuck KH. Erythropoietin and VEGF exhibit equal angiogenic potential. Microvasc Res 2002; 64: 326-33.
14. Carlini, R. G., Reyes, A. A., and Rothstein, M. (1995). Recombinant human erythropoietin stimulates angiogenesis in vitro. Kidney Int. 47, 740–745.
15. Schaper W, Ito WD. Molecular Mechanisms of Coronary Collateral Vessel Growth. Circulation Research 1996;79:911–9. doi:10.1161/01.res.79.5.911.
16. Hattan N, Warltier D, Gu W, Kolz C, Chilian WM, Weihrauch D. Autologous vascular smooth muscle cell-based myocardial gene therapy to induce coronary collateral growth. American Journal of Physiology-Heart and Circulatory Physiology 2004;287. doi:10.1152/ajpheart.00145.2004.
17. Majesky MW. Vascular smooth muscle diversity: Insights from developmental biology. Current Atherosclerosis Reports 2003;5:208–13. doi:10.1007/s11883-003-0026-x.
18. Vale PR, Losordo DW, Symes JF, Isner JM. Growth factors for therapeutic angiogenesis in cardiovascular diseases. Rev Esp Cardiol 2001;54.
19. Unger EF, Banai S, Shou M, Lazarous DF, Jaklitsch MT, Scheinowitz M, et al. Basic fibroblast growth factor enhances myocardial collateral flow in a canine model. American Journal of Physiology-Heart and Circulatory Physiology 1994;266. doi:10.1152/ajpheart.1994.266.4.h1588.
20. Vahid Tavakolian Ferdousie, Maryam Mohammadi, Gholamhossein Hassanshahi, Hossein Khorramdelazad, Soudeh Khanamani Falahati-pour, Mohsen Mirzaei, Mohammad Allah Tavakoli, Zahra Kamiab, Zahra Ahmadi, Reza Vazirinejad, Effat Shahrabadi, Ioanna Koniari, Nicholas G Kounis, and Ali Esmaeili Nadimi, “Serum CXCL10 and CXCL12 chemokine levels are associated with the severity of coronary artery disease and coronary artery occlusion,” International Journal of Cardiology, vol. 233, pp. 23–28, 2017
21. G. Hassanshahi, S.S. Patel, A.A. Jafarzadeh, A.J. Dickson, Expression of CXC chemokine IP-10/Mob-1 by primary hepatocytes following heat shock, Saudi Med. J. 28 (2007) 514–518.
22. S. Singh, M. Varney, R.K. Singh, Host CXCR2-dependent regulation of melanoma growth, angiogenesis, and experimental lung metastasis, Cancer Res. 69 (2009) 411–415.
23. Z. Ahmadi, M.K. Arababadi, G. Hassanshahi, CXCL10 activities, biological structure, and source along with its significant role played in the pathophysiology of type I diabetes mellitus, Inflammation 36 (2013) 364–371.
24. W. Barud, A. Nasiłowska-Barud, J. Sobstyl, J. Mieczkowska, G.Wójcicka, J. Bełtowski, et al., Association of stromal-derived factor-1 alpha and endogenous sex hormones in men aged over 50 years with stable coronary artery disease, Adv. Med. Sci. 57 (2012) 322–327.
25. D. Milosz, L. Czupryniak, M. Saryusz-Wolska, G. Zasadzinska, A. Borkowska, E. Cieplucha, et al., Adiponectinemia, inflammatory process activity, and endothelial dysfunction in patients with type 2 diabetes and acute coronary syndrome with ST elevation in relation to the severity of lesions in the coronary arteries, Pol. Arch. Med. Wewn. 117 (2007) 343.
26. W. Jin, Y. Zhao, W. Yan, L. Cao, W. Zhang, M. Wang, et al., Elevated circulating interleukin-27 in patients with coronary artery disease is associated with dendritic cells, oxidized low-density lipoprotein, and severity of coronary artery stenosis, acMediat. Inflamm. 2012 (2012).
27. Benefits and Risks of Coronary Bypass Surgery. The Society for Cardiovascular Angiography and Interventions 2015. http://www.secondscount.org/heart-condition-centers/info-detail-2/benefits-risks-of-coronary-bypass-surgery-2#.XNtRjS2b5QI
Received: 17 April, 2019
Accepted: 23 May 2019
Sebastian Alcivar, Jonathan Hermenejildo
School of Biological Sciences and Engineering, Yachay Tech University
Corresponding author: [email protected]
