2024..01.01.3
Files > Conference Series > 2024 > Chimboazo ild pagina nueva
Anthropometric indicators and their relationship with body fat in obese women.
Yury Rosales-Ricardo1*, Vinicio Caiza-Ruiz2, Sonia Álvarez-Carrión3
1 Universidad Nacional de Chimborazo – Ecuador. Facultad de Ciencias de la Salud;Ecuador
2 Universidad Nacional de Chimborazo – Ecuador. Facultad de Ciencias de la Salud.;
3 Universidad Nacional de Chimborazo – Ecuador. Facultad de Ciencias de la Salud.;
* Correspondence: [email protected]
Available from. http://dx.doi.org/10.21931/BJ/2024.01.01.3
ABSTRACT
To determine the anthropometric indicator of best correlation with body fat in women with obesity aged 20 to 59 years. A correlational cross-sectional study was conducted. The percentage of body fat was determined (% GC) and lipid profile (LDL, TG, CT), Body Mass Index (BMI), Hip Waist Index (ICC), Waist Height Index (ICE), Conicity Index (CI), Body Adiposity Index (BSI), Hip Height Index (HSI) and Body Weight by Height Index (BWI). Seven hundred and eighty obese women were selected by random cluster sampling. The correlation of the mean % GC with anthropometric indicators was: BMI:0.697, ICC: 0.661, ECI: 0.910, CI: 0.587, ICadE: 0.323, CAI: 0.578, EICP: 0.549. The lipid profile correlation with anthropometric variables and indices was: LDL (BMI: 0.615, ICC: 0.765, ECI: 0.881, CSI: 0.535, ICadE: 0.588, ECDI: 0.492), TG (BMI: 0.690, ICC: 0.776, ICE: 0.855, CI:0.625, CI: 0.572, CIadE: 0.632, EICP: 0.631) Y TC (BMI: 0.699, ICC: 0.715, ECI: 0.829, CI: 0.601, ACI: 0.609, CIadE: 0.709, EICP: 0.500) High correlation between % GC and Waist Circumference. Waist Height Index had a better correlation with Body Fat.
Keywords: obesity; health; women; nutritional status
INTRODUCTION
A country's entire production and service capacity rests on working-age adults. That is why the nutritional evaluation of this group, whose social importance is indisputable, acquires excellent relevance in the study of any population from the point of view of their health status. Anthropometry, an easy-to-apply, inexpensive and non-invasive procedure, has been widely used to estimate nutritional status from a clinical and epidemiological point of view.
The incorporation of women into work, their participation in the economic development of the country and their leading role in the support and development of the family mean that, from a social and financial point of view, their medical attention should be ensured so that the biological changes produced by the decrease in estrogen production in their organism do not turn this transition stage into a disease, for which these women should receive comprehensive medical attention.
Obesity in women has peculiar nuances that are beginning to be understood. The higher prevalence of obesity in women is a product of biological and psychological characteristics, as well as social situations. Pregnancy and menopause favor obesity. Women have a higher prevalence of eating disorders. In addition, the "obesogenic" environment may have a more significant effect on women because the portions they eat are usually greater than their needs 1.
According to the World Health Organization (WHO) 2, obesity is the most prevalent chronic non-communicable disease in the world, which is why it is called "The Epidemic of the 21st Century". Over 3 billion adults were overweight in 2016, 39% of persons (39% of males and 40% of women). In total, 11% of men and 15% of women in the adult population of the world were obese in 2016 2.
According to the latest concept issued by WHO, obesity is defined as an abnormal or excessive accumulation of fat 2, i.e., describing this as a body weight above values considered normal for height would be incorrect and would depart from the genuine concept of obesity, as body fat is only one component of total body weight.
The indicator used and validated to evaluate obesity in adults is the Body Mass Index (BMI). However, this has several difficulties in the sense that what it considers is overweight and not obesity. On the other hand, other indicators such as waist circumference (WC) and waist height index (WHI) 3 have been less studied in these populations. The EWI in Asian studies (in adults from China) 4 is a better indicator of coronary risk factors, dyslipidemia and type 2 diabetes than other anthropometric indicators such as BMI, WC and waist-hip index in some epidemiological studies 4 - 9. The results indicated that the EWI could be an optimal anthropometric predictor of metabolic syndrome risk factors. Other less-used indexes at the international level, such as the Conicity Index 10 or the Body Adiposity Index 11, have reported good results.
Therefore, this study aimed to determine the anthropometric indicator with the best correlation with body fatness in obese women aged 20 to 59.
MATERIALS AND METHODS
Cross-sectional correlational study to determine the relationship between body fat percentile (using three anthropometric methods in isolation and the mean of these) and lipid profile (LDL, TC, TAG) and other existing anthropometric indicators such as Body Mass Index, Waist Circumference, Hip Circumference, Body Weight, Waist Hip Index, Hip Height Index, Taper Index, Conicity Index, Body Weight, Hip Hip Height Index, Hip Height Index, Hip Height Index, Hip Taper Index, Hip Conicity Index and Body Weight, Waist Circumference, Hip Circumference, Body Weight, Waist Hip Index, Hip Height Index, Conicity Index, Body Adiposity Index, based on the correct WHO definition of obesity.
For this purpose, 780 women with obesity were selected using random sampling by clusters. The first conglomerate was the 320 clinics in the 10 health areas of Holguin, Cuba. From there, 20% of these (64 clinics) were selected by simple random sampling. From each clinic, one out of every ten patients with these research characteristics was determined by systematic random sampling. Of these 780 patients, 55 did not present themselves, for a 7 % loss, and another 35 were no longer obese or pre-obese when they introduced themselves or did not want to donate their data to the study, for a 4.4 % loss, which represented a total loss of 11.4 % (90 patients). The final sample consisted of 690 female patients between 20 and 59 years of age with obesity from the 10 health areas of the municipality of Holguín, Cuba. In the consultation of health promotion and physical development of the Provincial Center of Sports Medicine of Holguin, 30 patients were attended weekly, two days per week for 26 weeks.
Anthropometric measurements were performed by an anthropometric technician level II of the International Society for the Advancement of Kineanthropometry (ISAK). Body weight was determined using a previously calibrated electronic scale with a sensitivity of up to 0.1 kg, and height was measured utilizing a stadiometer with a sensitivity of 0.1 cm. A Harpenden caliper with a sensitivity of 0.1 mm and a pressure of 10 mm2 was always used for the triplicate evaluation of the 4 skinfolds (tricipital, bicipital, subscapular and suprailiac muscles). The percent body fat was assessed by first estimating the Body Density using the Durnin-Womersley formula for women between 16 and 72 years of age (measurement of the bicipital, tricipital, subscapular and suprascapular skinfolds) and then taking this result to the Siri equation to determine the fat percentages. All measurements were performed in triplicate in a non-consecutive manner and using the median as the final value 12.
The lipid profile was found in the clinical area of the Center in conjunction with the Department of Clinical Bioanalysis of the University of Medical Sciences of Holguin.
The author of the research carried out the surveys.
Measurements were taken for both studies (according to the methodology of the International Society for the Development of Cineanthropometry, ISAK) 15:
The sequence of measurements used:
1. Body weight (BW) in kg.
2. Height (E) in meters
3. Waist circumference (WC) in cm.
4. Circumference of the hip (CCad) in cm.
5. Biceps crease (Pb) in mm.
6. Triceps crease (Pt) in mm.
7. Subscapularis crease (Pse) in mm.
8. Suprailiac crease (Psi) in mm.
Other variables considered:
1- Age in years
2- Associated pathologies
To determine the type of causal obesity (exogenous or endogenous), we used the determination of the possible associated pathologies that could have caused the obesity in the clinical consultation of the Center using the methodology of the SEEDO 12, 15.
It was essential to identify the medications taken by the patient, with particular emphasis on determining the intake of drugs associated with an increase in weight, such as insulin, sulfonylureas, methyglinides, thiazolidinediones, phenothiazines, tricyclic antidepressants, certain antipsychotics, glucocorticoids, megestrol acetate, estrogens, antiepileptics such as valproate and carbamazepine, cyproheptadine and beta-blockers. This suggested the presence of endogenous obesity 12, 15.
From the results of these variables, the following indexes were found:
1- Percent body fat (%BF).
Three methods found this:
A) The above four skinfolds were measured to estimate body density (D) and from there, the percent body fat (%BF) with the Durnin-Womersley and Siri equation, respectively, for the female population of working age (18 to 59 years) for adult Cuban population 16:
D = 1.1567 - 0.0717 * log10 (Pt + Pb + Pse + Psi) (1)
% GC= (5.03 / D) - 4.59
B) Weltman's formula for obese women aged 20 to 60 years 13, 16:
% GC= 0.11077 * CC - 0.17666 * E + 0.14354 * PC + 51.033.
C) Lean's more accurate formula for women aged 18 to 83 years 14, 16:
% GC= 0.232 * CC + 0.657 * Pt + 0.215 * Age - 5.5
In addition to the individual result of each one, the average of the three values was also found to determine the fat percentages and their correlation with the anthropometric indexes that are exposed below much more efficiently:
1- Body Mass Index (BMI)
BMI= WC / E2
2- Waist Hip Index (ICC)
ICC= CC / CCad
3- Height Waist Height Index (ICE)
ICE= CC / E
4- Conicity Index (CI) 17
CI= CC / (0.109 √ PC / E)
5- Body Adiposity Index (BAI) 18
BCI= ([CCad]/[E]1.5-18)
6- Hip Height Index (ICadE)
ICadE= CCad / E
Index proposed by the author
The venous blood samples to determine the laboratory variables were taken after an overnight fast of 12-14 hours, and low-lipid diets were processed in duplicate, not exceeding 5% of the variation coefficient. The reagents of national production (Finlay laboratories): total cholesterol (TC): Colestest reagent; triglycerides (TG): Triglitest reagent and low-density lipoproteins (LDL) according to Friedewald's formula (LDL= CT- (HDL + TG * 5).
The results of PC, CC, CCad, BMI, ICC, IAC, IC, ICadE and ICE were correlated with the %GC in their three results, the mean of these three values, and the lipid profile.
The mean (X) and standard deviation (SD) were used for the parametric statistical analysis. The Spearman correlation coefficient was employed to study the level of correlation between variables. A 95% confidence interval was used.
The objectives and procedures of the study were explained in detail to all the participants, and they were provided with the necessary information for their knowledge. In addition, so that they could answer correctly, the interview was carried out as long as the patients expressed their informed consent to participate in the research and also agreed to answer questions involving the sexuality of the couple. This was a research project cited in the no-risk research category.
RESULTS
The final sample of 690 women diagnosed with obesity in all health areas of Holguín municipality, aged between 20 and 59 years, is shown in Table 1.
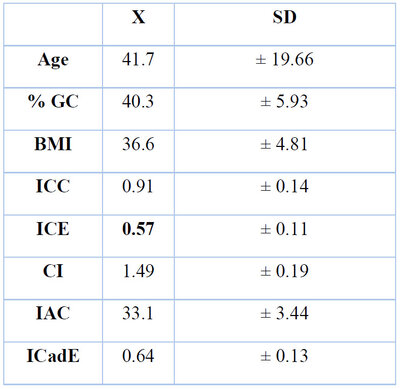
P <0.05
Table 1. Descriptive statistics of the study variables.
In women with obesity, there is a high correlation between Body Fat and Waist Circumference, with a somewhat lower correlation between the former and Body Weight and Height. On the other hand, there is a low correlation with Hip Circumference and Age (Table 2).
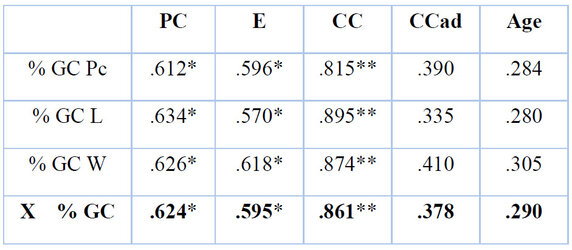
P <0.05
Table 2. Correlation of the variables with the % CG. Total sample (n= 690).
Legend: %BF Pc: percent body fat calculated using skinfolds; %BF L: percent body fat using the Lean equation (21); %BF W: percent body fat calculated using the Weltman equation(5); X %BF: mean of the three results; BW: body weight (kg); E: height (meters); WC: waist circumference or circumference (cm); HC: waist circumference or circumference (cm); HCad: hip circumference or circumference (cm). Degrees of correlation: **: highly significant (.750 - 1); *: significant (.500 - .749).
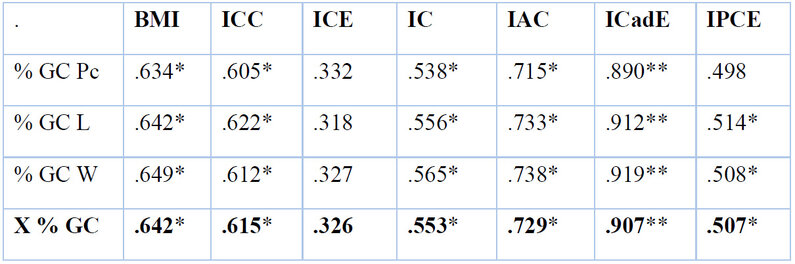
The Height-Waist Index was the best correlated with Body Fat in the whole population studied, much higher than other validated and much more used indexes (Table 3).
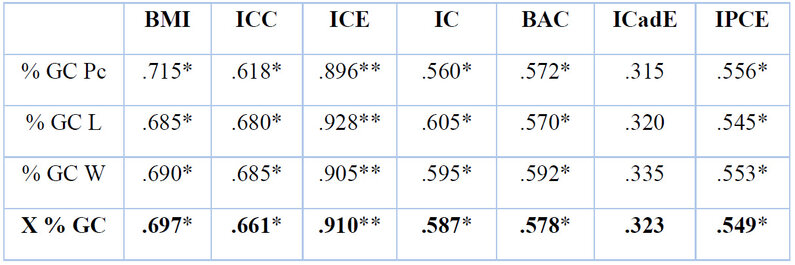
P <0.05
Table 3. Correlations between anthropometric indices and %GC. Total sample (n= 690).
In women with android obesity, the variable that correlated best with Body Fat was by far Waist Circumference. The index was Waist Height (Table 4).
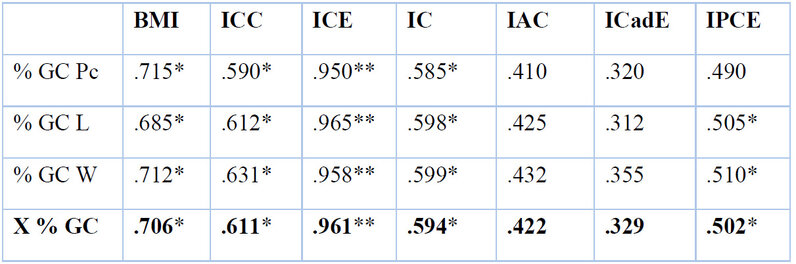
P<0.05
Table 4. Index correlations with %GC in obese android women (n=587).
Table 4. Index correlations with %GC in obese android women (n=587).
In women with gynecoid obesity, on the other hand, the variable with the best correlation with Body Fat was Hip Circumference and the index was Hip Height, as proposed by the author. (Table 5).
.
P<0.05
Table 5. Index correlations with %GC in obese gynaecoid women (n=103).
As for the lipid profile, the highest correlations with this were found in the Waist Hip Index, Waist Circumference, Waist Hip Index, Body Mass Index, Hip Height Index and Taper Index in that order (Table 6).
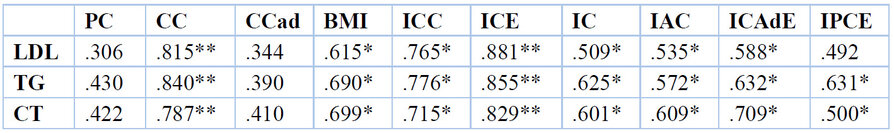
P<0.05
Table 6. Correlation of lipid profile with anthropometric variables and indices. Total sample (n= 690)
DISCUSSION
The main objective of this study was to determine the anthropometric indicator with the best correlation with body fat in obese women aged 20 to 59 years. Skinfolds, present in most studies on body composition as a comparison technique, show a high concordance or correlation with %BF obtained through various techniques such as densitometry, dilutional methods and bioelectrical impedance, which, together with its cost and accessibility, justifies its wide use in this type of studies and can be considered as the gold standard among anthropometric measurements. The Spanish Society for the Study of Obesity (SEEDO) recommends the use of skinfolds and the Siri equation for the assessment of body fat percentage, considering both the global and the specific way of calculating body density with the Durnin-Womersley equation to be valid 19.
This can be seen in a critical study in Brazil where the relationship between anthropometric markers of fat distribution and body fat as measured by bioelectrical impedance or the total number of skinfolds was assessed in 262 women. The body fat determined by skinfold summation and bioelectrical impedance were comparable. The thicknesses of body fat measured by bioelectrical impedance and those calculated by the sum of skinfolds, waist circumference, and waist-to-height ratio were strongly correlated. As for the taper index, a weak correlation was observed for women; the results were similar in our study 20.
Regarding the current research, similar results have been observed in other studies, as shown in Oliveira et al.21 men had higher BMI, WC, and WHR, whereas women had higher %BF (p 0.001). Males had a greater proportion of changed RCC and %GC for LDL-c and TC. There was a link between BMI and CC (r = 0.97 for men and 0.95 for women; p 0.001). The best association (p 0.001) in men was between CC and CCR (r = 0.82), and in women, it was %GC as well as CC (r = 0.80). Triglycerides (TG) were found to be connected to CC (male: r = 0.992; female: r = 0.95; p 0.001), as well as to CC (male: r = 0.82; female: r = 0.79; p 0.001). In several analyses, BMI was associated with total cholesterol (p = 0.051) in males and weakly associated with TG/HDL-cholesterol (p = 0.062) in females.
In a study conducted in Pernambuco, Brazil,22, the diagnosis of MS was found in 65.3% of the patients. There were 81.3% who were inactive and 37.4% who were overweight in 28% of the patients. HOMA-IR and sagittal abdominal diameter (SAD) (p = 0.016), body mass index (p = 0.040), and body fat % (p = 0.016) were found to be correlated. The DAS was the anthropometric indicator that presented the best correlation with IR in hospitalized patients with coronary artery disease.
Another study included a sample of 105 workers. The following were operationalized as clinical variables: abdominal waist measurement, body mass index, skin fold, blood pressure and lipid profile. Pearson's correlation coefficient was calculated with a 95% confidence interval. The results showed a slight increase in total cholesterol in males at the expense of HDL cholesterol, with no changes in the other variables. A higher susceptibility to cardiometabolic risk was seen in non-obese people. There was insufficient concordance with our investigation since the fat mass index did not significantly correlate with the other anthropometric measures. Individuals with a changed abdominal circumference and the metabolic syndrome diagnostic criteria are closely related. 23.
Domínguez-Reyes et al.24 evaluated anthropometric measures in a Mexican adult; after abdominal obesity in women, hypertriglyceridemia was the metabolic risk factor with the highest prevalence, followed by hyperglycemia, hypercholesterolemia and high blood pressure, which were more common in men, even though abdominal obesity was more common in women. Waist circumference was the best predictor for presenting one or more metabolic risk factors [area under the curve ABC = 0.85 (95% CI, 0.78-0.92)], followed by BMI [ABC = 0.79 (95% CI, 0.72-0.88)] and finally ICC [ABC = 0.63 (95% CI, 0.52-0.74)]. In addition, it was observed that abdominal obesity doubles the risk of presenting metabolic syndrome. In a different study, the waist-to-height ratio (WHI) was the predictor variable with the highest adjusted OR (7.1 [4.3-11.6]) and the highest area under the curve (0.954 [0.928-0.979]); from an overall cut-off value for discriminating obesity of 0.507, it achieved a sensitivity of 90% and a specificity of 90%, has been an excellent predictor of obesity in children 25.
In other studies, the correlations were: BMI: body fat (0.70) very coincident with our study (0.697), waist (0.70), ICCad (0.48), ICT (0.72); ICCad: body fat (0.38), waist (0.69), endomorphy (0.39), mesomorphy (0.38); ICT: body fat (0.50) slightly different with ours (0.661) and waist (0.96); taper: waist (0.85), ICCad (0.58), ICT (0.85). The indicator with the poorest relationship between obesity and body mass index does not distinguish between different body parts. The waist-hip index presents a high prevalence but a weak relationship with body composition at risk. The waist-height index reflects a distribution of body volume. It suggests the best correlations with the body components at risk, being the most prevalent and adequate index to explain the biological risk associated with myocardial infarction 26.
The main strength of the present study is the quality of its methodology: the use of measurement protocols that were carried out according to the methods of the International Society for the Development of Kineanthropometry (ISAK) and SEEDO to perform the measurements and hence the realization of the respective anthropometric indicators. An ISAK level II anthropometric technician performed the anthropometric measurements. In addition, the sample used was probabilistic, using random cluster sampling, representative of the population.
Despite its strengths, some issues related to our studies deserve attention. It was impossible to measure body fat percentages using the international gold standard measures that would have given greater accuracy in correlation levels with the double indirect anthropometric indicators used. Furthermore, it was not possible to work with populations from other provinces of the country.
CONCLUSIONS
Therefore, it can be concluded that, in women with obesity, in general, there is a high correlation between Body Fat and Waist Circumference. The Waist Height Index was the one that correlated best with Body Fat over the other most commonly used indexes. In women with android obesity, the variable that best correlated with Body Fat was Waist Circumference, and the index was the Waist Height Index. In women with gynecoid obesity, the variable with the best correlation with Body Fat was Hip Circumference, and the index was Hip Height, as proposed by the author. With lipid profile, the highest correlations were found in the Waist Hip Index, Waist Circumference, Waist Hip Index, Body Mass Index, Hip Height Index and Conicity Index.
Author Contributions: A short paragraph specifying their contributions must be provided for research articles with several authors. The following statements should be used "Conceptualization, YRR; methodology, YRR, VCR, SAC; software, YRR; validation, YRR; formal analysis: YRR, VCR, SAC; investigation, YRR, VCR, SAC; resources, YRR; data curation, YRR; writing—original draft preparation, YRR; writing—review and editing, YRR, VCR, SAC; visualization, YRR; supervision, YRR; project administration, YRR; funding acquisition, YRR All authors have read and agreed to the published version of the manuscript." Please turn to the CRediT taxonomy for the term explanation. Authorship must be limited to those who have contributed substantially to the work reported.
Funding: "This research received no external funding."
Institutional Review Board Statement: "Not applicable."
Informed Consent Statement: "Not applicable."
Conflicts of Interest: "The authors declare no conflict of interest."
REFERENCES
1. Cano, E. R., Recio, G. M., Saldaña, M. R., Fernández, C. Á., Reyes, A. H., & Luque, R. M. (2020). Comparación de índices antropométricos, clásicos y nuevos, para el cribado de Síndrome Metabólico en población adulta laboral. Revista española de salud pública. 2020; (94), 83.
2. Obesidad y sobrepeso [Internet]. Who.int. [citado el 22 de enero de 2023]. Disponible en: https://www.who.int/es/news-room/fact-sheets/detail/obesity-and-overweight
3. Hsieh T. The waist and height ratio as a simple anthropometric index to identify metabolic risk. Internac J of Obesit. 2003; 27(5): 610-616
4. Shao J, Yu L. Waist-to-Height Ratio, an Optimal Predictor for Obesity and Metabolic Syndrome in Chinese Adults. J Nutr Health Aging. 2010; 14(9):782-5.
5. Ashwell M, Gibson S Waist-to-height ratio as an indicator of 'early health risk': simpler and more predictive than using a 'matrix' based on BMI and waist circumference BMJ Open 2016;6: e010159. doi: 10.1136/bmjopen-2015-010159
6. Sardinha LB, Santos DA, Silva AM, Grøntved A, Andersen LB. A Comparison between BMI, Waist Circumference, and Waist-To-Height Ratio for Identifying Cardio-Metabolic Risk in Children and Adolescents. PLOS ONE. 2016; 11(2): e0149351. https://doi.org/10.1371/journal.pone.0149351
7. Hou X, Chen S, Hu G, Chen P, Wu J, Ma X, Jia W. Stronger associations of waist circumference and waist-to-height ratio with diabetes than BMI in Chinese adults. Diabetes research and clinical practice. 2019; 147:9-18.
8. A Rodrigues, L Mascarenhas, A Gama, I Mourão, H Nogueira, V Rosado, C Padez, Waist-to-height ratio and its association with sedentary behaviour in a sample of Portuguese male children, European Journal of Public Health, 2019; 29(1) ckz035.026, https://doi.org/10.1093/eurpub/ckz035.026
9. Lam BCC, Koh GCH, Chen C, Wong MTK, Fallows SJ. Comparison of Body Mass Index (BMI), Body Adiposity Index (BAI), Waist Circumference (WC), Waist-To-Hip Ratio (WHR) and Waist-To-Height Ratio (WHtR) as Predictors of Cardiovascular Disease Risk Factors in an Adult Population in Singapore. PLOS ONE. 2015; 10(4): e0122985. https://doi.org/10.1371/journal.pone.0122985
10. Rachael W Taylor, Ianthe E Jones, Sheila M Williams, Ailsa Goulding, Evaluation of waist circumference, waist-to-hip ratio, and the conicity index as screening tools for high trunk fat mass, as measured by dual-energy X-ray absorptiometry, in children aged 3–19. The American Journal of Clinical Nutrition, 2000; 72(2): 490–495, https://doi.org/10.1093/ajcn/72.2.490
11. Bergman, R. N., Stefanovski, D., Buchanan, T. A., Sumner, A. E., Reynolds, J. C., Sebring, N. G., Xiang, A. H. and Watanabe, R. M. A Better Index of Body Adiposity. Obesity. 2011; 19: 1083-1089. doi:10.1038/oby.2011.38
12. Lecube A, Monereo S, Rubio MÁ, Martínez-de-Icaya P, Martí A, Salvador J, Masmiquel L, Goday A, Bellido D, Lurbe E, García-Almeida JM, Tinahones FJ, García-Luna PP, Palacio E, Gargallo M, Bretón I, Morales-Conde S, Caixàs A, Menéndez E, Puig-Domingo M, Casanueva FF. Prevention, diagnosis, and treatment of obesity. 2016 position statement of the Spanish Society for the Study of Obesity. Endocrinol Diabetes Nutr. 2017 Mar;64 (1):15-22.
13. Cándido A. P. C., Alosta J. P. S., Oliveira C. T., Freitas R. N., Freitas S. N., Machado-Coelho G. L. L.. Anthropometric methods for obesity screening in schoolchildren: the Ouro Preto Study. Nutr. Hosp. 2012 Feb [citado 2018 Jul 05] ; 27(1): 146-153.
14. Lean, EJ. Waist circumference as a measure for indicating need for weight management, BMJ, 1995; 311:158-161.
15. Ferreyro, F., Esparza, F. y Jones, M., Eds. Kinanthropometry XV. International Society for the Advancement of Kinanthopometry Conference. World Conference in Knanthropometry and Body Composition ISAK-UADY 2016, Ediciones de la Universidad Autónoma de Yucatán, Mérida, Mexico. 284 p.
16. Carvajal W, Deturnel Y, Echevarría I, Martínez M, Castillo ME. Protocolo de valoración de la composición corporal para el control cineantropométrico del entrenamiento deportivo. Documento de consenso del Departamento de Cineantropometría del Instituto de Medicina del Deporte de Cuba. Revista. Cubana de. Medicina del. Deporte y la Cultura. Física 2010; 5(3).
17. Valdez R, Seidell JC, Ahn YI, Weiss KM. A new index of abdominal adiposity as an indicator of risk for cardiovascular disease. A cross-population study. Int J Obes Relat Metab Disord. 1993 Feb;17(2):77-82.
18. Bergman RN, Stefanovski D, Buchanan TA, Sumner AE, Reynolds JC, Sebring NG, Xiang AH, Watanabe RM. A better index of body adiposity. Obesity (Silver Spring). 2011 May; 19(5):1083-9
19. Martín Moreno Vicente, Gómez Gandoy Juan Benito, Antoranz González María Jesús. Medición de la grasa corporal mediante impedancia bioeléctrica, pliegues cutáneos y ecuaciones a partir de medidas antropométricas. Análisis comparativo. Rev. Esp. Salud Publica . 2001 Mayo; 75(3): 221-236.
20. Diniz-Araujo. Evaluación de la grasa corporal por impedancia bioeléctrica y su correlación con indicadores antropométricos. Nutr. Hosp. 2012; 27(6)
21. Oliveira M, Arruda M, Fagundes R, Martins L, Moreira E, Trindade E. Relación de indicadores antropométricos con factores de riesgo para enfermedad cardiovascular. Arq. Bras. Cardiol. 2010 Ap; 94( 4 ): 478-485.
22. Pessoa L, Araújo Tavares CM, Freire Clementino MC, Freire Lustosa M, Batista RA, Calado Brito D. Asociación de los indicadores antropométricos y de composición corporal en la predicción de la resistencia a la insulina en pacientes con enfermedad de las arterias coronarias. Nutr. Hosp. 2016 Ago; 33( 4 ): 825-831.
23. Cedeño Morales R, Castellanos González M, Benet Rodríguez M, Mass Sosa L, Mora Hernández C, Parada Arias JC. Indicadores antropométricos para determinar la obesidad, y sus relaciones con el riesgo cardiometabólico. Revista Finlay; 2015; 5(1): 12-23
24. Domínguez-Reyes T, Quiroz-Vargas I, Salgado-Bernabé AB, Salgado-Goytia L, Muñoz-Valle JF, Parra-Rojas I. Las medidas antropométricas como indicadores predictivos de riesgo metabólico en una población mexicana. Nutr. Hosp. 2017 Feb; 34(1):96-101. Disponible en: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0212-16112017000100015&lng=es. http://dx.doi.org/10.20960/nh.983.
25. Vaquero-Álvarez M, Romero-Saldaña M, Valle-Alonso F, Llorente J, Cantarero. Estudio de la obesidad en una población infantil rural y su relación con variables antropométricas. Atención Primaria;2019; 51 (6): 341-349
26. Martín-Castellanos A, Cabañas MD, Martín P, Barca FJ. The body composition in myocardial infarction males. Novel findings in both the association and relationship between anthropometric indicators of risk. JONNPR. 2017;2(9):388-398. DOI: 10.19230/jonnpr.1547
Received: 9 October 2023/ Accepted: 15 January 2024 / Published:15 February 2024
Citation. Rosales-Ricardo Y, Caiza-Ruiz V, Álvarez-Carrión S. Anthropometric indicators and their relationship with body fat in obese women. Revis Bionatura 2024; 1 (1) 3. http://dx.doi.org/10.21931/BJ/2024.01.01.3
Additional information Correspondence should be addressed to [email protected]
Peer review information. Bionatura thanks anonymous reviewer(s) for their contribution to the peer review of this work using https://reviewerlocator.webofscience.com/
All articles published by Bionatura Journal are made freely and permanently accessible online immediately upon publication, without subscription charges or registration barriers.
Publisher's Note: Bionatura Journal stays neutral concerning jurisdictional claims in published maps and institutional affiliations.
Copyright: © 2024 by the authors. They were submitted for possible open-access publication under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
